The Mount Sinai Health System is achieving improvements in patient outcomes within the Department of Obstetrics, Gynecology and Reproductive Science through an innovative data dashboard, with the additional goal of sharing the fundamentals of this initiative and highlighting the benefits of the dashboard.
Invited by the Joint Commission, a team from Mount Sinai in May 2024 presented an Accelerate Performance Improvement webinar titled “Driving Clinical Transformation for the Safe Reduction of Cesarean Birth (C-Birth) Rates.” The presentation outlined the development of Mount Sinai’s data-driven infrastructure and focused on its success in identifying and addressing disparities in the Nulliparous Term Singleton Vertex (NTSV) C-birth rate and vaginal birth after Cesarean (VBAC) rate.
“We know that severe maternal morbidity is closely linked with Cesarean births, which have been on the rise nationally,” says Toni A. Stern, MD, MS, MBA, Vice Chair of Quality and Clinical Transformation in the Department of Obstetrics, Gynecology and Reproductive Science. “We believe that quality care is equitable care that results in an exceptional patient experience. That led us to take a critical look at the care we provide at Mount Sinai to better understand the disparities that exist and how we could address those for the benefit of our patients.”
Mount Sinai is engaged in a systemwide effort to integrate quality, equity, and the patient experience through the combined work of offices including Enterprise Reporting and Data Stewardship, the Institute for Health Equity Research, and the clinical data operations team within the Office of the Chief Medical Officer.
The Obstetrics Clinical Measures Overview Dashboard has played a key role in these equity and quality improvement efforts since its launch in 2019. It provides real-time access to comprehensive obstetrics and gynecology outcome data, including delivery type, obstetric comorbidity index, and severe maternal morbidity rates, that are searchable and customizable based on sociodemographic factors and quality measures. Data transparency, which facilitates the identification of disparities, fosters continuous improvement and promotes greater reliance on data-informed decision-making.
Obstetrics Clinical Measures Overview Dashboard presents timely data to providers.
In the presentation to the Joint Commission, Alana Noble, MBA, Director of Clinical Data Operations, Mount Sinai Health System, outlined the development of this data infrastructure. “We present accurate and timely data to allow our providers to identify and address disparities, and achieve the best possible health outcomes for our OB/GYN patients,” Ms. Noble said. She added that creating such a data-driven infrastructure is an achievable goal for most health systems.
Within the Mount Sinai Health System, data demonstrated that at the baseline in 2021, Black patients had the highest NTSV C-birth rate (38.9 percent) and lowest VBAC rate (13.2 percent). Over the next two years, VBAC rates increased for all groups. Although Black patients consistently had lower rates compared to other groups, the overall VBAC rate improved to 19.3 percent by 2023, with the rate doubling among Black Medicare/Medicaid patients over the two-year period. However, trends during this time revealed that the highest NTSV C-birth rates were consistently observed among Black patients across all payor groups—commercial and Medicare/Medicaid.
“The transparency of our data extends to everyone, from the care providers who are performing deliveries to the interdisciplinary team,” Ms. Noble said. “With access to metrics by provider, such as NTSV C-birth rates, length of stay and breastfeeding rates, they can monitor their performance, and that of their peers, and work to achieve the best possible outcomes for patients through a health equity lens.”
In the presentation, a pilot initiative focused on improving NTSV C-birth rates was outlined by Desmond Sutton, MD, Site Director of Obstetric Quality and Patient Safety, and Medical Director of Labor and Delivery, Mount Sinai West, and Assistant Professor, Obstetrics, Gynecology and Reproductive Science, Icahn School of Medicine at Mount Sinai.
“As we are all aware, C-births can be a lifesaving procedure, but they are associated with higher rates of morbidity and mortality in the overall population and affect the short-term and long-term health outcomes for many of our patients,” Dr. Sutton said. “And we know that a lower C-birth rate typically indicates evidence-based management of labor and overall good quality of care.”
During the pandemic, Mount Sinai West experienced an increase in C-birth rates, as did many hospitals nationally, Dr. Sutton said. The rate remained high after the pandemic.
“In the first quarter of 2023, our site’s NTSV C-birth rate was 32.5 percent, and we expanded our strategies for improvement,” Dr. Sutton said. This included lectures for OB/GYN physicians and nurses, and an email newsletter that focused on quality, safety, and the NTSV C-birth rate. In a nursing-driven “peanut ball initiative,” the site partnered with an organization called Premier Birth Tools, and nurses were trained in patient positioning utilizing a peanut-shaped exercise ball to obtain positions that helped alleviate pain and accommodate fetal movement into the birth canal.
The dashboards provided the opportunity for physicians to review their data. One-on-one discussions were held with physicians with an NTSV C-birth rate of 35 percent or higher, focusing on the evidence-based management of labor. Providers who had rates that were less than 35 percent but above the overall Health System goal of 26 percent received the same information but in specialized emails.
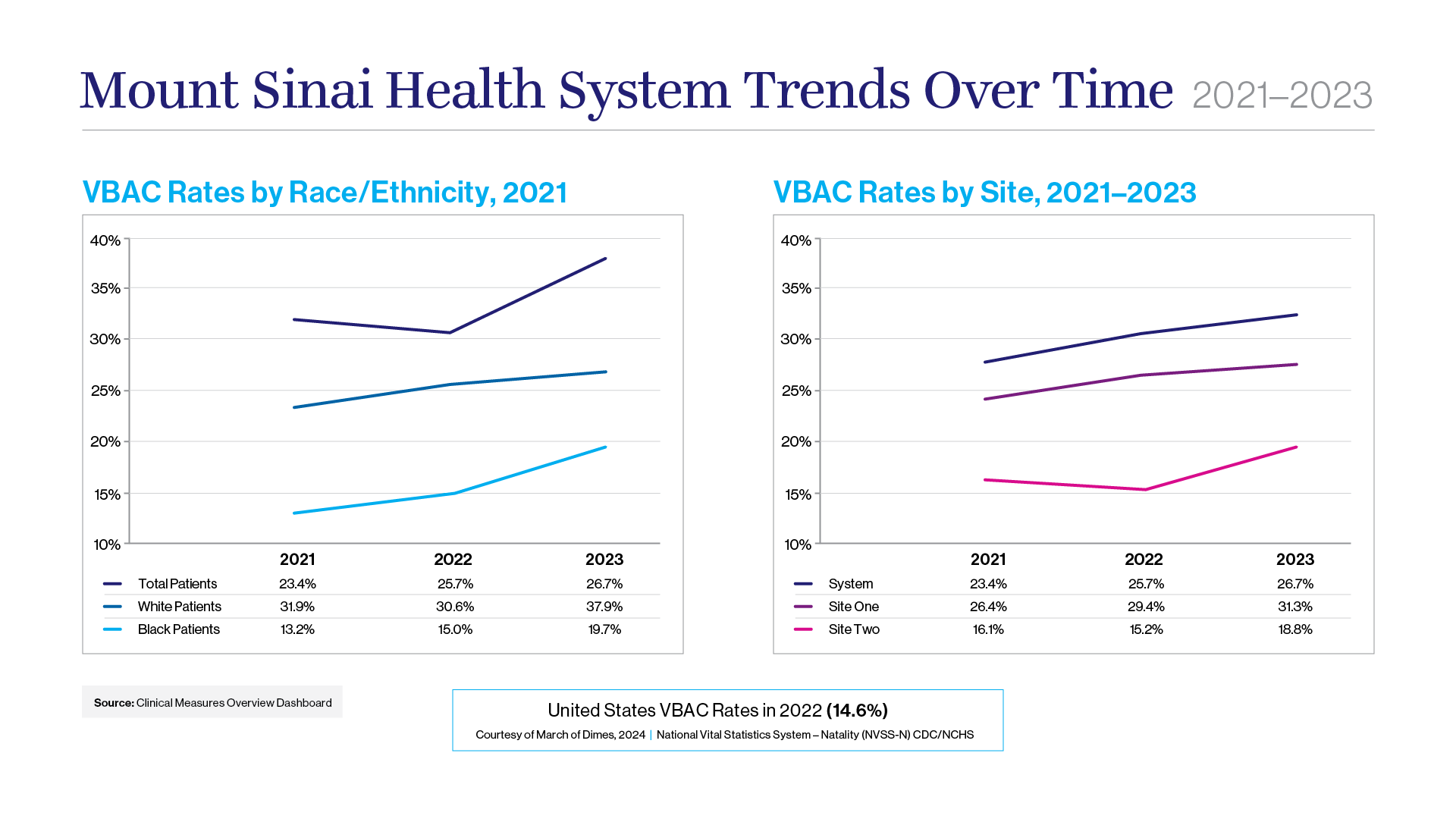
VBAC rates increased over time for all race/ethnic groups. Black patients consistently showed lower rates compared to other race/ethnic groups. However, VBAC rates for Black Medicare/Medicaid patients doubled between 2021 and 2023.
The effort achieved significant success by the first quarter of 2024. Among 11 providers with high NTSV C-birth rates, 8 showed improvement. For the site overall, the rate fell to 26.7 percent, exceeding the initial goal of reaching 29 percent by the third quarter of 2024.
Going forward, the Health System is dedicated to a culture of continuous improvement. This includes launching a patient education platform—available online and in print—and a remote blood pressure monitoring pilot project aimed at high-risk patients. “Controlling blood pressure increases the likelihood of a vaginal birth as well as contributing to a healthier pregnancy overall, even if they have a Cesarean,” Dr. Stern says.
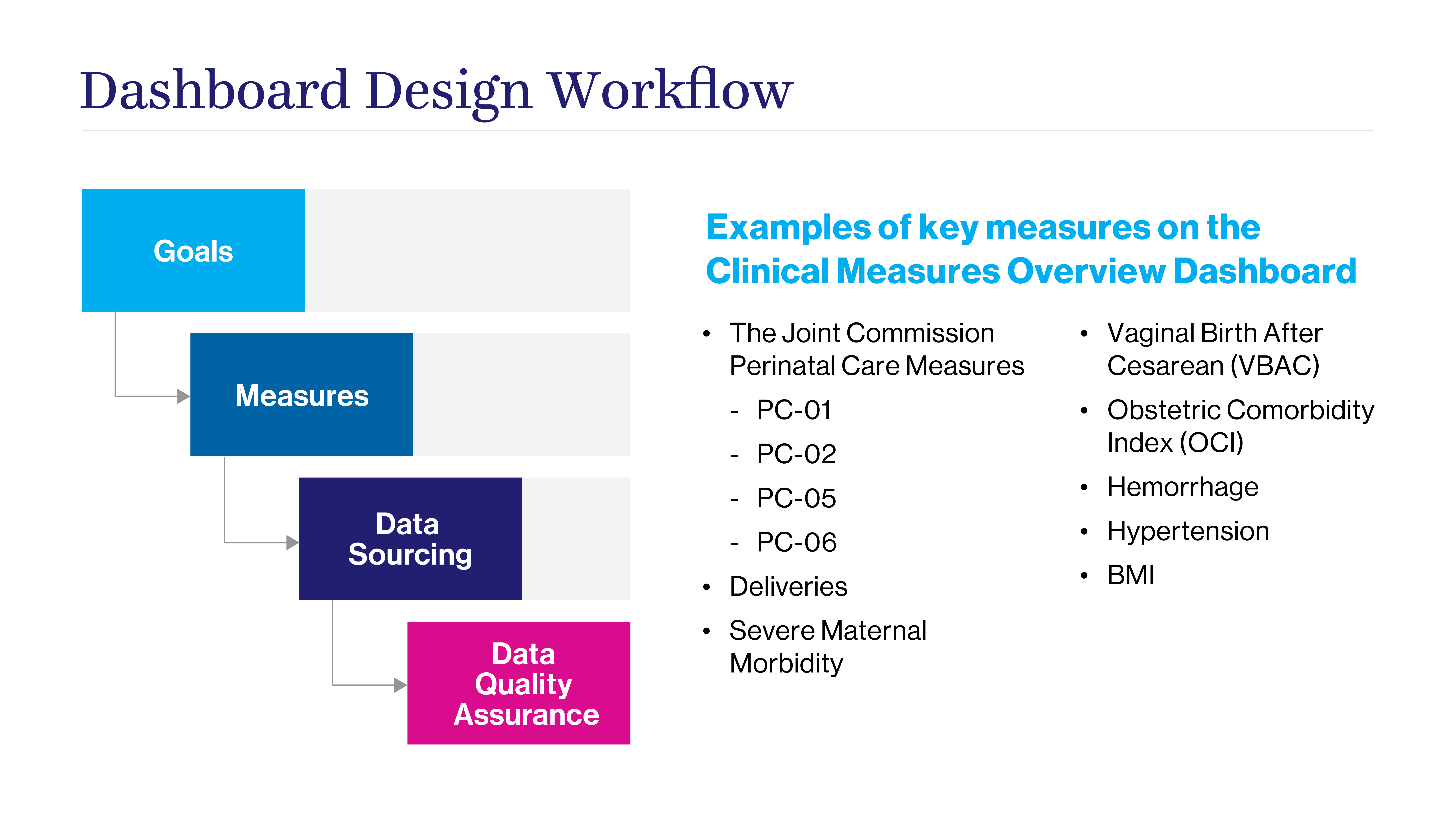
In late 2024, the Department was preparing the next phase of its efforts to address disparities and enhance overall quality of care. There are plans to implement doula support for patients, which has been linked to optimizing health equity and outcomes. But the data dashboard remains a major driver of progress, and Dr. Stern believes the model developed at Mount Sinai could easily be adopted by other academic health care centers. The key, she says, is to bring together front-line leadership stakeholders, along with data engineers and analysts, to establish goals, metrics, data sourcing, and quality assurance measures.
“We recognize that this is going to be a long journey and that our targets are not going to be realized in a year or two,” Dr. Stern says. “The data we gather along the way will be crucial in identifying the areas where we are seeing improvements and where recalibration is required.”
Register to view the webinar “Driving Clinical Transformation for the Safe Reduction of Cesarean Birth Rates” here.

From left, Toni Stern, MD, MS, MBA, Alana Noble, MBA, and Desmond Sutton, MD.
