People who are at higher risk of developing ovarian cancer due to an inherited genetic mutation—often referred to as previvors—are increasingly considering risk-reducing salpingectomy with delayed oophorectomy (RRS-DO), in which their fallopian tubes but not their ovaries are removed, to mitigate their chances of developing ovarian cancer.
The clinical and nonclinical reasons that some people consider this option—which is not currently the standard of care—were explored in a recently published qualitative study led by Stephanie V. Blank, MD, Director of Gynecologic Oncology, Mount Sinai Health System, and Professor of Obstetrics, Gynecology and Reproductive Science, Icahn School of Medicine at Mount Sinai.
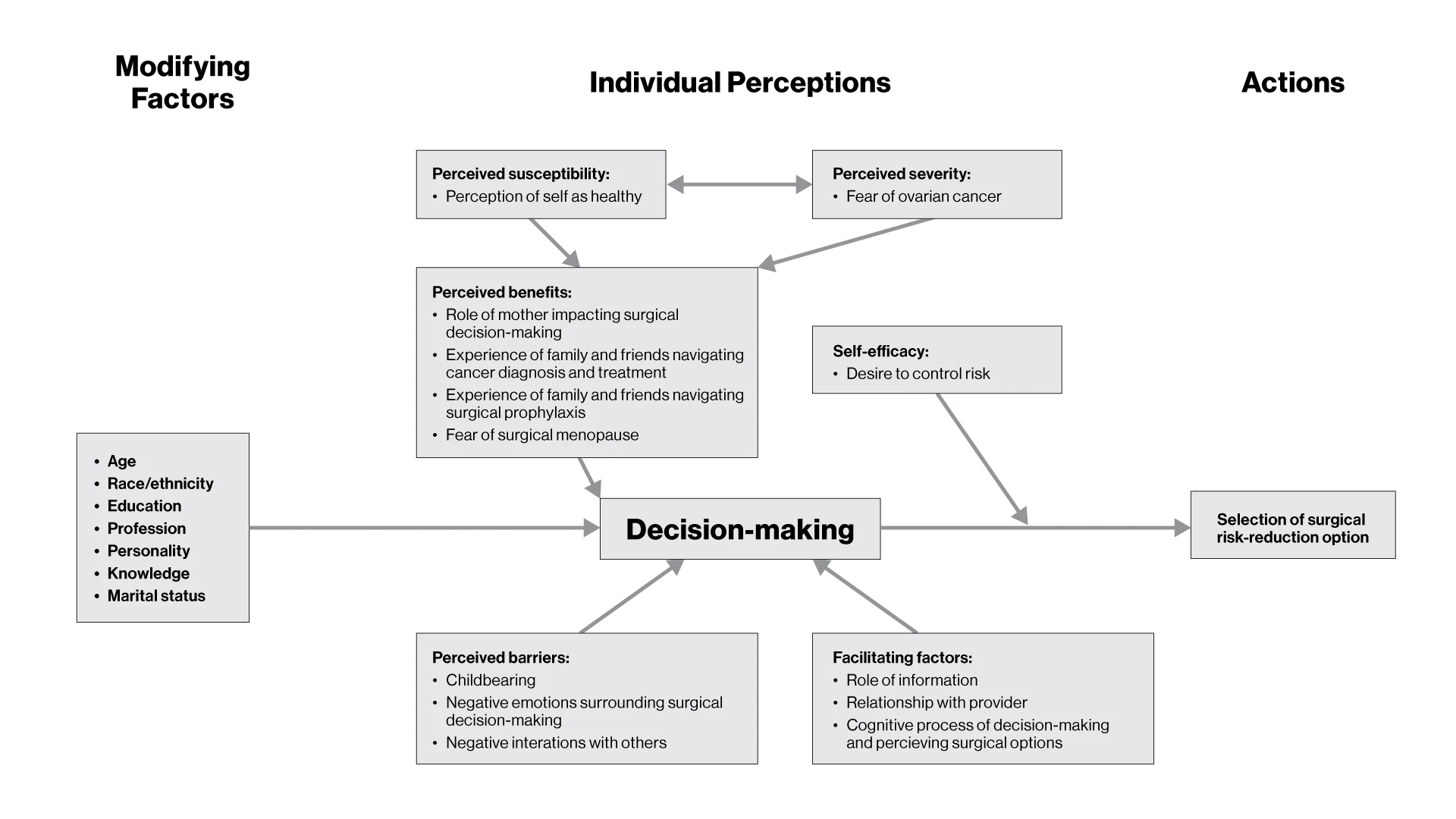
“Our research found that people who chose RRS-DO were primarily influenced clinically by wanting to avoid surgical menopause and nonclinically by their ability to advocate for themselves, as well as their relationship with and trust in their doctors,” Dr. Blank says. “Shared decision-making was also key.”
One respondent explained that when decision-making was shared with her doctor, “then it’s something that you’ve bought into and accepted, as opposed to just being sold on.”
By age 70, people with a mutation in the BRCA1 gene have a 39 to 46 percent risk for developing ovarian cancer, and people with a mutation in the BRCA2 gene have a 10 to 27 percent risk. In comparison, the general population has a lifetime risk of 1.2 percent.
For people with a hereditary breast and ovarian cancer syndrome, the National Comprehensive Cancer Network (NCCN) recommends risk-reducing salpingo-oophorectomy (RRSO), in which the ovaries and fallopian tubes are removed. The NCCN recommends the procedure at ages 35 to 40 for people with a BRCA1 mutation and at ages 40 to 45 for people with a BRCA2 mutation.
Despite these recommendations, many with a hereditary risk are reluctant to undergo RRSO at the recommended age. Recent evidence suggests that BRCA1/2-associated ovarian tumors originate in the fallopian tube, so some providers are now offering RRS-DO, and multicenter trials are investigating the outcomes associated with RRS-DO. Mount Sinai offers patients with BRCA1 mutations RRS-DO or RRSO through this trial. The decision-making that determines whether a patient has the recommended RRSO vs RRS-DO is not well understood.
In the study led by Dr. Blank, interviews were conducted with previvors ages 31 to 46 who had BRCA1, BRCA2, and Lynch-related mutations. Subjects were planning RRS-DO or RRSO, had undergone RRS, or were undecided. Semi-structured interviews were conducted with the previvors and data interpreted through thematic analysis. A universal codebook was applied to all interviews and revised using an iterative approach. Examining codes within and across interviews allowed for major themes and patterns to emerge.
Clinical concerns included the previvors’ perceptions of their personal risk of ovarian cancer and concern about fertility. Nonclinically, the previvors’ family relationships, the availability of data, and feelings of anxiety or empowerment toward the decision-making process were also relevant. Family relationships involved both caring for young children (“I have small children. I want to be around for them”) and watching relatives struggle with ovarian cancer (“This could be my future unless I do something to prevent it”).
Previvors who selected RRS-DO viewed it as a stepwise approach to risk reduction. One respondent explained that after she had a baby, her obstetrician suggested the procedure as a stopgap measure, saying, “Even if you’re not ready to get your ovaries out…you can do this now and then do that a little bit later.”
The findings suggest that improving patient education regarding surgical menopause, understanding previvors’ priorities and experiences, and focusing on communication and shared decision-making could enhance their satisfaction with surgical risk reduction. Previvors stated that experiential knowledge, particularly through the perspective of the gynecologic oncologist, was important, alongside statistical data.
One previvor stated, “I feel like the best perspective you can get is from someone like my doctor, who sees so many patients who go through it and sees how it ends up, or like someone who’s had it done themselves. The articles are only so useful.”
The study concluded: “By understanding previvors' priorities and experiences, physicians can better partner with previvors as they navigate their ovarian cancer risk reduction journey. This will ultimately optimize shared decision-making.”
Featured

Michal Elovitz, MD
Dean for Women’s Health Research

Susan Khalil, MD
Assistant Professor, Obstetrics, Gynecology and Reproductive Science
Konstantin Zachashansky, MD
Associate Professor of Obstetrics and Gynecology

Stephanie V. Blank, MD
Director of Gynecologic Oncology, Professor of Obstetrics, Gynecology, and Reproductive Science

Dmitriy Zamarin, MD, PhD
Head of Gynecologic Medical Oncology, Tisch Cancer Institute, Professor of Medicine, Hematology, and Medical Oncology
