Orthopedic surgeons at The Mount Sinai Hospital became the first in the New York
metropolitan area to use augmented reality (AR) for a total hip replacement. Used by Brett
L. Hayden, MD, to complete an anterior total hip arthroplasty, this innovative technology gives surgeons X-ray-like vision and—during the surgery—allowed for Dr. Hayden and his team to employ enhanced alignment and placement of the acetabular component.
“The intraoperative use of augmented reality provides a much better sense of the patient’s
anatomy,” says Dr. Hayden, who completed the total hip arthroplasty on a patient who had a previous revision for dislocation on one side and osteonecrosis on the other.
The AR system works by projecting holograms onto special “smart” glasses loaded with AR
software. This enables the surgeon to see the anatomy, instruments, and joint implant inside the patient with three-dimensional clarity.
He notes, “Not only was it very easy to use, it was seamlessly integrated with my standard hip replacements.”

Dr. Hayden and team performing direct anterior total hip replacement.

Surgical instruments used for an augmented reality hip replacement
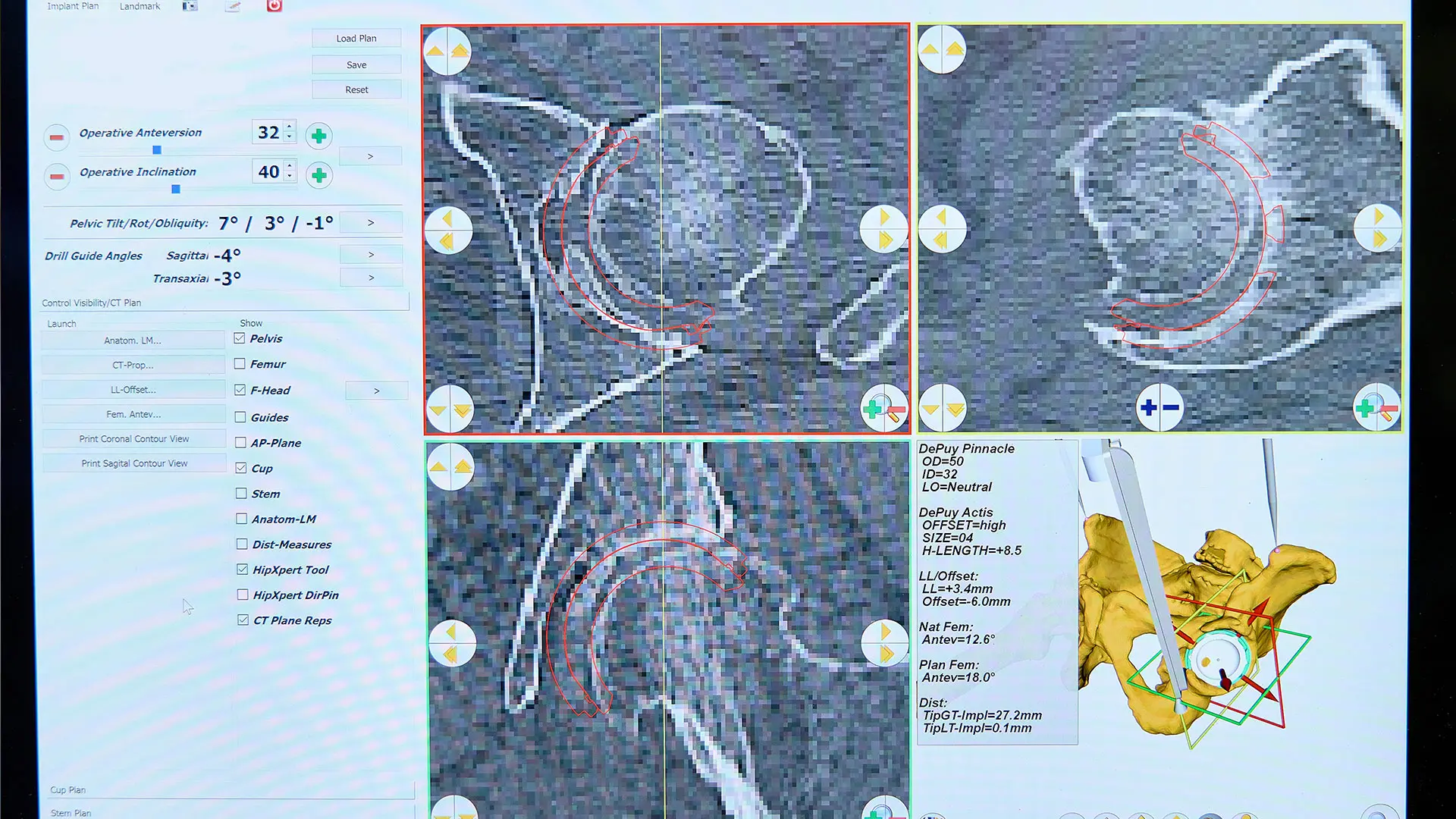
CT based, three-dimensional patient specific plan for total hip replacement

Dr. Hayden and team performing direct anterior total hip replacement with augmented reality glasses.
Cleared by the United States Food and Drug Administration in February 2021, AR technology is designed as an alternative to robotic systems, characterized by bulky workstations, cameras, and screens, with low-profile systems that no longer require the surgeon to constantly look back and forth between patient and monitor. Instead, 3D holograms now fill the surgeon’s field of vision with more data and information than was previously possible. Specifically, augmented reality digitally overlays the preoperative CT scan and detailed surgical reconstruction plan on top of the patient’s anatomy as seen real-time by the surgeon via tracking and registration technologies. This capability allows for accurate alignment and placement of the implant.
“The AR software allows the surgeon to effectively compare the CT scan to what they’re actually seeing inside the patient,” explains Dr. Hayden, who is Assistant Professor of Orthopedic Surgery at the Icahn School of Medicine at Mount Sinai. “That lets you know the fidelity of the registration and if the 3D plan is correctly aligned.”
In addition to increased precision, Dr. Hayden believes the technology could lead to quicker surgeries because the need for intraoperative X-ray or fluoroscopy—the two-dimensional standard for the field—would be reduced.
Where AR could have its greatest impact, Dr. Hayden adds, is in joint replacement patients at the highest risk for dislocation. This population includes individuals with stiff spines, a history of lumbar spine fusion or severe arthritis in the lumbar spine, or patients with osteonecrosis. The use of augmented reality has the potential to allow for more exact placement within the narrower “safe zone” of these complex cases. Another prime audience for the high-tech procedure could be patients undergoing revision hip replacement.
“In light of their altered anatomies and potential for bony defects, it would be very helpful for the surgeon to understand, based on the CT scan and 3D reconstruction plan, where all the intact bone is for component placement, as well as for screw positioning,” says Dr. Hayden.
Based on the success of his maiden procedure, Dr. Hayden is convinced AR could be a game-changer.
“The accuracy and precision it allows could help avoid surgical complications such as malpositioning and dislocations,” he says. “Additionally, the technology could be a valuable training tool since it allows others to learn the technique remotely by seeing it vividly through my eyes. While new, the system is very promising.”
Featured

Brett L. Hayden, MD
Assistant Professor Orthopedic Surgery
