Mount Sinai’s Elizabeth R. Dennis, MD, MS, is on a mission to optimize outcomes and improve quality of life for patients with patellofemoral instability.
The multifactorial condition, responsible for about 3 percent of all knee injuries, commonly occurs in adolescent females between the ages of 14 and 18 years. About a third experience recurrent instability. The condition can hinder participation in sports and other activities and cause persistent apprehension and long-term damage to the knee.
“They feel they can’t trust their knees,” says Dr. Dennis, an Orthopedic Surgeon in the Division of Sports Medicine, Mount Sinai Health System, and Assistant Professor, Orthopedic Surgery, Icahn School of Medicine at Mount Sinai. “It can be really debilitating for them. In the past, we didn’t know as much as we do today about how to treat it and patients were commonly just referred for physical therapy. Today, we know a lot more but we still have a lot of questions that we don’t know the answers to. I have been fortunate in my training to be able to do research around answering some of those questions.”
In addition to age and gender, other known risk factors for patellar instability include trochlear dysplasia, patella alta, lateralized force vector, femoral and tibial malrotation, ligamentous laxity, and skeletal immaturity.
Less clear are which of these risk factors, or combination of them, predict which patients with patellar instability who sustain a first dislocation will experience subsequent dislocations. This is important because each dislocation event threatens injury to the cartilage of the patellofemoral joint.
Despite knowledge of some of the risk factors that may increase that risk after an initial instability, nonsurgical management remains the standard of care for first-time dislocators.
Thus, the research that Dr. Dennis is working on aims to answer two important questions: 1) Who is at risk for recurrent instability and, therefore, would benefit from early surgical intervention; and 2) If surgery is needed, for which patients is isolated medial patellofemoral ligament (MPFL) reconstruction sufficient, and who requires an additional bony procedure (i.e., osteotomy)?
“The ultimate goal is to help these patients get back to their sport, improve their quality of life, and preserve their patellofemoral joint,” she says.
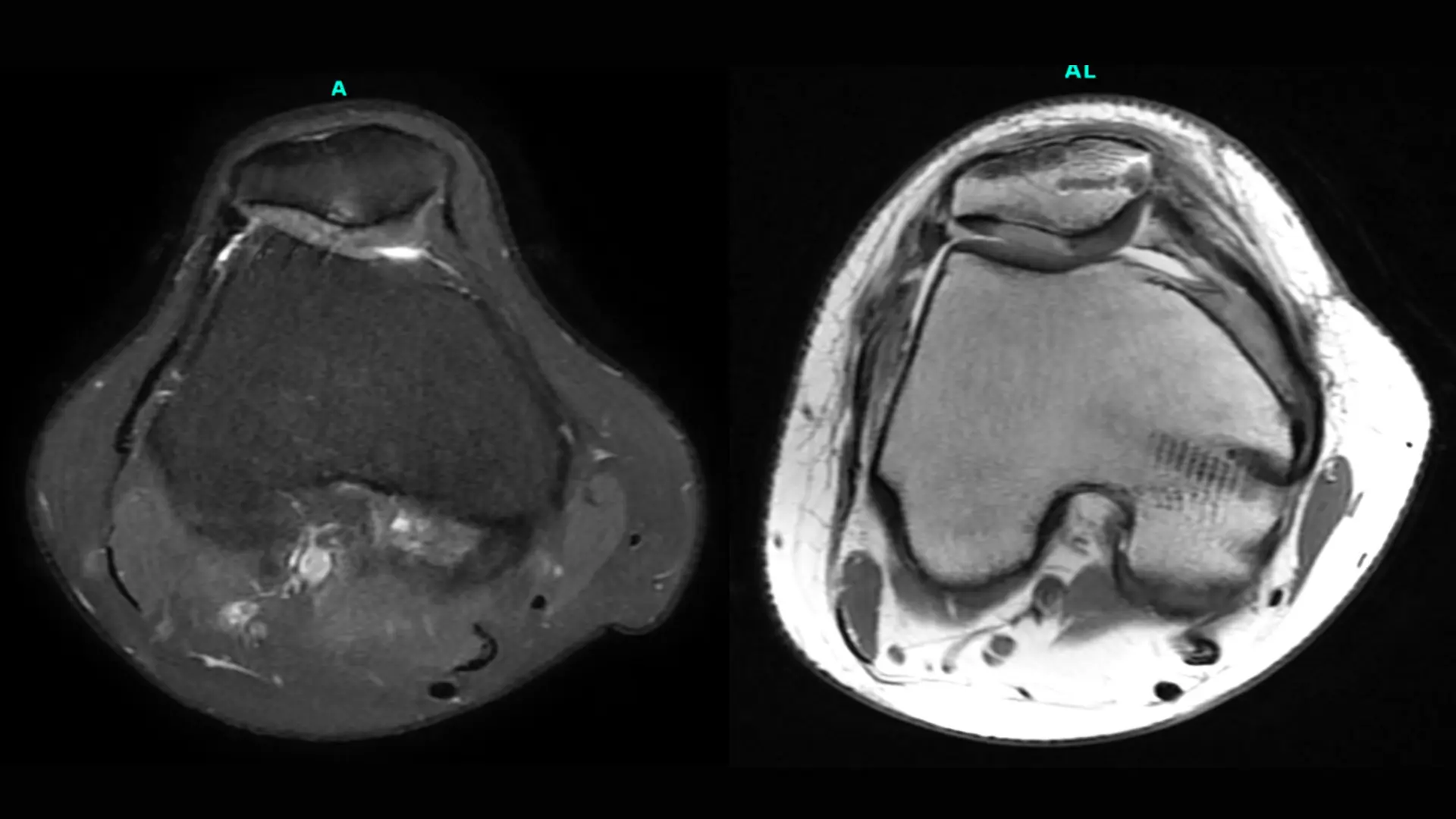
Image: A 31-year-old female patient presented with recurrent patellar instability and pain in the setting of a prior lateral release. An MRI demonstrated chondral breakdown of the lateral patellar facet. The patient underwent an MPFL reconstruction with anterior medializing tibial tubercle osteotomy and cell-based cartilage restoration to her patella.
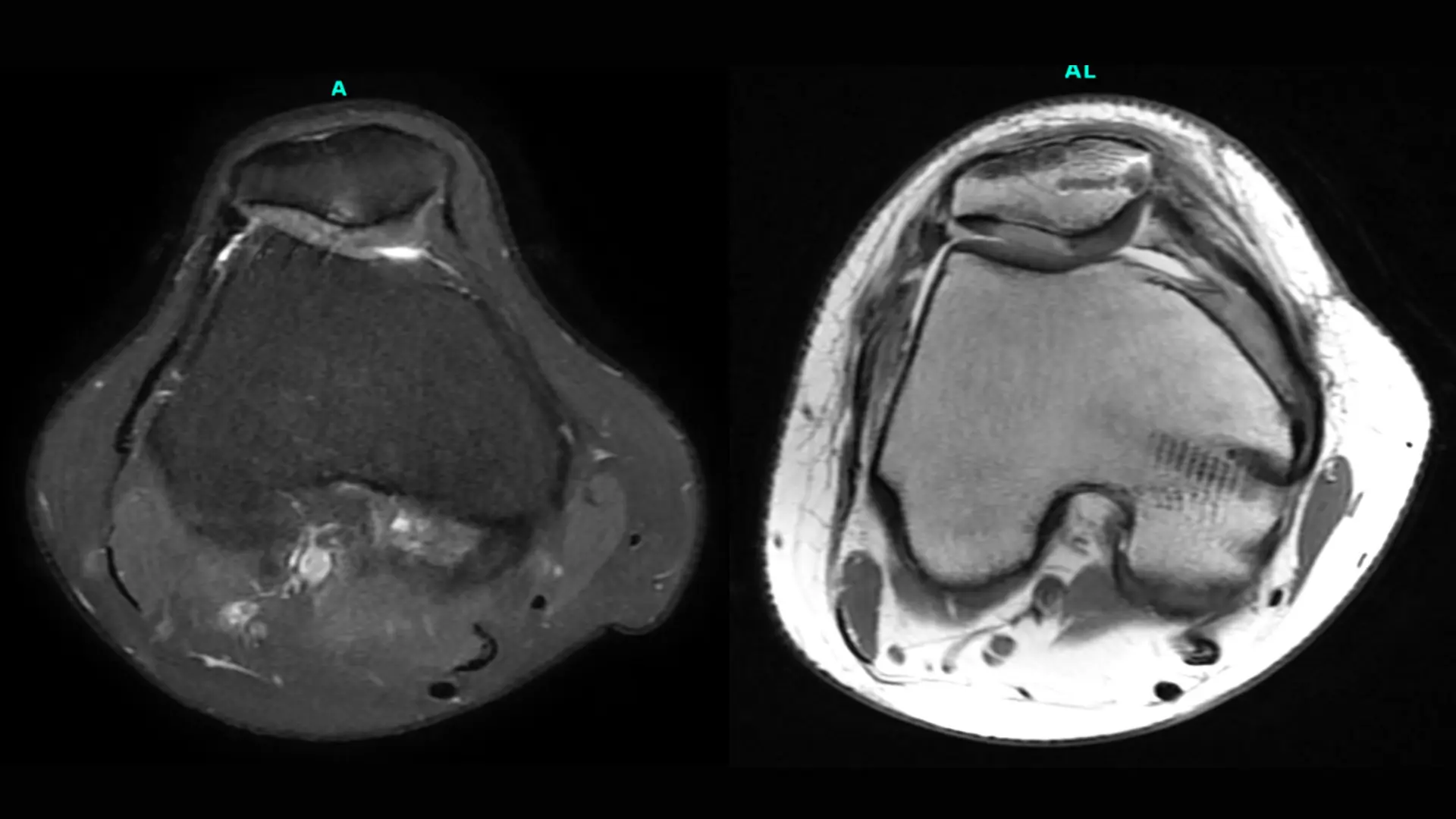
Preoperative (left) and three-month postoperative (right) MRI axial images depicting incorporation of the patient’s cell-based cartilage graft as well as her MPFL reconstruction.
The JUPITER Study
A pilot study performed at the Hospital for Special Surgery (HSS) of 138 patients with recurrent patellar instability who underwent primary, unilateral, isolated MPFL reconstruction—regardless of bony anatomy—between March 2014 and December 2019 showed favorable patient-reported outcomes and low recurrence rates at both two and five years. The study was performed while Dr. Dennis was a fellow at HSS under Beth Shubin Stein, MD, Attending Orthopedic Surgeon and Co-Director of the Women’s Sports Medicine Center at HSS.
Those patients had been selected based on their lack of exclusion criteria that are hypothesized to require a concomitant osteotomy, including an off-loadable grade 3 or 4 chondral defect, significant anterior knee pain, revision surgery, or the “jumping J” sign, describing patients who can’t fully extend their knee without dislocating their patella. This work will be published in an upcoming edition of the American Journal of Sports Medicine.
In 2024, Dr. Dennis, who began working at Mount Sinai in 2021, was invited to continue to build on this research with Dr. Shubin Stein under a nationwide multicenter collaborative called Justifying Patellar Instability Treatment by Early Results (JUPITER), a prospective cohort study that expands upon the hypotheses and goals of the previously described pilot study and is designed to better characterize the patellar instability population and identify best treatment practices. More than 2,000 patients—male and female of all ages—have been enrolled since 2016.
“It’s a big deal, and we are excited to be participating,” Dr. Dennis says. “I am very grateful to the principal investigators, Dr. Shubin Stein and Shital Parikh, MD, a pediatric sports medicine surgeon at Cincinnati Children’s Hospital Medical Center, for inviting me to participate in the study group and I'm excited to see what results we can discover.”
Video: A 25-year-old female patient with recurrent patellar instability and patella alta. Patient underwent a distalizing and anterior medializing tibial tubercle osteotomy and MPFL reconstruction.
Patient’s preoperative exam under anesthesia (left) depicting significant patellar translation and the inability of the patella to engage the trochlea until approximately 90 degrees of knee flexion. Patient six weeks postop during physical therapy (right) performing a straight leg raise and knee range of motion.
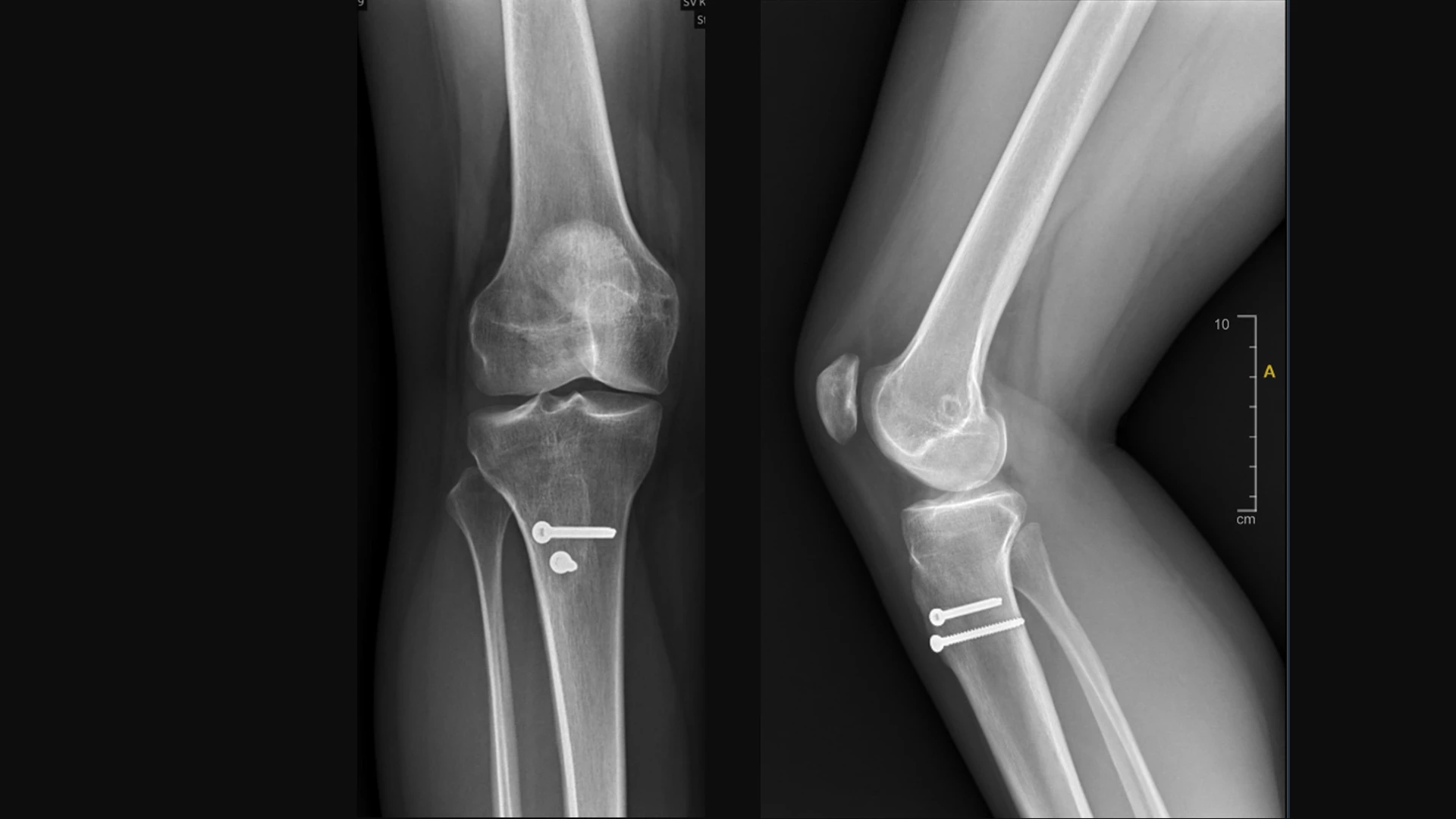
Anterior, posterior, and lateral view of the distalizing and anterior medializing tibial tubercle osteotomy and MPFL reconstruction.
The latest JUPITER phase, JUPITER 4.0, will prospectively enroll a new group of 850 consecutive patients with recurrent patellar instability. As in the pilot study, they will all undergo MPFL reconstruction but no bony procedures will be performed regardless of their patellar height or presence of trochlear dysplasia, unless the patients meet the previously described exclusion criteria.
The patients will be followed to determine who experiences recurrent instability.
“By reverse engineering, we’re trying to figure out who fails after an isolated MPFL, and what’s unique about that group of patients. Ultimately, we hope to create a treatment algorithm that surgeons can use to identify which patients will benefit from an osteotomy and those who will do fine with an isolated MPFL reconstruction,” Dr. Dennis explains.
Additionally, Dr. Dennis plans to travel around the world over the next two years as an International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) Patellofemoral Traveling Fellow, an honor bestowed on two recipients every two years, to learn from the world’s experts about complex patellofemoral surgery, including derotational osteotomy and trochleoplasty techniques.
“I am incredibly grateful to ISAKOS and the Patellofemoral Foundation for this opportunity,” she says. “Complex patellofemoral surgery is my passion, and I am excited to expand my surgical toolkit by learning from the world’s most expert patellofemoral surgeons.”
While all of this is underway, she continues to bring her expertise of treating patellofemoral instability to patients at Mount Sinai. “Patients need to know that if they are experiencing patellofemoral instability, there are solutions,” says Dr. Dennis. “It’s not limited to physical therapy and giving up sports. When you come to Mount Sinai for this care, you are part of a group that’s pushing this treatment forward.”
Featured

Elizabeth R. Dennis, MD, MS
Orthopedic Surgeon, Division of Sports Medicine, and Assistant Professor, Orthopedic Surgery