Gynecologic oncologists at the Icahn School of Medicine at Mount Sinai in 2023 launched a series of clinical trials to test promising treatments for gynecologic cancers, including antibody-drug conjugates (ADCs), a new and highly targeted approach.
Disease recurrence is a significant problem in gynecologic cancers, says Stephanie V. Blank, MD, Director of Gynecologic Oncology for the Mount Sinai Health System, Director of Women’s Health at the Blavatnik Family Chelsea Medical Center, and Professor of Obstetrics, Gynecology, and Reproductive Science at Icahn Mount Sinai. That is especially true in ovarian cancer, where the majority of patients will experience recurrence.
With each recurrence, the odds that a patient will respond favorably to chemotherapy decrease. “When chemotherapy isn’t working, we need a different approach,” Dr. Blank says. “ADCs give us more options—a new approach that could work when other treatments do not.”
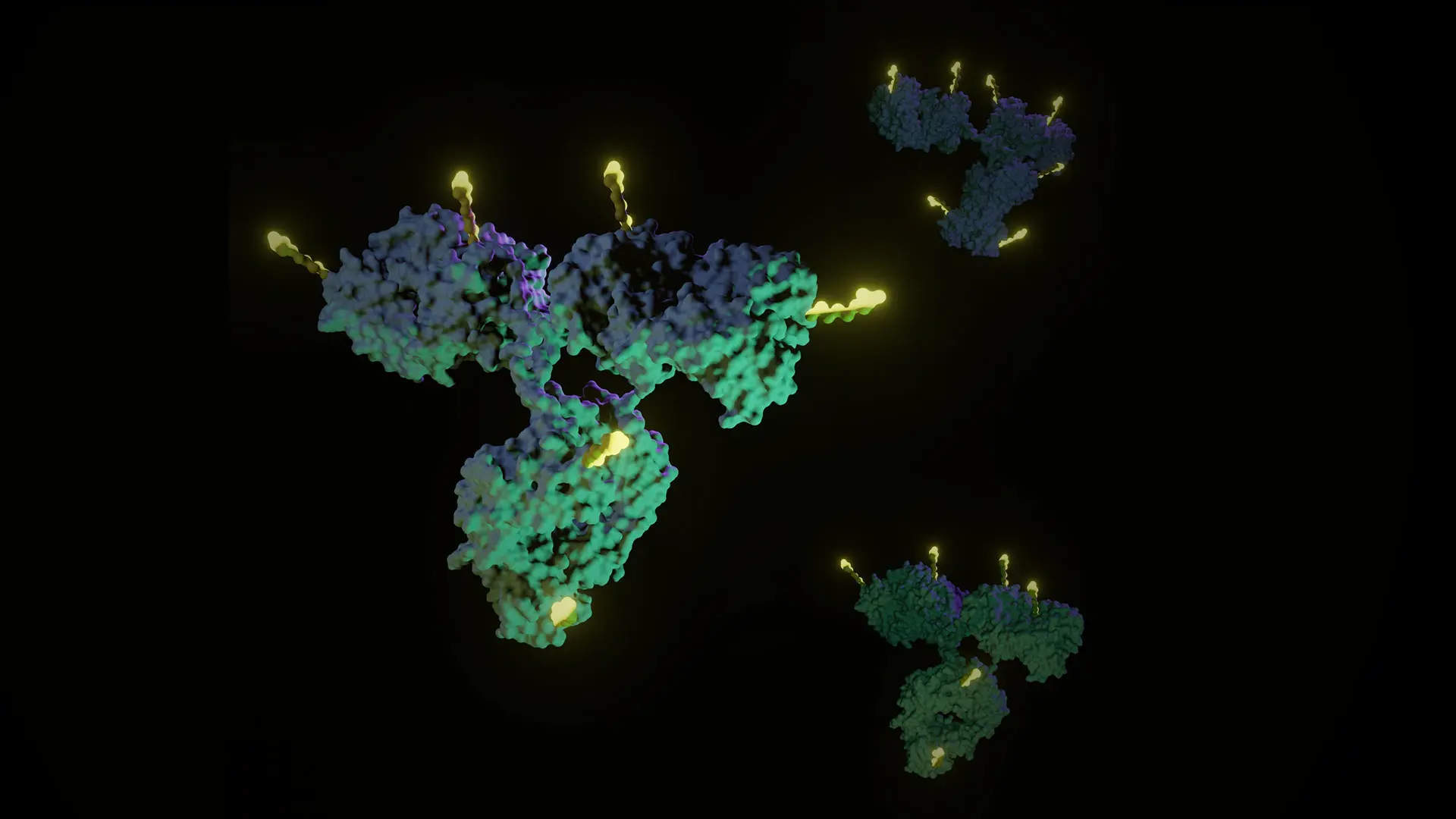
ADCs are targeted molecules designed to deliver a toxic payload into cancer cells by exploiting molecular targets on cells’ surfaces. They have a unique three-part delivery system, Dr. Blank explains. The first part identifies a target antibody or receptor on the surface of the cancer cell. The second component is a linker that holds the molecule together. Once the drug enters the cancer cell, the linker breaks apart, releasing the third element: a toxic payload.
“The drug is very toxic inside the cell. Because it sneaks in while attached to the linker, its toxicity elsewhere in the body is hopefully minimized,” Dr. Blank says. “It’s like a Trojan horse slipping into the cell to deliver a bomb.”
“When chemotherapy isn’t working, we need a different approach. I’m hopeful that ADCs will give us more options—a new approach that could work when other treatments do not.”
Stephanie V. Blank, MD
ADCs have been in development for some time, and they are starting to come into their own. “We’re finding so many uses for them in gynecologic cancer,” Dr. Blank says. In September 2021, the U.S. Food and Drug Administration approved tisotumab vedotin-tftv (Tivdak) for patients with recurrent or metastatic cervical cancer. In November 2022, the agency granted accelerated approval to mirvetuximab soravtansine-gynx (Elahere) for patients with ovarian, fallopian tube, or primary peritoneal cancer who received one to three prior systemic treatment regimens. In both cases, reports showed the drugs increased overall survival—an infrequent and notable finding for these difficult diseases, Dr. Blank notes.
Since 2017, Dr. Blank and her colleagues in the Division of Gynecologic Oncology have offered trials to extend ADCs to more patients with gynecologic cancers. Monica Prasad-Hayes, MD, Associate Professor of Obstetrics, Gynecology and Reproductive Science at Icahn Mount Sinai, has been the principal investigator of Mount Sinai’s trials researching mirvetuximab soravtansine-gynx.
The therapy specifically targets the folate receptor, which is often overexpressed in people with gynecologic cancers. Since its FDA approval, the drug has become the standard of care for patients with recurrent ovarian cancer who are folate receptor-α positive, Dr. Blank says.
GLORIOSA, a multisite trial that launched at the end of 2023, is exploring the treatment as a maintenance therapy in patients with recurrent ovarian, fallopian tube, or primary peritoneal cancer. The phase 3 study will compare mirvetuximab soravtansine-gynx combined with the approved treatment bevacizumab to bevacizumab alone. “By giving patients this drug earlier in their treatment, we can hopefully extend the time between chemotherapy treatments or not need additional treatments at all,” Dr. Prasad-Hayes says.
Dr. Blank is the principal investigator of another trial testing an ADC known as disitamab vedotin, which targets tumors expressing human epidermal growth factor receptor 2 (HER2). HER2 is expressed in a significant portion of ovarian and endometrial cancers, and ADCs with HER2 as a target have been extremely effective in gynecologic cancers in earlier phase studies. This phase 2 study, scheduled to launch in early 2024, will test the drug in patients with previously treated ovarian and endometrial cancers that have recurred.
Meanwhile, Dr. Blank and her colleagues are also co-investigators of an investigator-initiated trial at Icahn Mount Sinai that is scheduled to begin recruiting patients in early 2024. The study will test sacituzumab govitecan-hziy (Trodelvy), which targets tumor-associated calcium signal transducer 2 (TROP2), a cell-surface protein involved in carcinogenesis. The drug is approved for treating bladder cancer and triple-negative breast cancer. Now, the research team will explore its benefit in combination with cisplatin for ovarian and endometrial cancer.
These clinical trials will help build the case for a greater role for ADCs in treating gynecologic cancer and provide hope for patients with recurrent disease. Making clinical trials accessible to all patients is an important mission for Dr. Blank and her colleagues at Mount Sinai, she says. “We pride ourselves on patient access to trials. For years, more than 40 percent of the patients who enroll in our trials have been from minoritized groups,” she adds. As a comparison, an FDA report broke down the subpopulations participating in trials for new drugs (molecular entities and therapeutic biologics) in 2020. They found that 75 percent of participants were white. Just 8 percent were Black, 6 percent were Asian, and 11 percent were non-white Hispanic.
Dr. Blank and her colleagues work closely with Woman to Woman, a mentorship and support group for patients with gynecologic cancers, to educate patients about clinical trials and ensure they have access to transportation, childcare, and other resources that can enable them to participate.
“We work very hard through social services and other programs to recruit a diverse patient population and make sure our clinical trials are accessible to everyone,” Dr. Blank says. “It has been shown that access to clinical trials improves outcomes. We want to improve the lives of all patients with cancer, and it’s exciting to be involved in research that may offer a new avenue for treating gynecologic cancers.”
Featured

Stephanie V. Blank, MD
Director of Gynecologic Oncology, Professor of Obstetrics, Gynecology, and Reproductive Science

Dmitriy Zamarin, MD, PhD
Head of Gynecologic Medical Oncology, Tisch Cancer Institute, Professor of Medicine, Hematology, and Medical Oncology