In 1962, cataract surgery was revolutionized with the introduction of phacoemulsification, which uses ultrasonic waves to break up and aspirate out cloudy fragments of the eye’s lens. The father of that technology was Charles D. Kelman, MD, a surgeon and attending on the staff of what was then known as The New York Eye and Ear Infirmary (NYEE).
Six decades later, the next wave of innovation has arrived. It promises to reconfigure the cataract landscape through the advent of miCOR and miLOOP, which pack the power and performance of bulky phaco machines into simple handheld devices.
Just as cataract surgery’s move into ambulatory surgery centers in the mid-1980s was disruptive at the time, but soon became recognized as a safe, affordable, and familiar choice
for surgeons, the movement toward office-based cataract procedures has been gaining ground in the United States.
“Cataract surgery is transitioning to a new era of convenient office-based settings made possible by miniaturized devices like miCOR and miLOOP,” says James C. Tsai, MD, MBA, President, New York Eye and Ear Infirmary of Mount Sinai. “As a major referral center that performs thousands of cataract cases a year, we’re helping to shape this frontier by participating in a trial to refine the technology so that it’s safe and effective when finally rolled out to patients across the country. Equally as far-reaching are the implications it could have for making cataract surgery more affordable and accessible to people in developing nations globally.”
In January 2024, NYEE became the only institution in the Northeast, and one of 10 in the country, to inaugurate use of miCOR for cataract surgery.

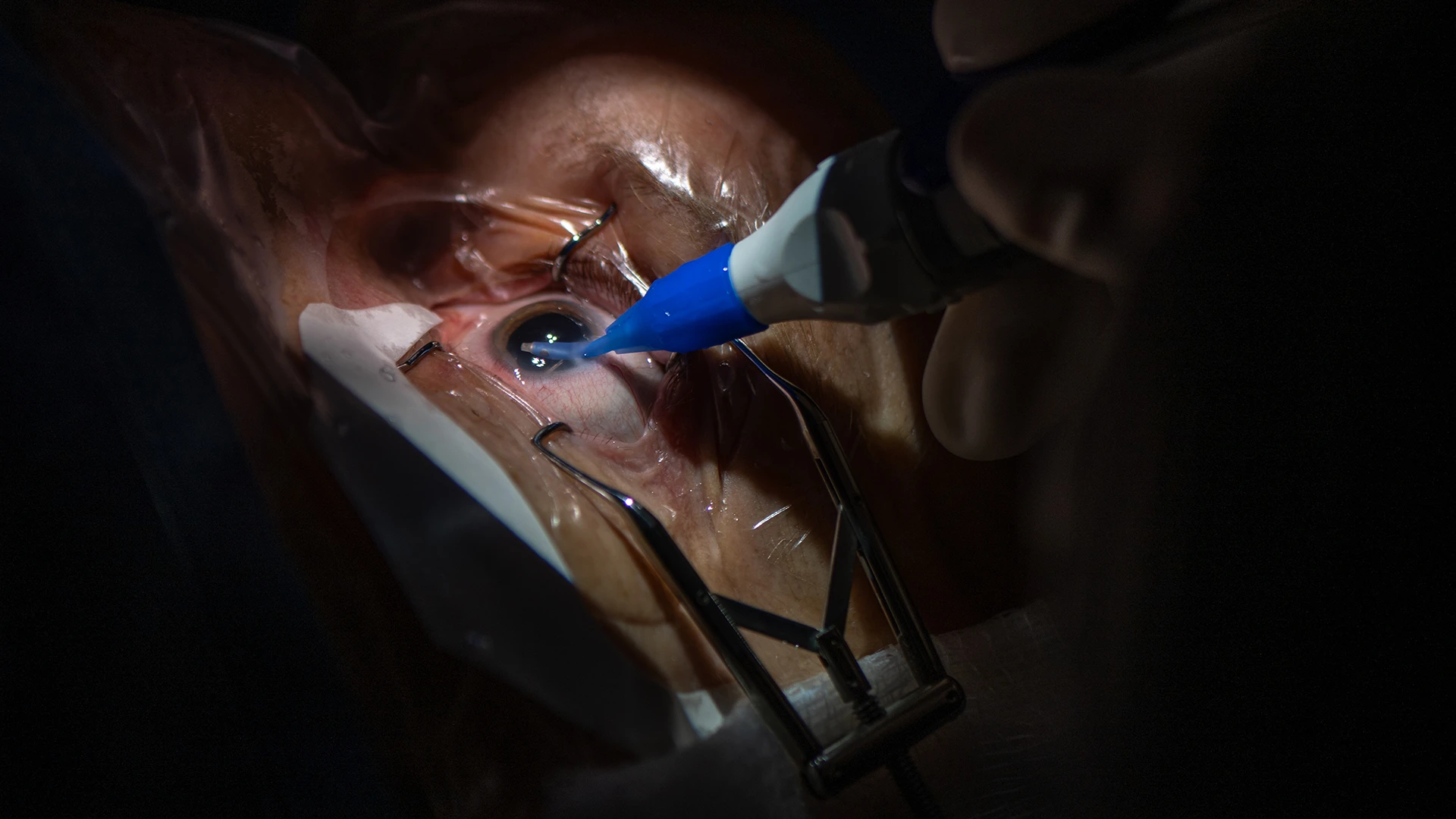
Kira Manusis, MD, performs the first cataract surgery at NYEE using miCOR, a subsonic, non-cavitating iso-thermic lensectomy system.
“For more than five decades, ophthalmologists have been waiting for new cataract technology that is not just an incremental extension of the conventional phacoemulsification technology, and miCOR puts the power of a 250-pound ‘mainframe’ machine into a miniaturized handheld lens pen, which can fragment and extract the cataract in less than five minutes with less thermal energy, no cavitation power, and less fluidic impact—not to mention the capital expense of the big phaco machines,” says Tsontcho (Sean) Ianchulev, MD, MPH, Director of Ophthalmic Innovation and Technology at NYEE. He is also the technological founder of the miCOR and miLOOP devices, which were ultimately acquired by ZEISS Medical, a global technology leader in the field of optics and ophthalmology.
For all its benefits, phacoemulsification has always had its share of vulnerabilities. It requires, for example, complex instrument-heavy equipment with significant installation and maintenance costs and a steep learning curve for ophthalmologists, and it presents challenges for treating advanced cataracts. The costs, complexity, and extended learning curve have held back cataract surgery from solving the global blindness epidemic despite a highly effective (95%+) 10-minute procedure that can restore a person’s vision and dramatically improve their life. A recent report by the World Health Organization still lists cataracts as a leading cause of blindness and visual impairment in the world, with almost 100 million people experiencing this curable condition.
To overcome these barriers, more efficient, streamlined, and scalable techniques and instrumentation that could impact cataract surgery are needed not just in the developed world, but in developing countries where cataract-related blindness is a critical and worsening public health problem.
Enter miLOOP, a groundbreaking microinterventional device with the ability to fragment all densities of cataracts using self-expanding nitinol technology to substantially reduce phaco energy and fluid use. Yet miLOOP still leaves the need for phacoemulsification to further fragment and extract dense lens segments. That’s where miCOR serves as the ideal companion for phaco-free nuclear extraction.
Approved by the U.S. Food and Drug Administration in 2022, miCOR is a self-contained lens pen that eliminates the need for a console, foot pedal, and other expensive machinery. The mechanism of fragmentation is low-frequency 40 Hz, non-ultrasonic, non-cavitating vibrations of the tip, so heat, and thus the need for fluidic irrigation, is dramatically reduced.

Close-up view of miCOR lens pen with a nucleus removal tip
Lens fragmentation and extraction using miCOR with irrigation/aspiration removal tip attachment
“Use of the device is very intuitive and requires just over a minute for my team to set up, making it much quicker to turn the room over for the next patient,” explains Kira Manusis, MD, Director of the Center for Refractive Solutions at NYEE, who has successfully performed the first procedures with miCOR at the hospital. “Everything is contained in a handpiece, and I’m able to do surgery just as efficiently as with a much larger phaco machine.”
As for getting up to speed on the device, Dr. Manusis cites “a bit of a learning curve, but not a steep one.”
In addition to the technology figuring in a growing number of successful patient procedures, it is being introduced to residents as part of their surgical training. “We want our trainees to be prepared for the future and the changes in technology that may have a profound impact on how they practice their craft,” points out Dr. Manusis.
Dr. Ianchulev, a faculty member at NYEE, is a founder, board member, and/or equity owner of multiple life-science companies, including the public company Eyenovia, Inc., and private companies Iantrek, Inc., and Aeye, Inc. As a prominent innovator in the field of ophthalmology, he is the holder of multiple issued and pending patents including the technology related to the development of cataract surgery devices discussed in this article. This technology was sold to ZEISS; Dr. Ianchulev has no current financial interests with ZEISS and does not benefit financially from the sale of these devices.
