After diagnosing a three-year-old boy with unilateral retinoblastoma in the right eye, Ekaterina Semenova, MD, PhD, an ophthalmologist and surgeon with the Ocular Oncology Service at New York Eye and Ear Infirmary of Mount Sinai (NYEE), presented the mother with two options. One was removal of the cancerous eye; the other was preserving it by delivering a chemotherapeutic agent directly to the tumor site through intra-arterial chemotherapy (IAC).
There was little question in the mind of the mother or surgeon over which course to pursue. And in August 2022, NYEE teamed up with the Mount Sinai Pediatric Cerebrovascular Disorders Program to become one of the few institutions in the New York metropolitan area to treat retinoblastoma, the most common type of eye cancer in young children.
“We now have in place a highly skilled multidisciplinary team to provide this specialized service, including ophthalmology, neuroendovascular surgery, pediatric oncology, radiology, and anesthesiology,” says Dr. Semenova, Assistant Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai, who proposed starting a retinoblastoma service after joining the department in October 2021, and received strong support from NYEE leadership. “We’re now treating our second patient and as people become more aware of this service, we believe the demand will grow.”
The success of the first young patient is cause for encouragement. Dr. Semenova, who led the multidisciplinary team, discovered the tumor (nearly 10 millimeters in thickness) arising in his retina, and recommended a two-part course of treatment. It consisted of intra-arterial chemotherapy done by Johanna Fifi, MD, a neuroendovascular surgeon and Professor of Neurosurgery, Neurology, and Radiology at Icahn Mount Sinai, to target the tumor, followed by a series of intravitreal chemotherapy injections by Dr. Semenova to eliminate the tumor seeds floating in the vitreous.
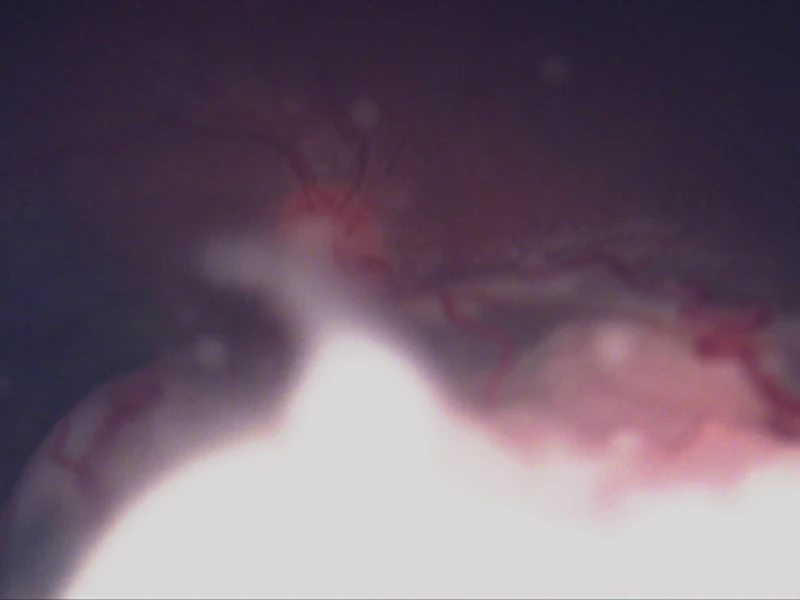
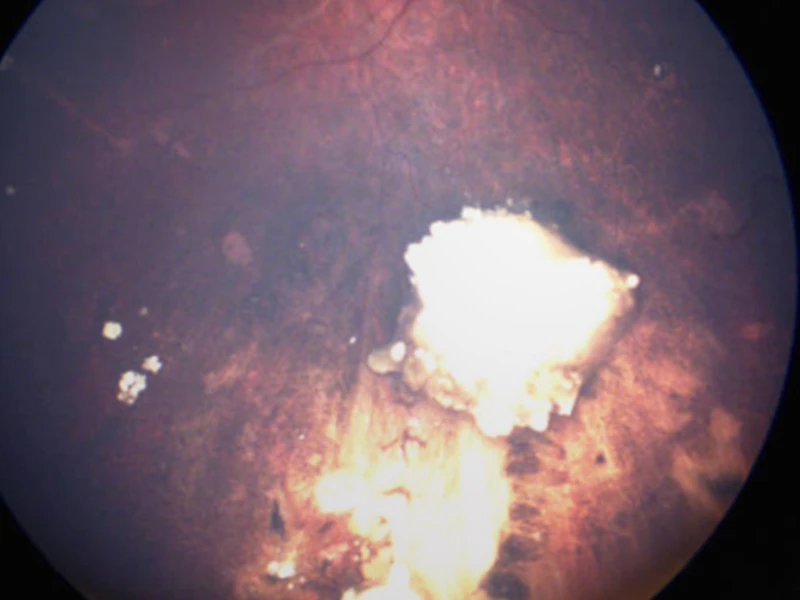
Fundus photo of the right eye showing large retinal tumor with vitreous seeds and retinal detachment before the treatment.
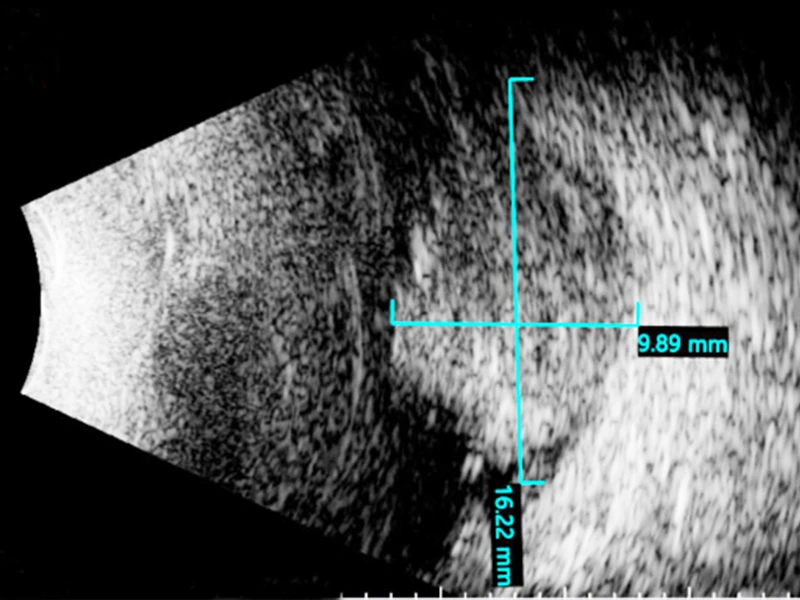
Ultrasound of the retinal tumor measuring 9.9 x 16.2 mm in size before the treatment.
“The child’s tumor was very large, which ruled out such alternative forms of eye-salvaging treatment as cryotherapy, thermotherapy, and plaque radiation therapy. External beam radiation is very rarely used now because it can cause secondary cancers and disfigurement of the face,” explains Dr. Semenova. “The field has been moving to intra-arterial chemotherapy over the past 15 years, and we judged it to be the most appropriate choice for this patient.”
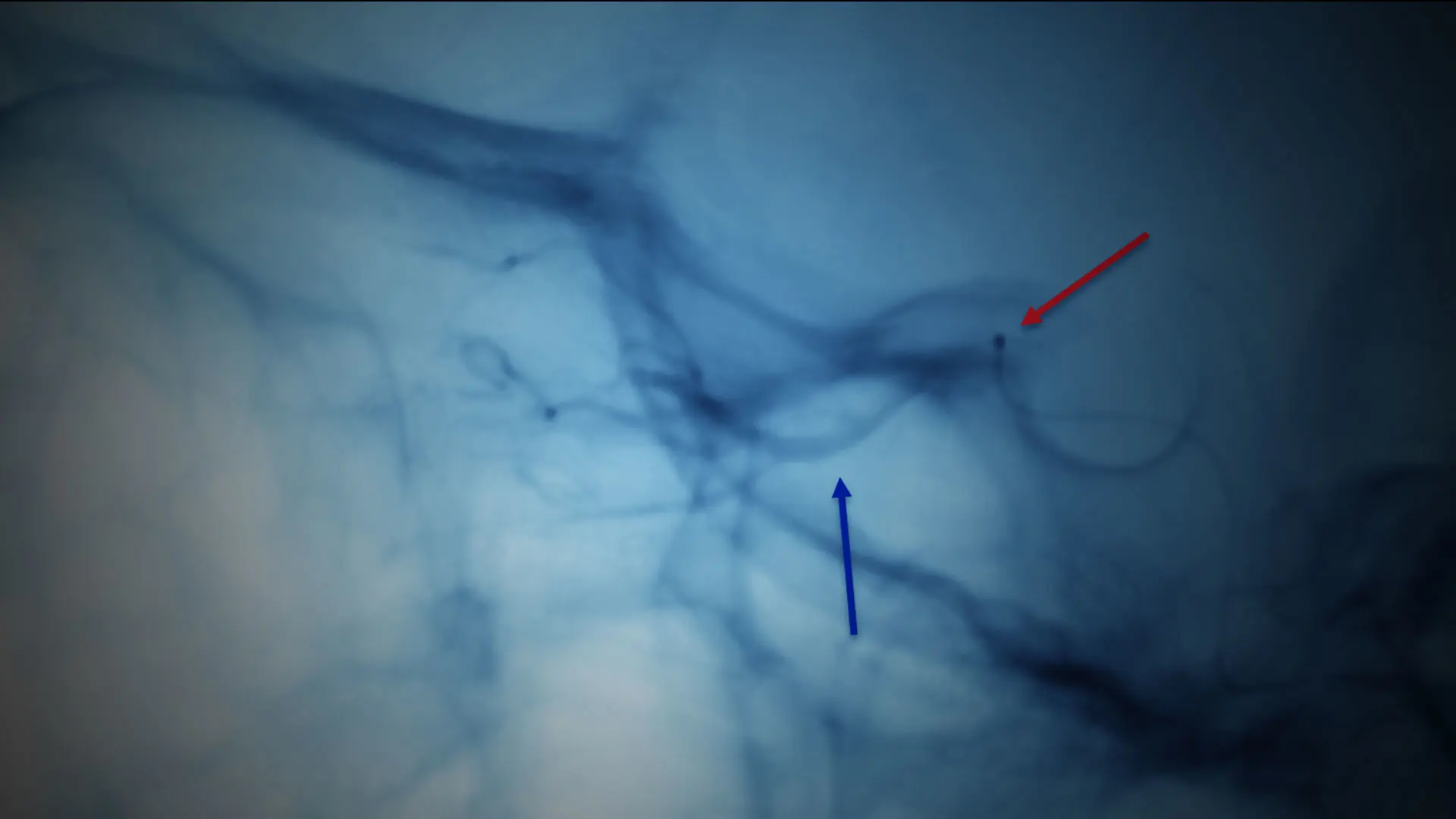
Dr. Fifi delivered the first of three rounds of the chemotherapeutic agent melphalan, spaced a month apart, directly to the tumor site, working with a Mount Sinai neurointerventional team that included a pediatric anesthesiologist. This required gaining access through the femoral artery and snaking a microcatheter into the carotid and then the ophthalmic artery using X-ray guidance.
“Because we were directly hitting the tumor, we could inject a lower dose of chemotherapy than if we used [conventional] intravenous chemotherapy, thus avoiding the use of multiple agents with greater toxicity,” notes Dr. Fifi, who is the Associate Director of the Cerebrovascular Center at Mount Sinai and Co-Director of the Pediatric Cerebrovascular Disorders Program at Mount Sinai Kravis Children’s Hospital. “In the case of this young patient, the outcome was terrific. His tumor shrank with each treatment and was completely inactive after a few months.”
But intra-arterial chemotherapy alone was insufficient to eradicate the cancer. It left largely untouched the vitreous seeds, which threatened to grow within the gel inside the eye if not properly treated. This is where Dr. Semenova’s training and knowledge proved critical.
Soon after Dr. Fifi completed her work, Dr. Semenova began a regimen of three intravitreal chemotherapy injections over several months, requiring use of a special technique to prevent cancerous cells from growing. “When I injected the chemotherapy, I performed cryotherapy at the same time around the needle to keep the tumor cells frozen in place when the instrument was withdrawn from the vitreous,” she says.

X-ray showing delivery of intra-arterial chemotherapy agent. The red arrow is showing the microcatheter tip in place and blue arrow is pointing to dye in the ophthalmic artery.
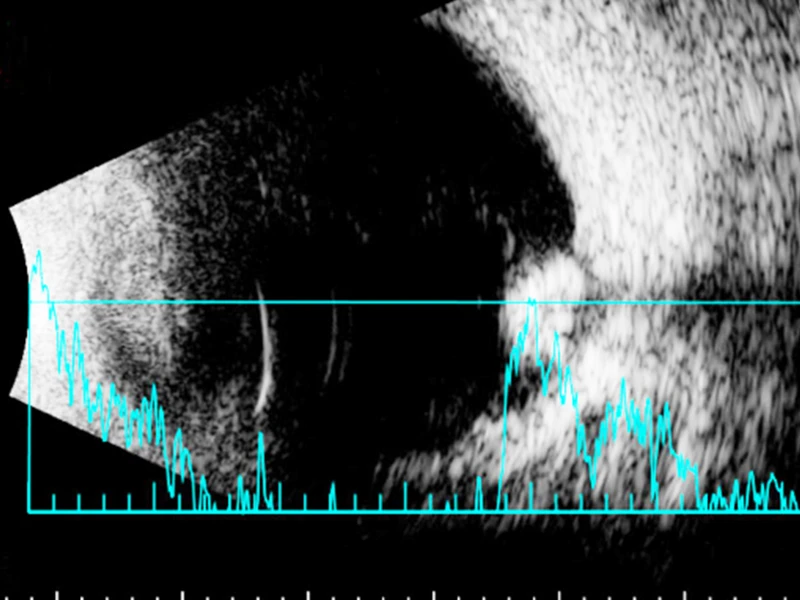
Ultrasound of the right eye showing regressed and completely calcified (dead) tumor after the treatment.
Fundus photo of the right eye after treatment showing completely calcified (dead) retinal tumor with calcified (dead) vitreous seeds.
During Dr. Semenova’s examinations of the patient following the last procedure in February 2023, the success of the injections was clear. “The vitreous seeds were gone, along with the tumor, and a retinal detachment we initially found also disappeared,” she observes. And while the child’s sight out of the affected right eye was only 20/250—slightly worse than prior to surgery—there was a more significant outcome to be weighed. “We preserved the boy’s eye and his vision,” says Dr. Semenova. “And six months out, there is no sign of cancer. We look upon these as major successes.”