When Amer Stanic, a 15-year-old boy with a severe bilateral eye infection, was referred to Anita Gupta, MD, Director of the Cornea Service at New York Eye and Ear Infirmary of Mount Sinai, his case pushed both patient and doctor to the limits.
“Amer had a serious and potentially blinding infection of both his corneas, acanthamoeba keratitis. These amoeba infections are not only exceedingly difficult to treat, but his was among the most severe cases I had ever seen,” recalls Dr. Gupta, a seasoned cornea specialist who led the team that provided nonstop support to the patient and his family. “An additional challenge was the emotional aspect: Amer was a healthy young kid with previously excellent vision, who now faced the possibility of permanent blindness.”
For the prior two and a half months, the patient had been treated with steroids for what was thought to be a pinkeye-related problem. When it didn’t improve, the parents sought a second opinion, and their son was sent to NYEE. “I was very, very scared he could lose his sight in both eyes,” admits the boy’s father, Edin Stanic. “But the doctors at NYEE were always there for us, and now he’s doing extremely well.”
NYEE’s Ophthalmic Pathology Service was the first stop, to identify the source of the infection. Codrin Iacob, MD, Assistant Director of Pathology, Molecular, and Cell-Based Medicine, made the pivotal diagnosis of acanthamoeba keratitis, a rare infection of the eye caused by a microscopic free-living amoeba that can result in visual impairment or, in the worst case, blindness. The invaders are known to burrow under contact lenses, which seemed likely in this case since the teenager had started wearing lenses less than a year earlier.
An initial examination by Dr. Gupta showed that both corneas were infected, and that the teen’s vision had been reduced to counting fingers in the right eye and 20/250 in the left eye.
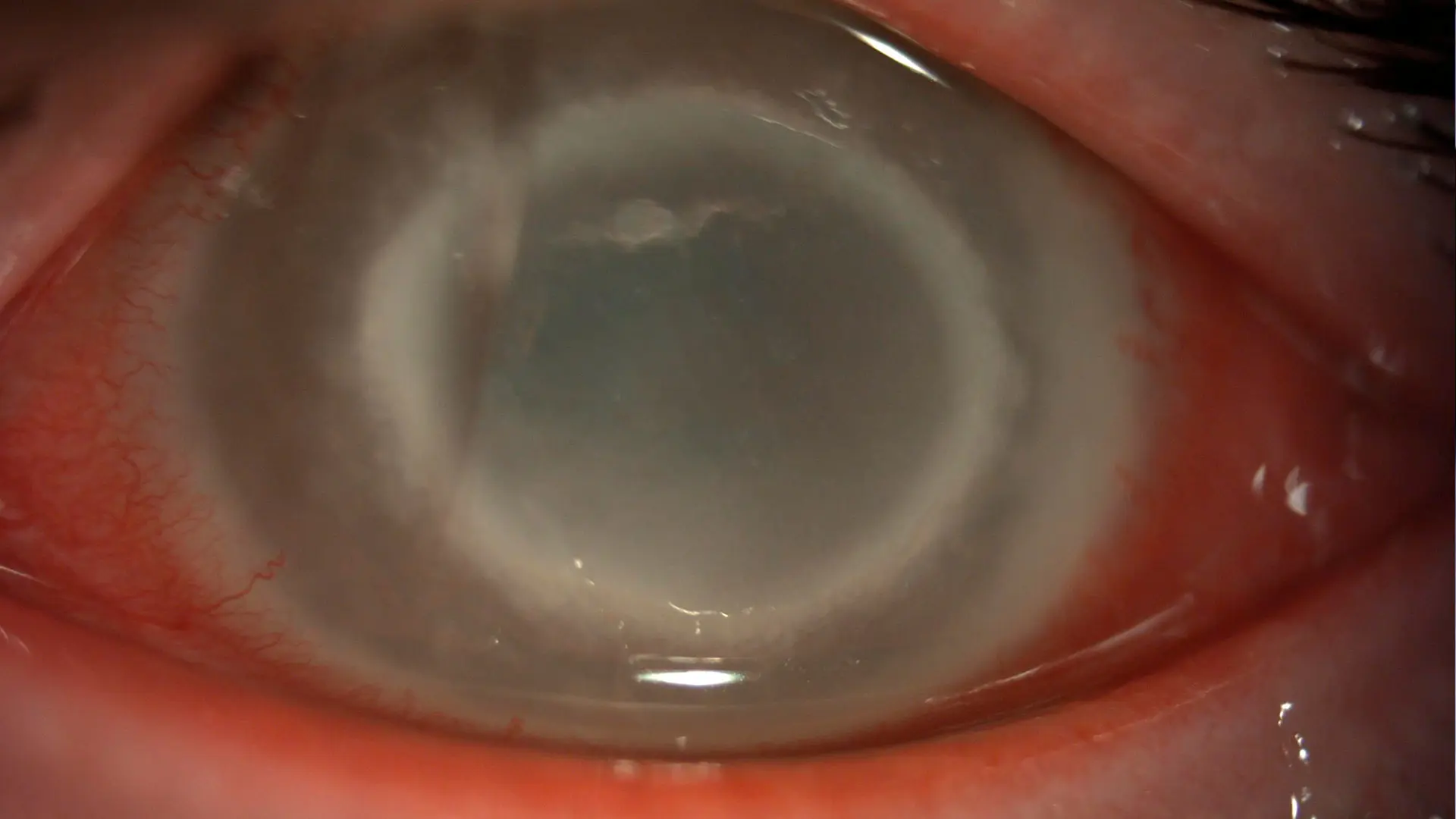
Fulminant acanthamoeba keratitis: Slit lamp photo of the left eye demonstrating large corneal ring infiltrate with diffuse stromal haze and edema. Visual acuity is 20/250.
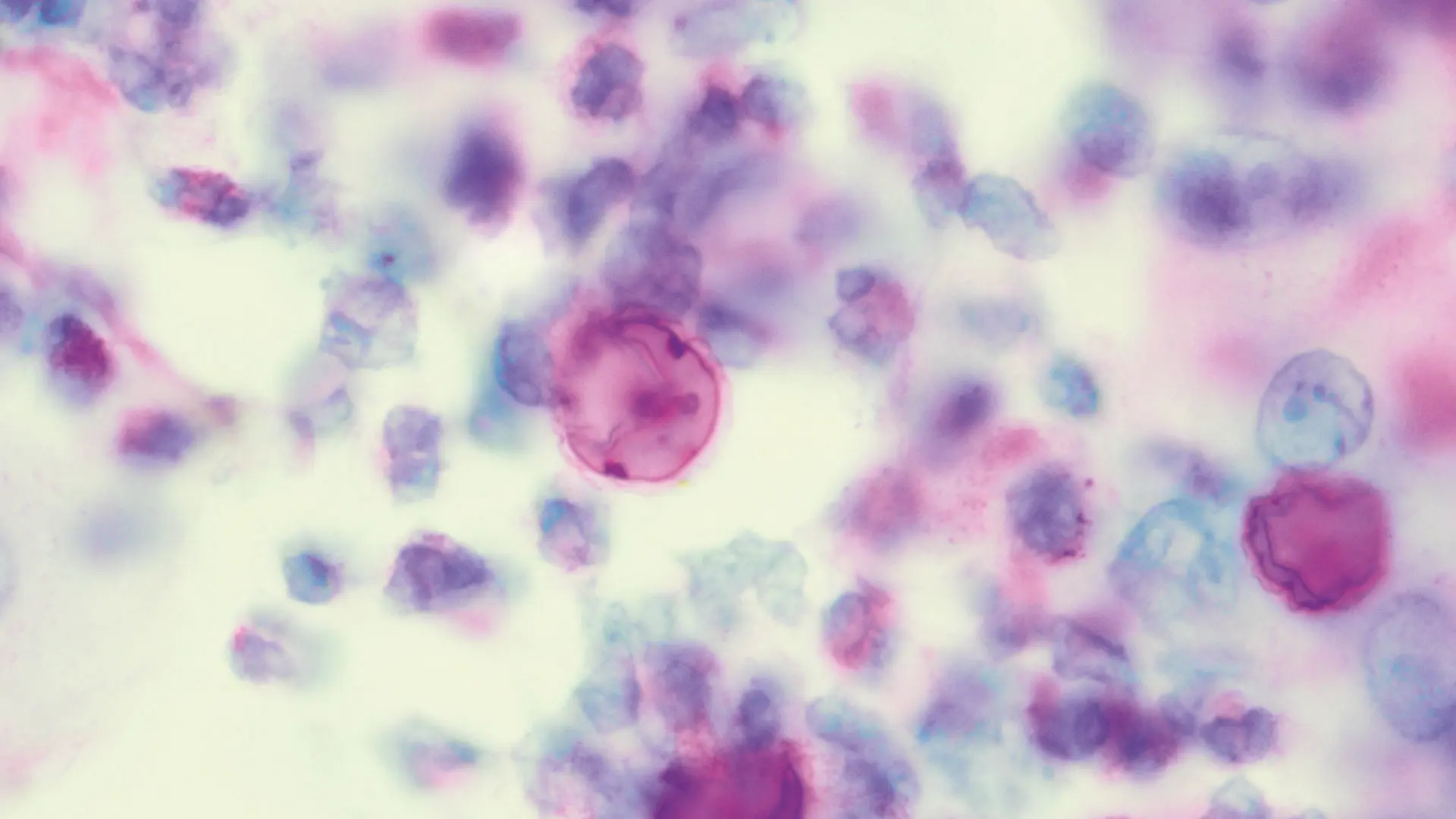
Oil immersion optic microscopy with Periodic Acid Schiff
staining shows an unstained thick
capsule of Acanthamoeba cyst with internal labeling of cuticle and organelles in the acute inflammatory background (cytology, original magnification 1000x).
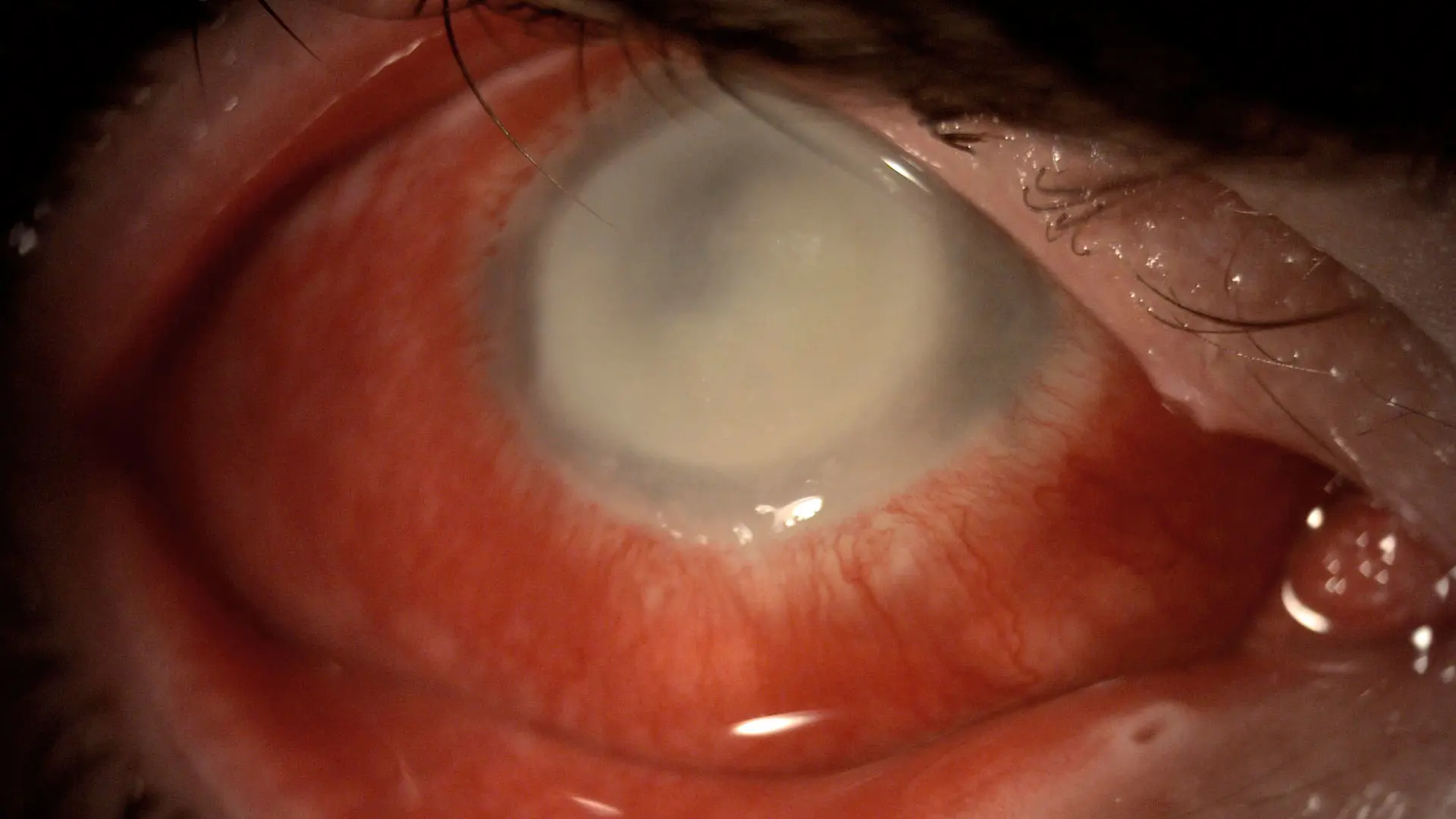
Slit lamp photo of the right eye demonstrating dense corneal infiltrate extending to the corneal limbus, with significant conjunctival injection and focal areas of scleral involvement. Visual acuity is counting fingers.
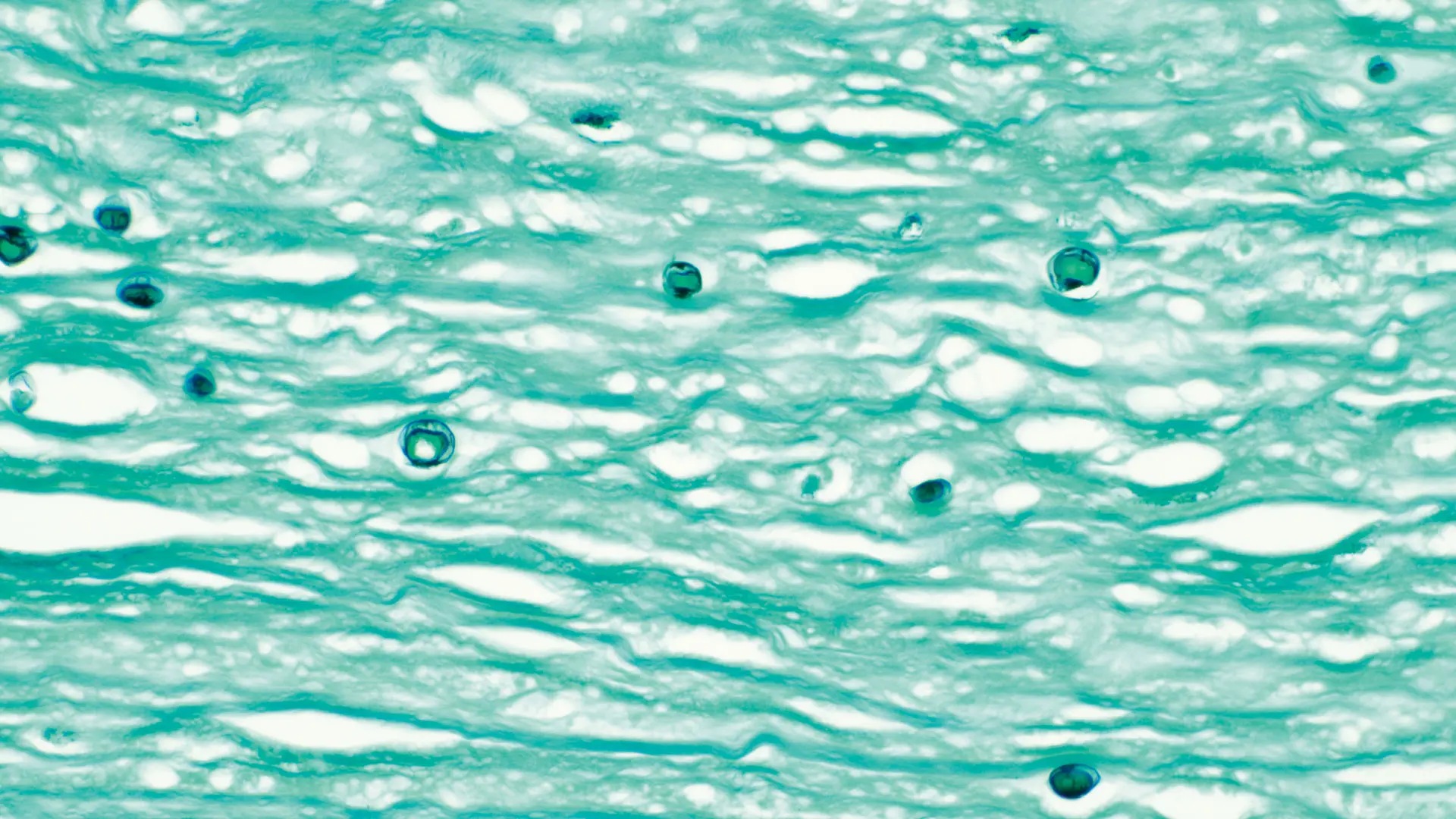
Gömöri Methenamine Silver staining highlights the thick capsule of the parasitic cysts in all strata of the corneal stroma (histology, original magnification 200x).
When his condition failed to improve over the next few weeks despite various combinations of medicines, including specialty antimicrobial medications compounded by the NYEE pharmacy, Dr. Gupta knew that major surgery would be needed. “I was very concerned about him,” she says. “He needed cornea transplant surgery in both eyes emergently. The success rate of the procedure when there is such extensive infection and inflammation is limited to around 30 to 35 percent, with a high chance of donor graft failure as well as other complications. Despite these risks, we had no other choice, and proceeded with surgery in both eyes just four days apart.”
Dr. Gupta’s concerns were well founded. In the operating room on May 15, 2020, with a pandemic raging outside the walls of the hospital, she first addressed the left eye, considered the more salvageable of the two, performing a penetrating keratoplasty to remove a large 12mm section of infected cornea. But even after that resection—the maximum deemed safe—amoeba remained around the cut edge, threatening to undo the intricate work surgeons had just completed. She sutured the donor graft in place, cauterized around the entire edge to try to kill off more of the microscopic invaders, and left the surgical suite hoping for the best for her young patient.
The scene repeated itself four days later as Dr. Gupta transplanted the cornea of the right eye in an equally difficult procedure. Within three weeks, however, results were apparent. “Amer did remarkably well,” Dr. Gupta recounts. “His corneal transplants were healing, and his vision improved significantly. Unfortunately, though, he was still at significant risk for further complications given the persistent infection and scarring in both his eyes.” Indeed, as typically happens with acanthamoeba, dying cysts from the remaining infection trigger an overwhelming inflammatory reaction that attacks and kills the cornea graft. This case was no different; at five weeks following surgery, the patient’s vision severely regressed as a result of the massive rejection of both corneas.
The uncertainty carried into the summer, when the infection appeared to have cleared but a new problem surfaced: cataracts in both eyes. So, with the patient barely seeing out of either eye, Dr. Gupta began what she refers to as visual rehabilitation. Following the initial surgery to “debulk” the infection and heal the eye, she performed a second cornea transplant on the left eye in October, made increasingly difficult by the scar tissue from the previous procedure. And while the patient’s vision improved after the transplant, it was still greatly impaired by the cataract.
The good news was that it set the stage for a turning point in the complex case. Cataract surgery was performed in December 2020 by Steven Rosenberg, MD, a pediatric specialist with NYEE at the time. Following the procedure, the teen’s left eye became stable, and his vision returned to 20/30 with regular glasses. That improvement enabled the youth to return to school and some semblance of a normal life. “This was such a huge save, thanks to a tremendous team effort we had in the middle of a pandemic,” exults Dr. Gupta, praising the work of her colleagues and residents, including then Chief Resident Masako Chen, MD, who saw the patient day after day while helping the entire family get through the ordeal.
The latest chapter was written on August 19, 2021, when Dr. Gupta returned to the OR with Dr. Chen, now a full-time faculty member and Director of the Comprehensive Ophthalmology Clinic at NYEE, to perform what ophthalmologists call “open sky cataract surgery” to remove the diseased cornea of the right eye and, while it was fully open at 8mm, opportunistically scoop out the cataract in one piece before inserting an intraocular lens and performing another corneal transplant. A follow-up visit in early September showed the teenager’s visual acuity as 20/80 at that point with excellent potential for full visual recovery once his eye heals from surgery over the next several months.
The patient can speak best to the outcome, and the journey that preceded it: “There were times that went really well, and others that went really poorly, like when the first cornea was rejected,” recalls Amer, now 16. “But after several more surgeries, things are going very well again, and it’s been consistent.” That steady progress, he adds, has allowed him to return with confidence to his senior year of high school in Brooklyn and resume friendships and activities that had been put on hold.
The encouraging results have also allowed Dr. Gupta a moment of quiet reflection after walking a fine line for so long between giving her patient hope and knowing the odds were stacked against him. “This was one of the more challenging cases I’ve handled, both because of the severity of Amer’s infection and the emotional and social challenges a young teenager faces when losing vision,” says Dr. Gupta.
“It left me proud for the incredible teamwork we have at NYEE and for the privilege we have as physicians, caring for people during profound moments in their lives.”

Amer and Dr. Chen during a follow-up visit
