As New York Eye and Ear Infirmary of Mount Sinai (NYEE) redraws its operational blueprint to meet the demands of a pandemic-driven world, it remains more committed than ever to expanding its educational program for ophthalmic residents and fellows—one of the largest and most respected training initiatives in the country.
“Education is basic to our mission of providing outstanding clinical care, and for that reason, our program to train the next generation of ophthalmologists will not only remain a top priority for New York Eye and Ear, it will continue to grow and improve in the years ahead,” says Paul A. Sidoti, MD, Deputy Chair for Education and Site Chair of Ophthalmology for NYEE.
There is no better marker of that commitment than the novel Joint Internship Program, which notched its first anniversary in July 2021. A special curriculum was developed for the 10 participating students, whose one-year internship at Mount Sinai Beth Israel now includes nine months of general medicine and three months of ophthalmology training at NYEE. According to Harsha S. Reddy, MD, Ophthalmology Residency Program Director and Site Director for Oculoplastics, Orbital, and Reconstructive Surgery at NYEE and Mount Sinai Beth Israel, that tailored curriculum teaches students the basics of the ophthalmic exam and exposes them to each of the subspecialty clinics at NYEE, as well as the Jorge N. Buxton, MD, and Douglas F. Buxton, MD, Microsurgical Education Center.
“We saw dramatic evidence of how these trainees were able to develop their skills in just three months here, prior to starting their first year of residency,” says Dr. Reddy. A number of trainees, he adds, took the Joint Internship Program a step further by using it as a platform to begin research projects.
Change is also critical to the future of the Buxton Microsurgical Education Center, where students learn and practice in a wet-lab setting the intricate microsurgical skills they’ll soon bring to patients in the operating room. Under way are sophisticated audio-visual improvements to this premier site. Specifically, high-resolution video cameras are being installed at four of the wet lab’s 16 microscope-equipped training stations, allowing residents to tape their practice sessions and then relay them to faculty members to review and critique synchronously or at a later time. By the same token, the new capabilities will allow faculty to videotape surgical procedures and techniques in the lab, then store them in an online library for ready access by residents as part of their surgical training.
“The AV upgrades will allow us to formally integrate lab activity into the curriculum,” explains Douglas F. Buxton, MD, Clinical Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai, and son of Jorge N. Buxton, MD, the first chief of cornea service at NYEE and a champion of modern microsurgery. “The new ‘smart’ cameras are connected to the internet, which will make it possible to stream real-time lab activity to any location. And that creates the opportunity for worldwide educational classes from NYEE.”

A dry-lab session, part of the AUPO SCOR skills transfer course at NYEE, with trainees practicing advanced anterior segment skills

(see caption 1)
Technologically, the Buxton lab is already among the leading ophthalmic surgical training sites in the country. In 2006, a virtual reality EyeSi Surgical simulator was installed, enabling ophthalmologists-in-training to experience simulated surgery for development of hand-eye-foot coordination before transitioning to the operating room. And recently, the country’s first robotic assistant for ophthalmic microsurgery entered the lab, where residents and fellows will soon have the unique opportunity to train virtually on the device through special curricula created for retinal and glaucoma surgery.
In acknowledgment of the stature NYEE’s training program has achieved, the Association of University Professors in Ophthalmology (AUPO) used the specialty hospital’s campus as a beta site in June 2021 for honing advanced cataract surgery skills and techniques. The program, known as SCOR (Surgical Curriculum for Ophthalmology Residents), brought together 15 residents throughout the New York metropolitan area for a combination of online and hands-on training prior to rolling out the first wet lab course to 74 third-year residents at a AUPO-sponsored event in the fall of 2021. “The small scale wet lab we held at NYEE generated very positive feedback from trainees and faculty alike, and that’s enabling us to further improve the curriculum to ensure the best possible training experience for residents,” says Steven Feldon, MD, MBA, Executive Vice President of AUPO.
Another significant training-related event has been NYEE’s implementation of the Ngenuity® 3D Visualization System. This state-of-the-art technology provides surgeons with enhanced magnification, detail, and depth perception for visualizing the internal structures of the eye. Instead of peering through a microscope during surgery, ophthalmologists put on special 3D glasses and look at an 80-inch, high-definition video monitor that projects three-dimensional images of the eye in real time. By allowing trainees to view the fine detail of what the surgeon sees in the OR, the 3D Visualization System constitutes a groundbreaking teaching tool at NYEE.
“The Ngenuity system speaks to our commitment to innovation and staying in the forefront of surgical technology,” says Dr. Sidoti. “And just as importantly, it speaks to our continued emphasis on education as the most powerful pathway to those goals.”
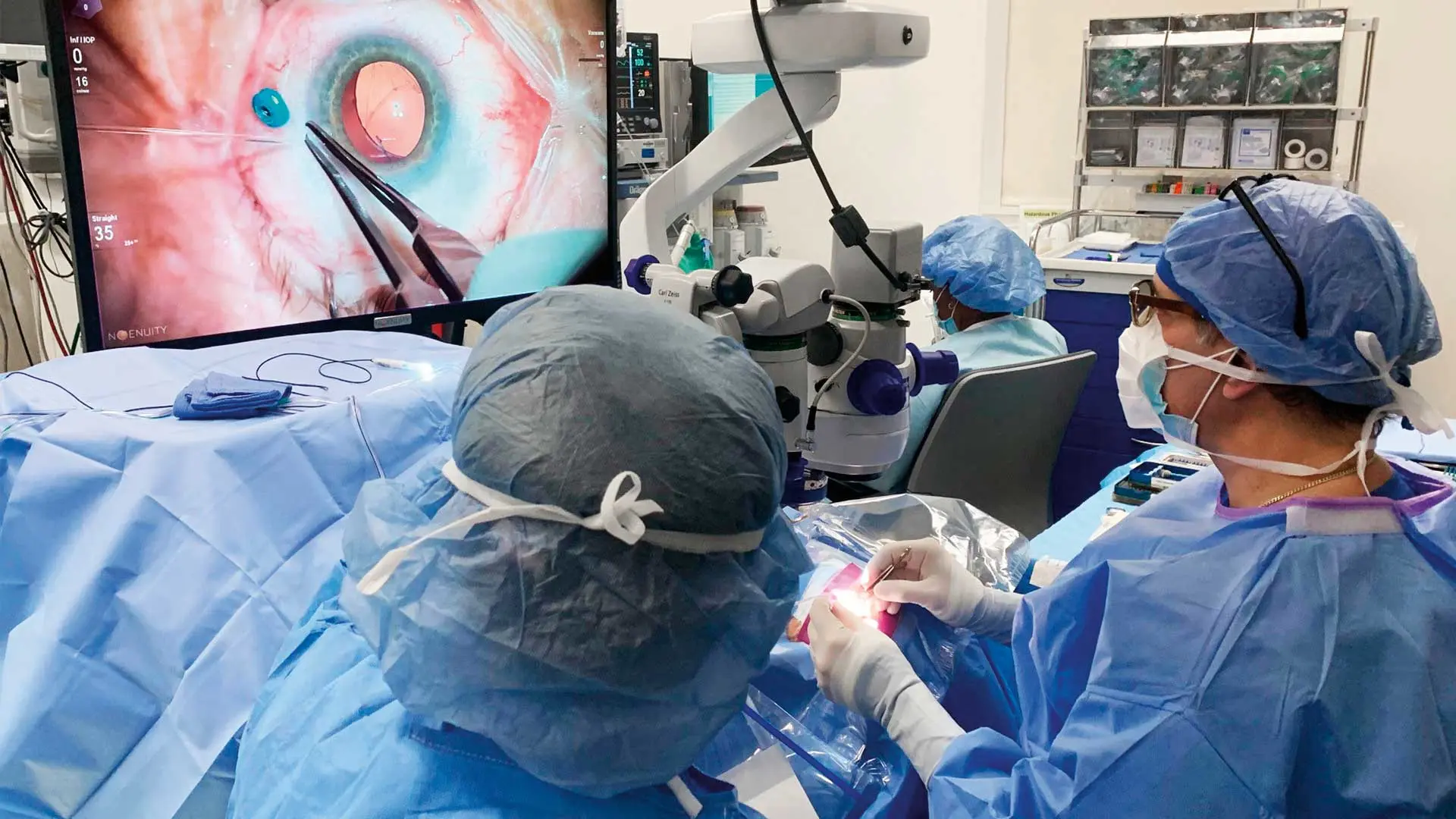
Ronald Gentile, MD, a retina specialist, performing vitrectomy surgery using the Ngenuity 3D Visualization System
