The first microinterventional ophthalmic robotic assistant continues to be a focus of innovation at New York Eye and Ear Infirmary of Mount Sinai (NYEE), as we prepare for pivotal Food and Drug Administration (FDA) trials. Our collaboration with the team of robotics engineers at Preceyes BV, the Dutch company that manufactures the robot, is broadening beyond its current European approval for retinal surgery to include glaucoma and anterior-segment procedures. We are also developing a robotics surgical training curriculum for residents, fellows, and faculty to engage them in this burgeoning technological advance.
“The progress we’ve made over the past year has been substantial, even in the face of COVID-19,” says Gautam Kamthan, MD, Assistant Director of the Ophthalmic Innovation and Technology Program at NYEE, who helped coordinate activities around the robot’s arrival from the Netherlands in the summer of 2020, and is now prepping it for a major surgical role. “We’ve been able to meet all our milestones, including developing the first-ever glaucoma module for any robotic platform. And before long, we’ll be the first clinical site in the United States to offer this technology for ophthalmic surgery.”
The glaucoma module is a particular source of pride since NYEE’s technologists have been integral to its development. Paving the way for this novel surgical module was a $100,000 grant from the New York Eye and Ear Infirmary Foundation.
Mount Sinai Innovation Partners (MSIP) has also contributed critical support to NYEE efforts to advance the ophthalmic surgical robotics program. MSIP, which helps translate Mount Sinai ideas, inventions, and discoveries into commercial products and services that benefit patients, made a meaningful investment in Preceyes and now holds a seat on its board of directors. “We pursued the relationship after identifying its product as highly innovative, and one that could differentiate New York Eye and Ear from other institutions,” says Erik Lium, PhD, President, Mount Sinai Innovation Partners. “It’s also consistent with our mission to support products that embody patient-centric innovation.”
A case in point is the extension of the surgical robot’s capabilities to the anterior segment of the eye for gonio-based glaucoma surgery. “This innovation can have a tremendous impact on new glaucoma stents and minimally invasive glaucoma surgery by improving implantation precision and reducing rates of malposition,” notes Tsontcho (Sean) Ianchulev, MD, MPH, Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai and Director of the Ophthalmic Innovation and Technology Program at NYEE. “Our glaucoma module can improve surgical precision from 100 microns achievable manually to less than 5 microns.” Technicians have completed validation of the module using high-fidelity eye models, he adds, and are now moving to a head-to-head study against conventional manual surgical intervention.
While the goal is to eventually position the module for FDA trials, that out-of-the-gate task will be handled first by the robotic assistant’s retinal component. The FDA trial for which the robot is now being prepped revolves around epiretinal membrane peeling, a delicate procedure to remove the micron-thin sheets of cells that grow over and distort the macula, reducing central vision. To evaluate the precision and accuracy of the robot in complex surgical procedures, NYEE is testing the device in the Jorge N. Buxton, MD, and Douglas F. Buxton, MD, Microsurgical Education Center, using the virtual reality EyeSi Surgical simulator.

Gautam Kamthan, MD, demonstrating the modified robot using a Kahook Dual Blade to remove the
trabecular meshwork to NYEE residents Shravan Savant, MD, and Maria Castanos, MD
The EyeSi Surgical simulator in the Buxton Microsurgical Education Center allows ophthalmic surgeons and trainees to practice epiretinal membrane peeling
The study will compare its impact in different user groups—including experienced retinal surgeons, fellows, residents, and, intriguingly, video gamers—to perform the epiretinal membrane peel with and without the assistance of the robot. In preparation, each group is given a half-hour of training on the procedure using the simulator. For comparative purposes, they will perform the same surgery and surgical maneuvers manually on the EyeSi simulator. “The results should be quite interesting given that one comparative group consists of gamers who have no surgical experience, but are very skilled at using a joystick, like the one on the simulator,” remarks Dr. Ianchulev.
“The special training course that’s being created for the robotic assistant will help train the next generation of ophthalmic surgeons in a technology that is rapidly sweeping through other surgical subspecialties. It will have applications for gene implantation, retinal intravascular interventions, and micromanipulations currently beyond the reach of the best of today’s manual surgery. It will enable a new level of precision and repeatability for tasks that require slow, delicate surgical acrobatics needed to reach our next level of sight-saving therapies,” states Richard B. Rosen, MD, Vice Chair and Director of Ophthalmology Research at NYEE, and Chief of Retina Service at Mount Sinai Health System.
According to Dr. Kamthan, the plan is to eventually integrate robotic training into NYEE’s ophthalmic surgical curriculum, based on the enormous interest residents and residency applicants have already shown. Among other things, he stresses, “it will be a major attraction for prospective residents and fellows when they’re considering where to train. We’ll be able to offer them the only robotic training program of its type in the world.”
Here are details about some of the ways that NYEE is extending the robot's capabilities into glaucoma and anterior-segment surgery:
![[see below]](https://images.ctfassets.net/iujm5coq335o/5SLfvVWuX2oEkG4bPrmXNh/002b06474f3fb49bdd429c4e5f2208bc/-OPHTH2021-_3_Image_5.jpg?fm=webp)
[see below]
![[see below]](https://images.ctfassets.net/iujm5coq335o/4iShf3buPlwabM6GwbTmxm/da2685125b9285b9d8315c5a81fc1b98/-OPHTH2021-_3_Image_6.jpg?fm=webp)
[see below]
iStent Inject Trabecular Bypass Shunt Device
Image 1: The Preceyes Robotic Surgical System (PRSS) is positioned for entry into the anterior chamber of the model eye. Although initially designed for vitreoretinal surgery, the platform has been successfully adapted for the anterior segment. The iStent Inject Trabecular Bypass Shunt is a first-of-its-kind minimally invasive glaucoma surgery (MIGS) apparatus that is currently the most implanted MIGS device. Challenges remain with implantation technique and a high rate of malposition. The trabecular meshwork is about 100 microns in size which makes it difficult for conventional manual gonio-surgery. The micron-level robotic precision is 10x higher than what is possible with unaided human dexterity and can enable a categorically higher resolution of surgical intervention.
Image 2: After the robot enters the anterior chamber, the surgeon places a lens onto the surface of the eye, coupled with clear gel to enable visualization of the patient’s trabecular meshwork, the target of the iStent. A hurdle to effective implantation is a surgeon’s natural resting tremor. At this microscopic scale, a tremor can decide whether the implant is a success or not. However, with the robot’s greater improvement in stability over even the best human hands, the surgeon has the opportunity to ensure the sights of the injector are exactly where they want them before they shoot.
![[see below]](https://images.ctfassets.net/iujm5coq335o/7cuHY3RsumsU109y1ua5Hm/9d8c72c42558a231817ef676429b6f7b/-OPHTH2021-_3_Image_3.jpg?fm=webp)
[see below]
![[see below]](https://images.ctfassets.net/iujm5coq335o/5oYmKdx31XrNSgKCyJerXJ/b3e957e4a0723cfa853be6fa7afb57ee/-OPHTH2021-_3_Image_4.jpg?fm=webp)
[see below]
Kahook Dual Blade Device
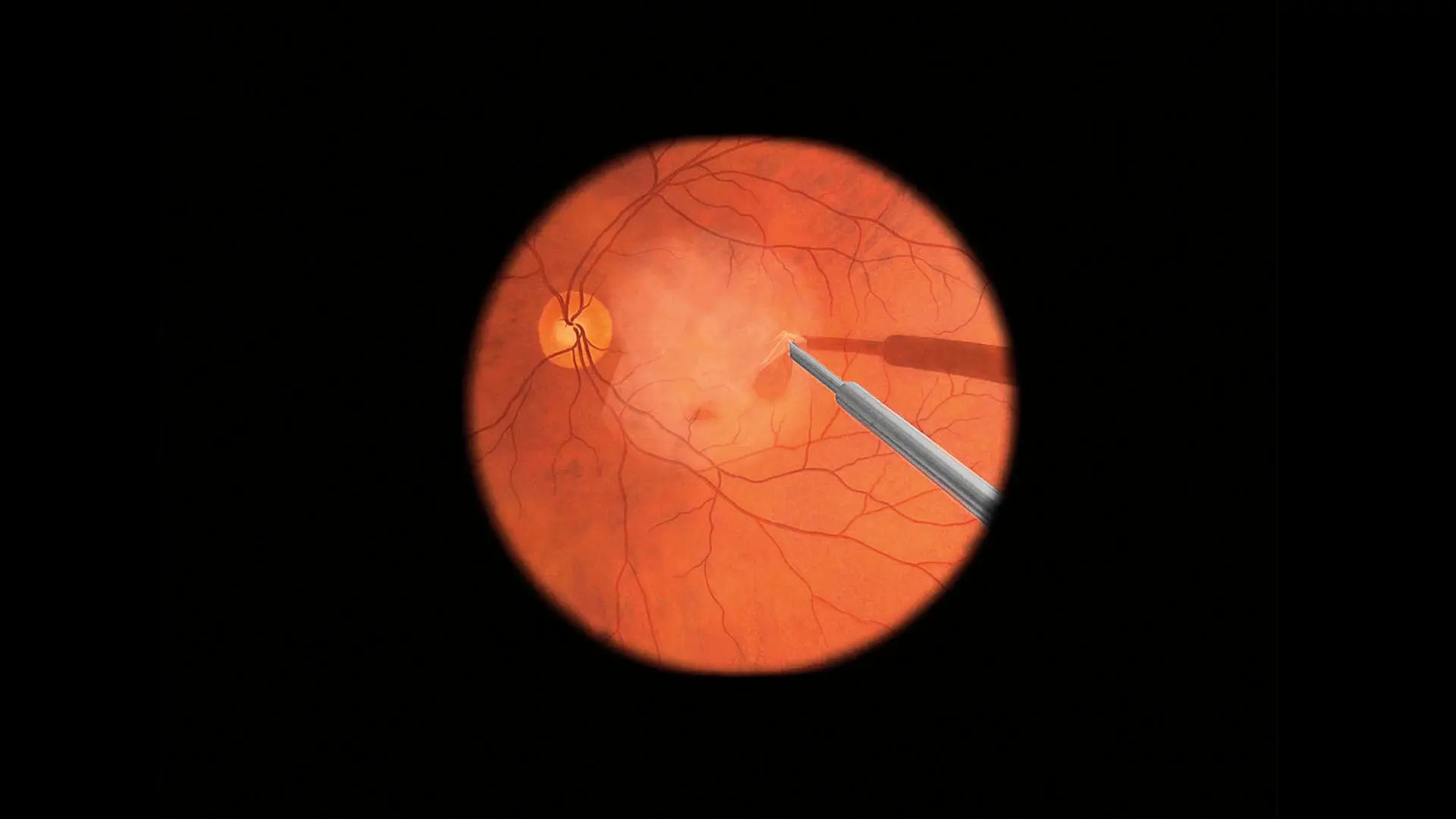
Image 1: While the iStent is the most commonly implanted MIGS device, the Kahook Dual Blade® (KDB) is the most commonly used non-implanted MIGS device. We wanted to demonstrate feasibility with both approaches using the robot. The KDB works by removing the trabecular meshwork of the angle in a sweeping motion. When performed manually, the procedure suffers when the surgeon traumatizes surrounding tissues and cuts too deep causing bleeding. The robot is perfectly poised to accomplish such a task, however, as it can be programmed to travel along a route or have a virtual barrier beyond which it cannot go.
Image 2: Again, the lens is placed onto the eye to allow a clear view of the trabecular meshwork. In this image, the robot has engaged the trabecular meshwork with the hook-shaped aspect of the blade and is removing it. Through our modifications of the robot, we have been able to achieve extreme angles of reach within the anterior chamber using the KDB. Almost 180 degrees can be treated with a single sweep. Most surgeons can only do 90 to 120 degrees manually. Not only can the surgeon achieve greater reach and maneuverability but can also pause and focus on re-adjusting the lens to maintain a clear view. Once readjusted, the surgeon can pick up right where they left off to complete the procedure because the robot kept the device in the exact same place.
