A 2024 study by Mount Sinai researchers shows a link between prediabetes among young people and adverse pregnancy outcomes later in life. The findings could alter how doctors routinely screen or counsel youth on blood glucose levels, and minimize potential maternal and neonatal risks, says corresponding author Katharine McCarthy, PhD, MPH, Assistant Professor of Population Health Science and Policy, and Obstetrics, Gynecology and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
“The lack of uniform preconception prediabetes treatment guidelines for adolescents may represent a missed opportunity to avert pregnancy-related complications,” Dr. McCarthy says. “Our results support expanded preconception hemoglobin A1c screening as a mechanism to intervene on excess cardiometabolic risk earlier in the life course.”
In the study, which was published in JAMA Network Open in September 2024, Mount Sinai researchers examined the significance of prediabetes prior to conception among adolescents and young adults, a group that is most at risk of unplanned pregnancy. The retrospective cohort study of more than 14,000 people between ages 10 and 24 years was generated by linking New York City birth registry, hospital discharge, and A1C Registry data between 2009 and 2017. The study included individuals who had no history of diabetes and at least one hemoglobin A1c (HbA1c) test prior to first birth. In the cohort, 5,896 (41 percent) were Hispanic, 4,149 (29 percent) were Black, 2,583 (18 percent) were white, 1,516 (10.6 percent) were Asian, and 185 (1.3 percent) had other or unknown race and ethnicity.
“The lack of uniform preconception prediabetes treatment guidelines for adolescents may represent a missed opportunity to avert pregnancy-related complications.”
Katharine McCarthy, PhD, MPH
Preconception prediabetes was associated with slight but significant increases in the likelihood of a hypertensive disorder of pregnancy and other adverse outcomes.
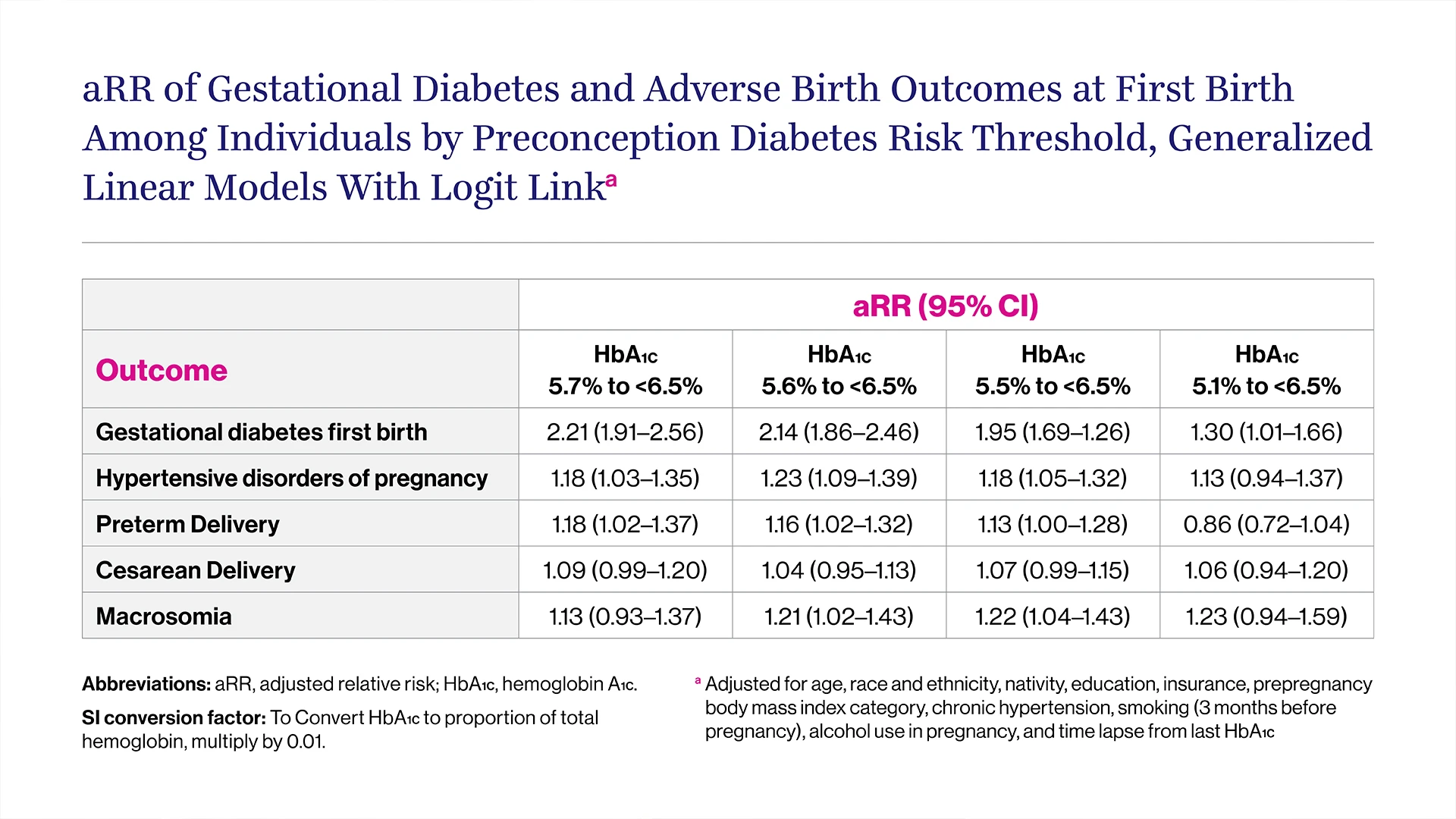
The primary outcome was gestational diabetes at first birth. Secondary outcomes included hypertensive disorders of pregnancy, preterm birth, Cesarean delivery, and macrosomia. Log binomial regression was used to estimate the relative risk (RR) of gestational diabetes at first birth by preconception HbA1c level, adjusting for prepregnancy characteristics. The researchers found that preconception prediabetes was associated with more than twice the likelihood of gestational diabetes at future first birth, with an adjusted RR of 2.21. The experts discovered that prediabetes during youth and adolescence could result in an 18 percent increased risk of hypertensive disorders during pregnancy, such as gestational hypertension and preeclampsia, or preterm delivery.
The study also assessed what level of hemoglobin A1c was most predictive of gestational diabetes at first birth among adolescents and young adults. The optimal threshold was slightly lower for young people than that used for adults (5.6 percent vs. 5.7 percent). Overall, the study results support the need to establish clear clinical guidance on how to screen and counsel young people who currently have elevated blood glucose levels without other risk factors, the researchers said.
The team will next investigate potential school policies and interventions that could reduce risks for heart and metabolism-related conditions in adolescence, and may benefit pregnancy and health outcomes across the lifespan.
Researchers from the Columbia University Mailman School of Public Health, the New York City Department of Health and Mental Hygiene, and the Department of Maternal and Fetal Medicine at Stamford Hospital contributed to this study. The research was supported by grants (R01DK134725, R21DK122266, and UL1TR004419) from the National Institutes of Health.
