Mount Sinai orthopedic surgeon Douglas B. Unis, MD, and his colleagues are steering the high-tech future of joint reconstruction. Led by Dr. Unis, the team is developing technology designed to offer patients personalized joint implants by carefully integrating 3-D printing, advanced robotics, and artificial intelligence (AI). The platform for this effort is Monogram Orthopedics, a company founded in 2016 by Dr. Unis, Sulaiman Somani, MD, and Anthony B. Costa, PhD, with funding from a National Institutes of Health (NIH) grant and ongoing support from the Icahn School of Medicine at Mount Sinai that will help the team launch clinical trials and secure approval from the U.S. Food and Drug Administration.
The robotics-driven orthopedic solution will initially focus on hip and knee replacements.

Monogram Robotic System in the operating room SOURCE: Monogram Orthopedics
“Leveraging state-of-the-art manufacturing methods and 3-D printing will allow us to efficiently deliver highly personalized implants at scale,” says Dr. Unis, who is Associate Professor of Orthopedics at the Icahn School of Medicine and Chief of Advanced Technology for Hip and Knee Replacement at Mount Sinai West. “By designing for optimized contact, we can create smaller implants that offer equivalent, or even superior, stability and improved physiological loading. We will be able to restore the center and axis of rotation with a high degree of accuracy because the implants will be designed for each patient and inserted with high-accuracy robotics.”
The reconstruction process starts with high-resolution CT scans that capture 0.625-millimeter slices. These images will provide the input needed to generate the implants and “cut paths” to help the surgeon visualize the surgical site. Raw 3-D imaging is then converted into “smart” computer-aided design (CAD) models, using computer vision techniques, including shape modeling and AI. Through AI, the system will efficiently analyze the scan and identify key anatomical landmarks and features to inform implant design and robotic execution.
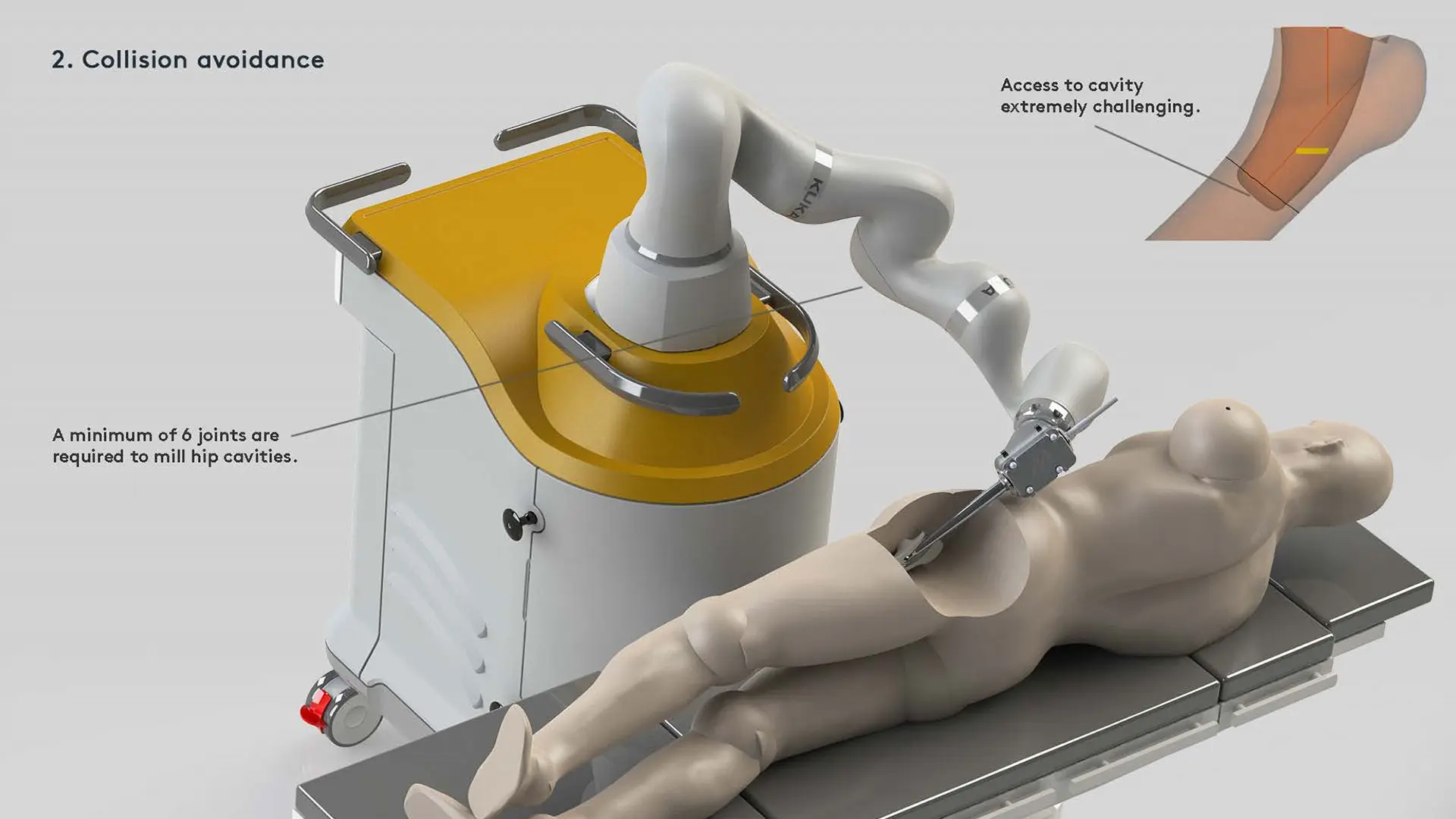
Closer examination of Monogram Robotic System SOURCE: Monogram Orthopedics
Drawing on this precise anatomical data, a customized implant is created out of medical grade titanium alloy using a direct metal laser sintering (DMLS) 3-D printer. “This customization is essential because, as technology improves, more patients in their 40s are getting hip and knee replacements,” explains Dr. Unis. “This makes fine-tuning these implants to match individual anatomy essential since younger patients typically put a greater load on implants over their lifetimes.”
Optimizing the Surgical Plan to Facilitate Superior Outcomes
The sophisticated technology being developed promises to enhance orthopedic surgery by running the surgical plan through an optimization and simulation engine to ensure the cuts are executed as safely and efficiently as possible. Rather than relying solely on a preoperative surgical plan, according to Dr. Unis, the system will leverage the robot’s kinematic redundancy to allow for intraoperative obstacle avoidance and real-time tissue tracking. “With the ability to simultaneously track six objects in real time, the system will allow for the integration of ‘smart tools’ into the surgical theater,” he says. “What was once an ordinary retractor is now a virtual boundary.”
The overarching goal of Dr. Unis and his colleagues is to address major clinical concerns through their platform, including cost, time, and a lack of control or real-time adjustment. The system’s software, for example, constantly reoptimizes to maximize efficiency in real-world scenarios. Moreover, rather than rely on conventional, cart-based optical navigation, the developers are exploring robot-mounted camera systems that eliminate line-of-sight issues and reduce cost and portability challenges.
They have taken into consideration the fact that 50 percent of early revision total knee arthroplasties are related to instability, malalignment or malposition, or failure of fixation. Preoperative planning and surgical robotics can thus address these primary modes of failure. More specifically, robotics can help prepare high-accuracy contoured cavities that mitigate the risk of poor placement, fracture, or subsidence.
“Ultimately, our system builds on fundamentally good surgical procedures,” emphasizes Dr. Unis. “Hip and knee replacements are proven to be long-lasting medical interventions that offer immediate improvement in a patient’s quality of life. We are now using the best available technologies to reduce the limitations of human error and off-the-shelf technology, bringing these procedures even closer to perfection.”
Featured
Douglas B. Unis, MD
Associate Professor Orthopedic Surgery
