When conventional treatments failed to stop the progression of a rare, benign retinal tumor that was damaging vision in a 15-year-old boy’s left eye, surgeons at New York Eye and Ear Infirmary of Mount Sinai (NYEE) took a bold and innovative step that they believed offered the best chance of avoiding a catastrophic loss of the eye.
They turned to a complex and rarely performed intraocular surgical procedure in a final attempt to save the eye and prevent permanent and complete vision loss. Only recently described in medical literature, the groundbreaking surgery involved using microscopic instruments and ultrafine sutures to meticulously ligate the blood vessels feeding the tumor before carefully resecting the tumor itself.
“We chose to attempt a technique we had never performed before,” says Gennady Landa, MD, Director of the Retina Service at NYEE and Associate Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai. “But we were confident this approach offered the most definitive treatment for such a complex case, while sparing the patient the side effects of repeated surgeries, radiation, or chemotherapy that are often required for treatment of tumors of this type.”
Dr. Landa was joined by Neal Patel, MD, Senior Vitreoretinal Surgery Fellow, in performing the surgery in February 2025.
Over the prior year, two attempts to treat the tumor through conventional laser surgery were undertaken by Ekaterina Semenova, MD, an ocular oncologist and Director of Pediatric Ocular Oncology at NYEE and The Mount Sinai Hospital. The retinal damage from this rare tumor, known as a retinal capillary hemangioblastoma, was found to be already considerable when Dr. Semenova first saw the patient. Though noncancerous, it had led to the development of a large retinal detachment that had been slowly growing over the years and had gone unnoticed until it resulted in severe loss of vision in the affected eye.
“At first, we opted to start with a more conservative approach by trying to attach the retina and to prevent further growth of the tumor with two separate laser procedures and by injecting into the eye a medicine that aimed to stop leakage from the abnormal blood vessels. However, despite our efforts, the detachment only increased over time,” notes Dr. Semenova, who has treated her fair share of benign and malignant ocular tumors in children and adults over the years. “We knew the patient’s risk of completely losing the eye was high, so we began looking at other approaches.”
Dr. Landa, a seasoned retina surgeon used to handling the most complex retinal, macula, and vitreous surgical cases referred to him from across the New York metropolitan area, was an integral part of that conversation. He mapped out a unique and bold surgical strategy with Dr. Patel for their young patient that could accomplish three critical goals within the same procedure: ligate the feeder blood vessels, resect the tumor, and attach the retina.
The two-hour surgery began with removing vitreous gel from the center and from the edges of the eyeball to access the fragile retina and the tumor’s dilated feeder vessels. Dr. Landa and Dr. Patel then moved on to the most challenging part of the surgery—isolating and ligating the two abnormal vessels. Using intraocular forceps and the finest available sutures, they gently tied off the vessels from within the eye to prevent potentially devastating bleeding.
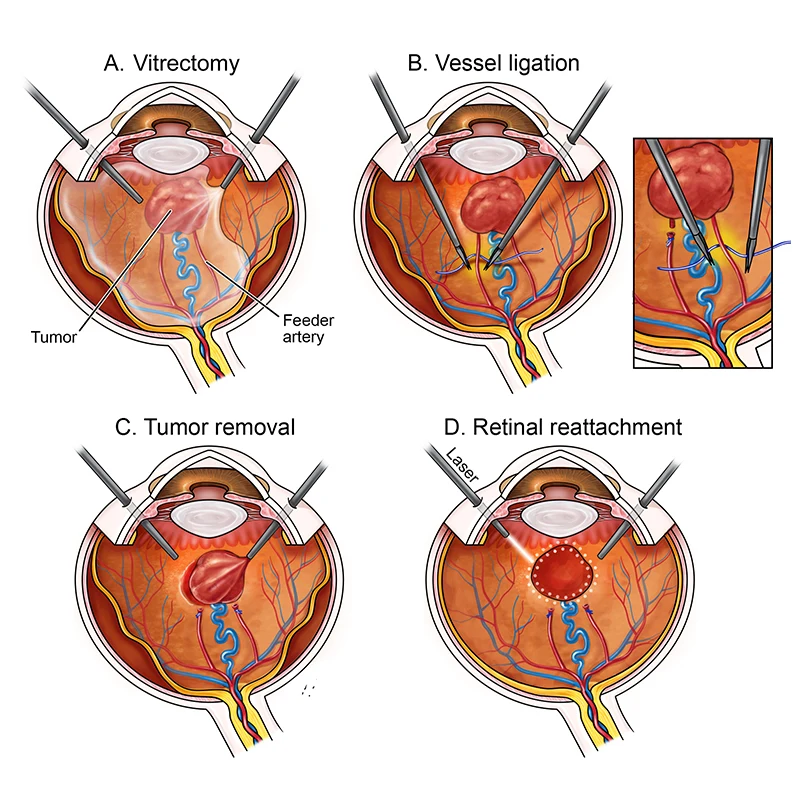
Surgical diagram showing key steps performed by Dr. Landa and Dr. Patel, including tumor removal, vessel ligation, and laser therapy to repair the retinal detachment (Gregory © 2025 Mount Sinai Health System)
“The vessels were unusually large and dilated,” says Dr. Patel. “We couldn’t simply use traditional cautery and cut them without causing severe bleeding. They had to be carefully tied off with sutures, all within the tight confines of the eye.” A bimanual surgical technique with micro forceps and ultrafine sutures allowed the surgeons to complete this challenging task.
With the feeder vessels sealed, the team proceeded to remove the tumor, which measured approximately 3 mm thick and 8 mm in diameter. The retina around the tumor was treated with additional diathermy to prevent bleeding, and both the tumor and surrounding retina were excised with minimal blood loss. The detached retina was repositioned and secured using laser therapy, and a gas bubble was inserted into the eye to maintain retinal attachment during healing.
Within two weeks, the teen had returned to his normal daily routine. The retina has remained attached, with no signs of tumor recurrence. While complete visual recovery is limited due to damage from long-standing retinal detachment, the eye appears healthy, functional, and cosmetically normal.
“We applied every bit of knowledge and surgical precision to execute this highly challenging, first-of-its-kind operation for our team, and we absolutely met our goals,” sums up Dr. Landa. “The tumor is out of the boy’s eye, the feeding blood vessels are sealed, and the retina is attached. Given the complexity and stakes, this was a major success and a testament to our collaborative efforts.”
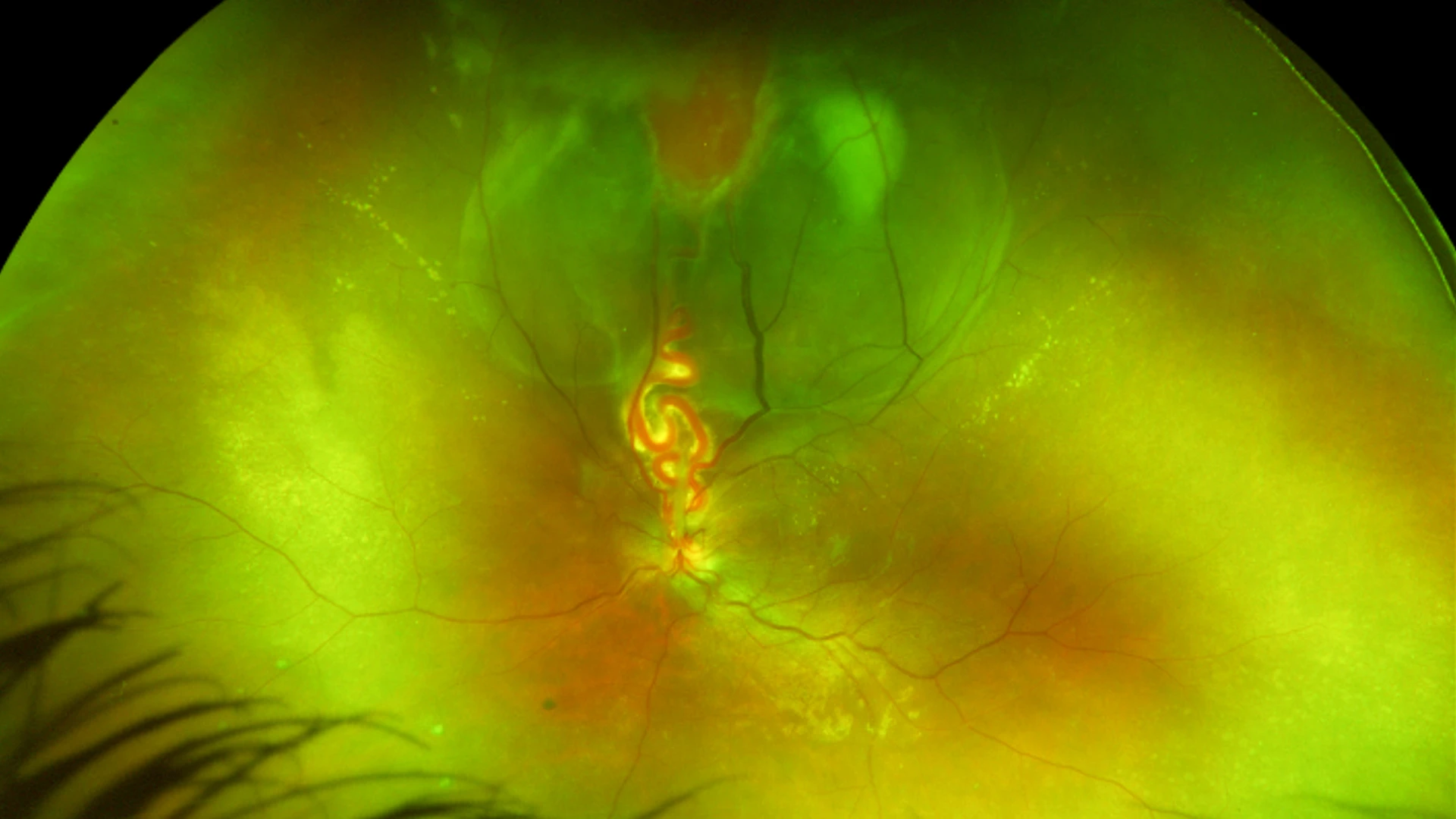
Fundus image of the tumor with a retinal detachment and the dilated feeder blood vessels
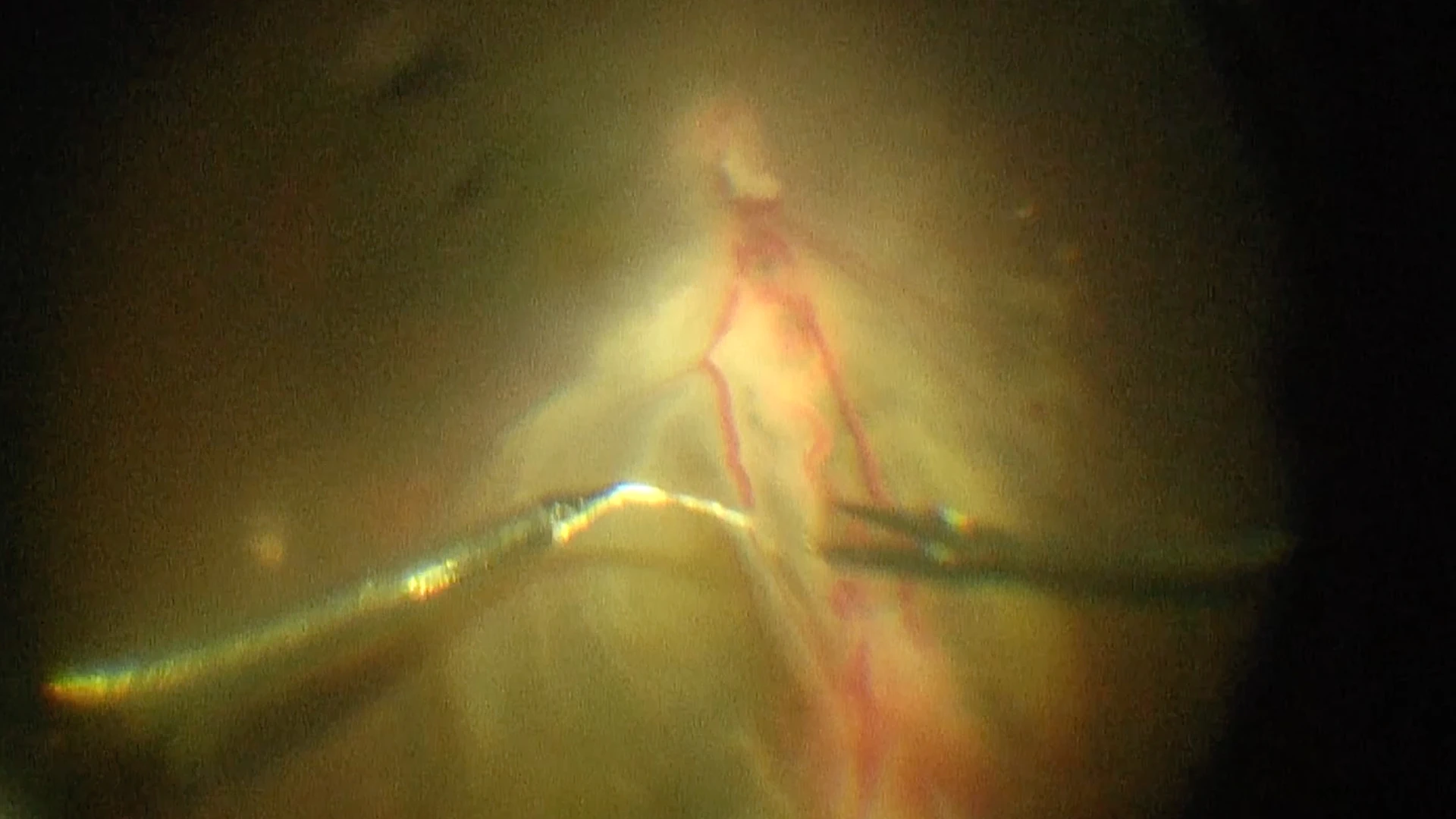
Ligation of the two abnormal vessels using intraocular forceps and sutures
