Machine learning is no stranger to the field of glaucoma, but its application to the disorders that swell the optic nerve and cause severe vision loss and potentially life-threatening diseases has been limited.
Researchers at the Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute have led a team from several institutions to advance the science, showing how machine learning can quantify the clinical stage of papilledema and guide the treatment of this optic neuropathy, characterized by swelling of the optic discs due to increased intracranial pressure. The results of the study were reported in the July issue of BMJ Neurology.
“For the first time, we’ve tasked an artificial neural network to assign a Frisén grade to fundus photographs of eyes with papilledema,” says senior author Mark Kupersmith, MD, Professor of Neurosurgery, Ophthalmology, and Neurology at the Icahn School of Medicine at Mount Sinai, and Chief of Neuro-Ophthalmology for the Mount Sinai Health System. “This information could be critical to clinicians in the diagnosis, treatment, and management of not just papilledema, but possibly other non-glaucomatous optic nerve problems such as optic neuritis and non-arteritic anterior ischemic optic neuropathy.”
Inasmuch as prior research has shown that machine learning can distinguish eyes with papilledema from normal eyes, Mount Sinai investigators were determined to learn if those curated data sets could be coupled with the Frisén scale to rate the severity of the disease and, just as importantly, indicate changes over time with a common treatment, acetazolamide, which is a carbonic anhydrase inhibitor.
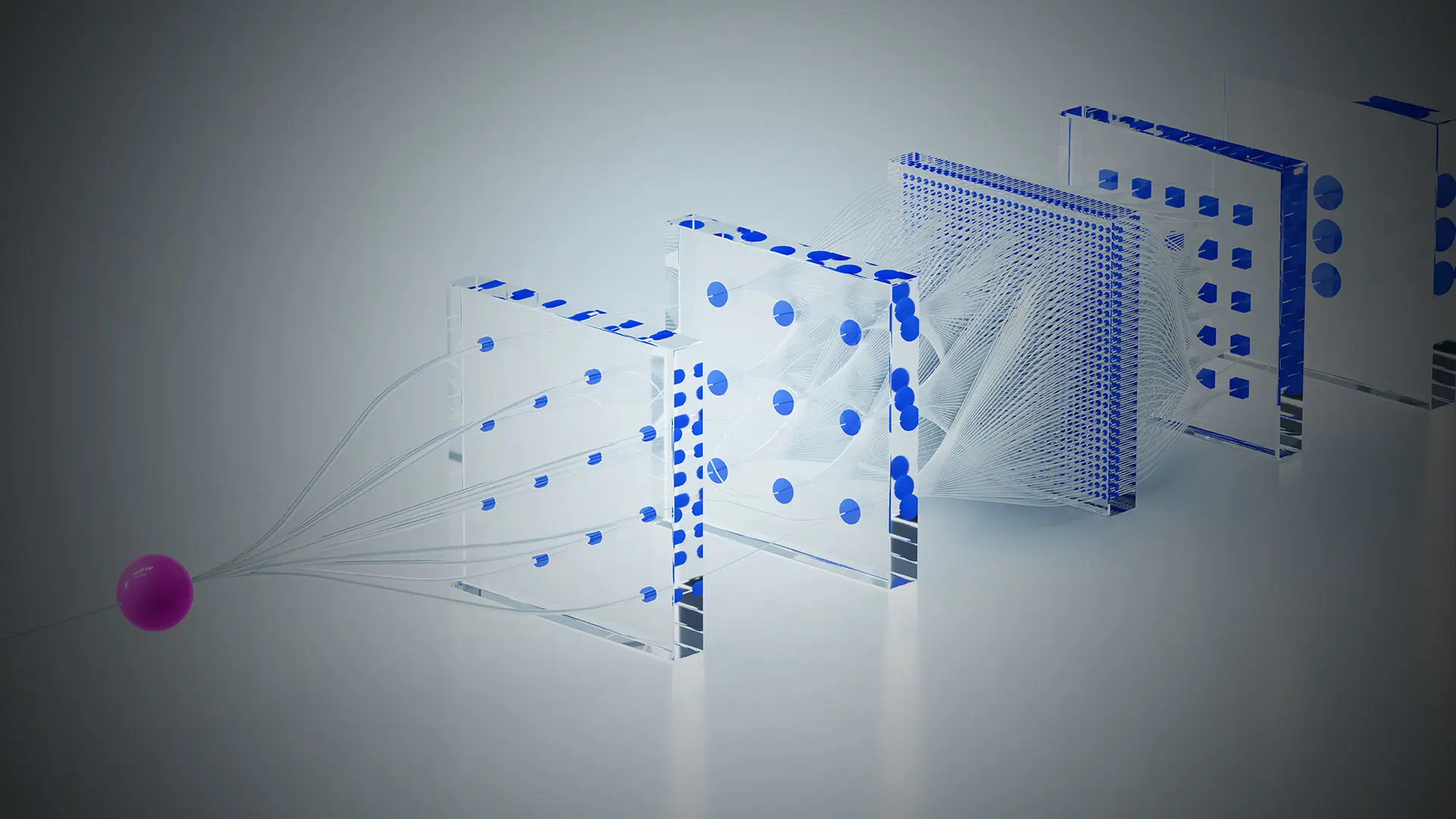
To that end, the team, which also included members from Harvard Medical School, the University of Iowa, and Cork University Hospital in Ireland, trained a convolutional neural network to assign a Frisén grade to fundus photographs taken from the eyes of 158 participants enrolled in the Idiopathic Intracranial Hypertension Treatment Trial, the first large study on the use of acetazolamide and weight loss for treating idiopathic intracranial-associated vision loss.
They learned that machine learning could indeed build on the Frisén scale to show differential changes over time in the eyes of study participants taking acetazolamide versus a placebo group.
“Our machine learning results correlated well with the expert evaluation by humans—certainly good enough for clinical use to show responses in patients to medications,” notes Dr. Kupersmith. “Given the increasing availability of fundus photography, including handheld cameras, neurologists should be able to use machine learning to quantify papilledema on a continuous basis that incorporates features of the Frisén grade to monitor interventions.” The technology could also help clinicians who have less experience and training in ophthalmology, he points out, making it a valuable diagnostic tool in emergency departments, intensive care units, and primary care offices.
The current study on papilledema is part of a larger effort by Dr. Kupersmith and his lab to explore non-glaucomatous optic nerve pathologies through the lens of fundus photography, OCT, and visual field, with eight studies under their belt.
“New York Eye and Ear Infirmary of Mount Sinai has become a center of excellence for applying artificial intelligence methodologies to optic nerve disorders,” he emphasizes. “And we’re hopeful this work will not only lead to better detection and prediction of a set of diseases that may be associated with life-threatening illness, but will do so at a stage when they can be effectively treated.”