Low-dose vaginal misoprostol is a safe and effective method for cervical ripening to induce labor in outpatient settings, according to a systematic review led by Joanne Stone, MD, Chair of the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
“With rates of labor induction increasing, it’s important to know which methods are safest and most effective at shortening the time to delivery,” Dr. Stone says.
More than 27 percent of pregnant patients in the United States had pharmacologically or mechanically induced labor in 2018, compared to less than 10 percent in 1990. In 2018, the results of a randomized trial of induction versus expectant management showed that labor induction resulted in a lower frequency of Cesarean deliveries. Yet while several systematic reviews have summarized the research on outpatient cervical ripening, the studies did not reach a consensus about which methods are safest and most effective.
To address that gap in understanding, Dr. Stone, and Rachel Meislin, MD, Assistant Professor of Obstetrics, Gynecology and Reproductive Science, joined colleagues from multiple institutions to evaluate outpatient methods of cervical ripening in labor induction. Their findings were published in the American Journal of Obstetrics & Gynecology in July 2023.
Dr. Stone, Dr. Meislin, and their colleagues conducted a systematic review and network meta-analysis to assess the safety and efficacy of the most common methods for outpatient cervical ripening. Their analysis included data from 42 randomized controlled trials, which included 6,093 patients. Using a network meta-analysis approach enabled the researchers to make indirect comparisons across trials, allowing for a more comprehensive assessment of the various cervical ripening methods in clinical use.
“By using this outpatient protocol for cervical ripening and labor induction, women with low-risk pregnancies can get closer to labor while in the comfort of their homes, without an increased risk of C-sections.”
Joanne Stone, MD
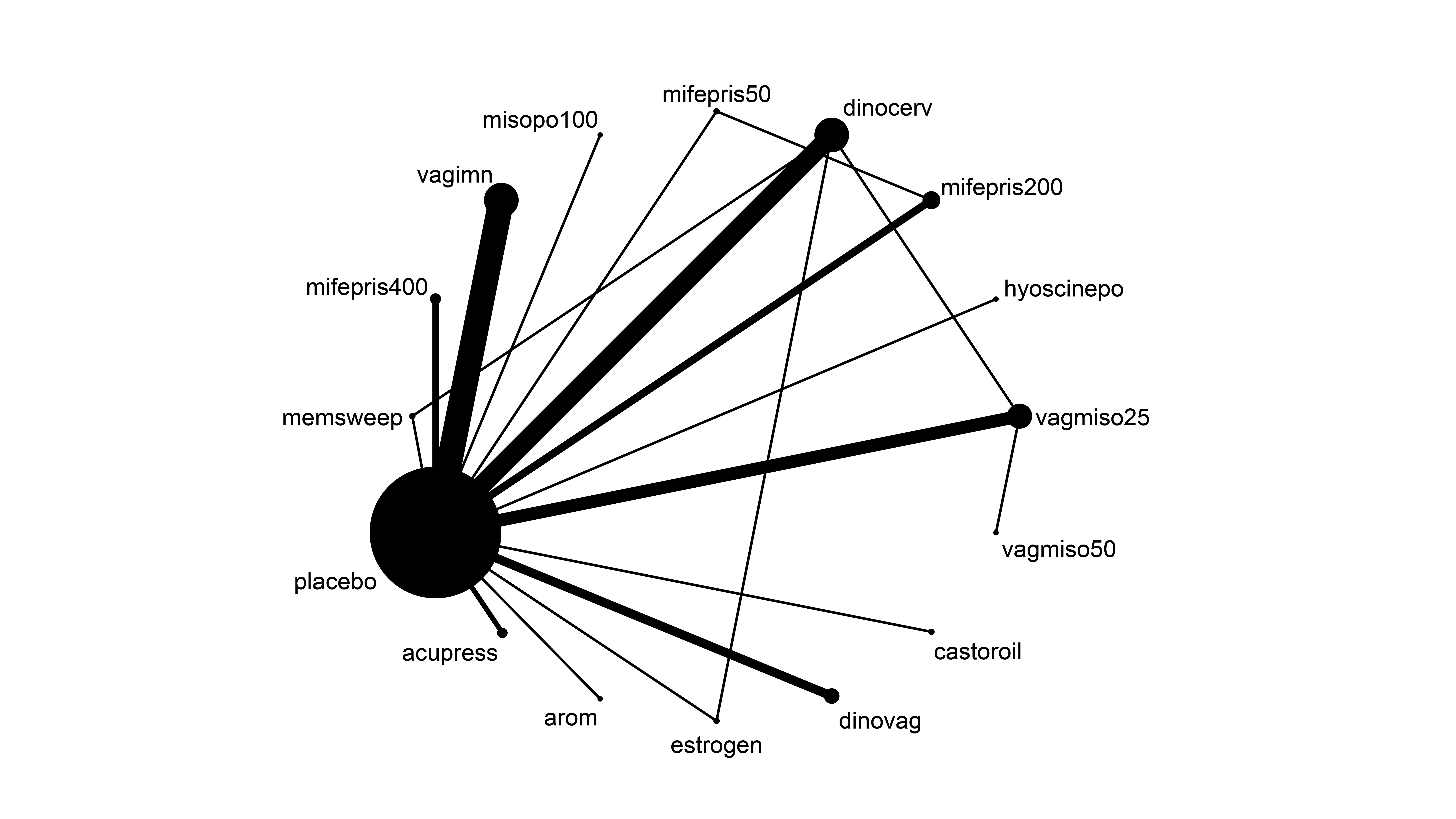
A comparison of pairs of intervention for cervical ripening in a network meta-analysis.
Those methods included acupressure, amniotomy, castor oil, cervical dinoprostone, vaginal dinoprostone, vaginal estrogen cream, oral hyoscine, sweeping of membranes, 200 mg oral mifepristone, 400 mg oral mifepristone, 50 mg oral mifepristone, 100 μg oral misoprostol, primrose oil, vaginal isosorbide mononitrate, 25 μg vaginal misoprostol, 50 μg vaginal misoprostol, and placebo or no treatment.
Across the methods studied, the researchers found that 25 μg of vaginal misoprostol was most effective in reducing the time from intervention to delivery. Importantly, that protocol did not increase the odds of undesirable outcomes such as cesarean delivery, the need for additional ripening methods, the incidence of a low Apgar score, or uterine hyperstimulation. The team’s analysis also showed that, among the effective methods, 50 mg of oral mifepristone was associated with the lowest odds of Cesarean delivery.
They found that acupressure, castor oil, and primrose oil were the least effective methods in reducing the time to delivery interval and were least effective in reducing rates of cesarean delivery.
Misoprostol is often used off-label for induction in labor and delivery suites, typically in doses of 25 μg to 50 μg. The results of the new analysis indicate a greater role for vaginal misoprostol in the outpatient setting. The researchers also found some evidence to suggest that misoprostol combined with a transcervical Foley catheter may further reduce time to delivery. However, they concluded that more research is needed to evaluate the combined use of those methods.
Dr. Stone is a well-known maternal-fetal medicine expert, and she leads a broad research program focused on improving outcomes in areas such as labor induction, ultrasound, and multifetal pregnancies. “This latest finding provides an evidence-based approach that will support physicians in making the best decisions for their patients,” Dr. Stone says.
“Our analysis indicates that 25 μg of vaginal misoprostol is preferred for its safety and efficacy,” she adds. “By using this outpatient protocol for cervical ripening and labor induction, women with low-risk pregnancies can get closer to labor while in the comfort of their homes, without an increased risk of C-sections.”
Featured

Farida G. Nentin, MD
Director of The Mount Sinai Hospital Obstetrics and Gynecology Residency Program, Associate Professor of Obstetrics, Gynecology and Reproductive Science

Barbara Deli, MD
Residency Program Director for Mount Sinai West, and Assistant Professor of Obstetrics, Gynecology and Reproductive Science

Katherine Chen, MD
Vice Chair of OB/GYN Education, and Professor of Obstetrics, Gynecology and Reproductive Science, and Medical Education
