High-risk patients traveling from many states for care; physicians wary of supplying reproductive health information; medical students, providers, and advocates searching for ways to help patients get the care they need.
These were some of the stories told in a virtual panel discussion on reproductive health care in the months that followed the Dobbs decision, in which the U.S. Supreme Court overturned Roe v. Wade. The panel, held in November 2022, was sponsored by Mount Sinai's Raquel and Jaime Gilinski Department of Obstetrics, Gynecology and Reproductive Science, and focused on the implications for patients and providers as many states moved to restrict or ban abortion.
The Division of Complex Family Planning is at the center of Mount Sinai’s response to this new landscape. “Complex Family Planning specialists focus on treating people who are at risk for pregnancy complications or have pregnancies that are abnormal, unintended, or unwanted, and frequently present with other health and potentially life-threatening medical conditions,” said Monica Dragoman, MD, Director of the Division of Complex Family Planning, and its fellowship program. “In essence, we are specialist providers of medical and procedural abortion care and pregnancy loss management, who also attend to people's complex contraceptive needs."
The discussion was hosted by Mount Sinai Trustee Susan Cullman, and led by Alexis Zachem, a third-year medical student at the Icahn School of Medicine at Mount Sinai. In addition to Dr. Dragoman, panelists were Joanne Stone, MD, MS, Chair of the Department of Obstetrics, Gynecology and Reproductive Science, and Adam Jacobs, MD, Medical Director of the Division of Complex Family Planning. Excerpts from the discussion are below; a video can be viewed here.
Please define Complex Family Planning, and give us an overview of the Division’s history.
Dr. Dragoman: In the Division of Complex Family Planning, what distinguishes us as subspecialists is that we have to know how to manage medically or surgically complex situations that demand skillful evaluation and the full thrust of hospital-based resources. Our expertise ensures that we can help everyone, especially those who require care that is anything but routine.
The American Board of Obstetrics and Gynecology officially designated complex family planning as a new subspecialty in 2020—a major milestone for our professional community. However, our Department has been home to a Division of Complex Family Planning since 2007 and established a Fellowship Training Program in 2014, a testament to how Mount Sinai is well ahead of the curve in terms of valuing and investing in this type of expertise for our health care community.
Our faculty members model and teach evidence-based practices and are nationally recognized for clinical excellence and dedication to medical education. And our Obstetrics and Gynecology Residency Program has formally trained more than 250 residents during their dedicated Family Planning rotations, making our program one of the country's largest resident training sites. Mount Sinai is home to one of only 28 accredited Complex Family Planning fellowships based at premier academic institutions across the United States—something that we are very proud of.
How does the Division benefit from being a part of the Mount Sinai Health System?
Dr. Stone: In the realm of family planning, the unique aspect that we bring is that we take care of the most complicated cases. Within the Health System and its hospitals, we benefit from the expertise of our colleagues, including anesthesiologists and interventional radiologists, who help us take care of patients who are truly beyond the scope of the typical patients who need general services.
This Division has had a commitment to the care of providing complex family planning services for decades, and we have a reputation for being a leader in this field. Even before the overturning of Roe v. Wade, we received referrals from all over the region and nation to take care of the most complicated patients.
I just want to highlight one more issue. Several months ago, New York Governor Kathy Hochul requested grant proposals for taking care of patients who require reproductive services. Dr. Dragoman, Dr. Jacobs, and the other Complex Family Planning members came up with four different proposals at The Mount Sinai Hospital, Mount Sinai West, Mount Sinai Beth Israel, and Mount Sinai South Nassau, and all four were awarded grants, so it is an incredible testament to the reputation we have earned in this realm.
Dr. Jacobs, could you please explain what we are seeing on the ground? How frequently are we seeing out-of-state care seekers?
Dr. Jacobs: First, I want to go over a bit of what is happening nationally, before I focus on what is going on in New York State and at Mount Sinai.
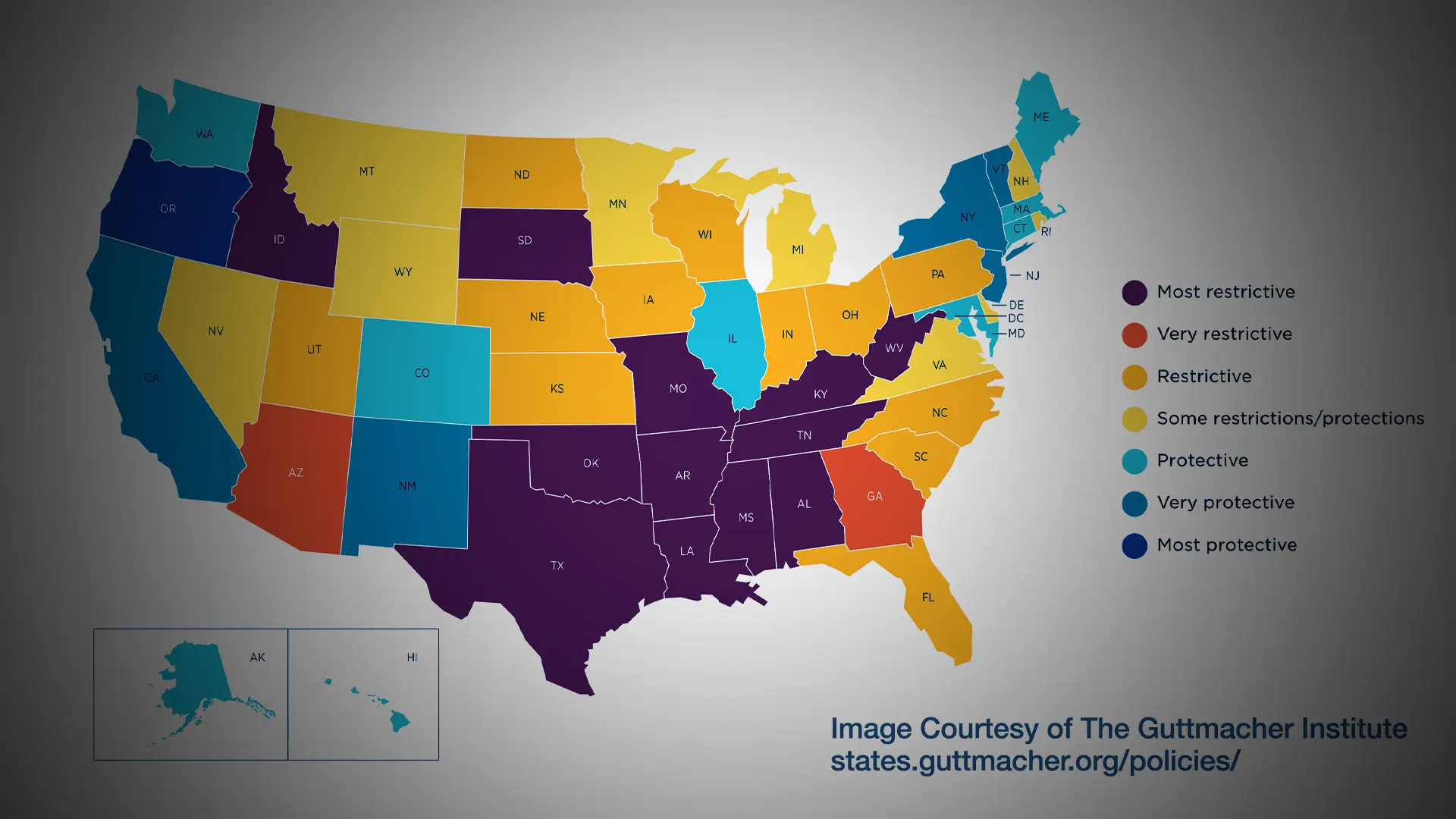
The Guttmacher Institute has been mapping the current state of abortion services in the United States. You will see that 15 states in the United States are not providing abortions, and Georgia provides them only up to six weeks. This is a significant concern, because we know from the data that banning abortion doesn't ultimately decrease abortion, it leads to unsafe abortion and only increases maternal morbidity and mortality.
In the states that are protective of reproductive rights, such as Illinois, North Carolina, Colorado, and New York, we are seeing an increase of 12 percent of cases since Roe has been overturned and people have traveled to seek care.
What we are seeing at Mount Sinai is a reflection of those numbers. We are seeing an increase of out-of-state abortion seekers. This includes patients from Georgia, Florida, Texas, Ohio, and South Carolina. Many of these cases are high-risk patients who need hospital care. Many of these patients are uninsured or underinsured. Or they actually have commercial insurance, and because they have to travel state-to-state, they lose their insurance, and they are in desperate need. Mount Sinai is uniquely prepared to support these patients. We have all of the necessary coverage from other services such as hematology, cardiology, and anesthesia, and we have ICUs and the labor floor for patients who need a labor induction.
What we have seen in recent months is frustrating for so many people, but we are also seeing the community coming together, and this is extremely inspiring. National organizations like the Bridge Alliance, Planned Parenthood, and the Haven Coalition are helping patients pay for travel and housing, and we are figuring out how to work this problem to provide essential health care to patients who need it.
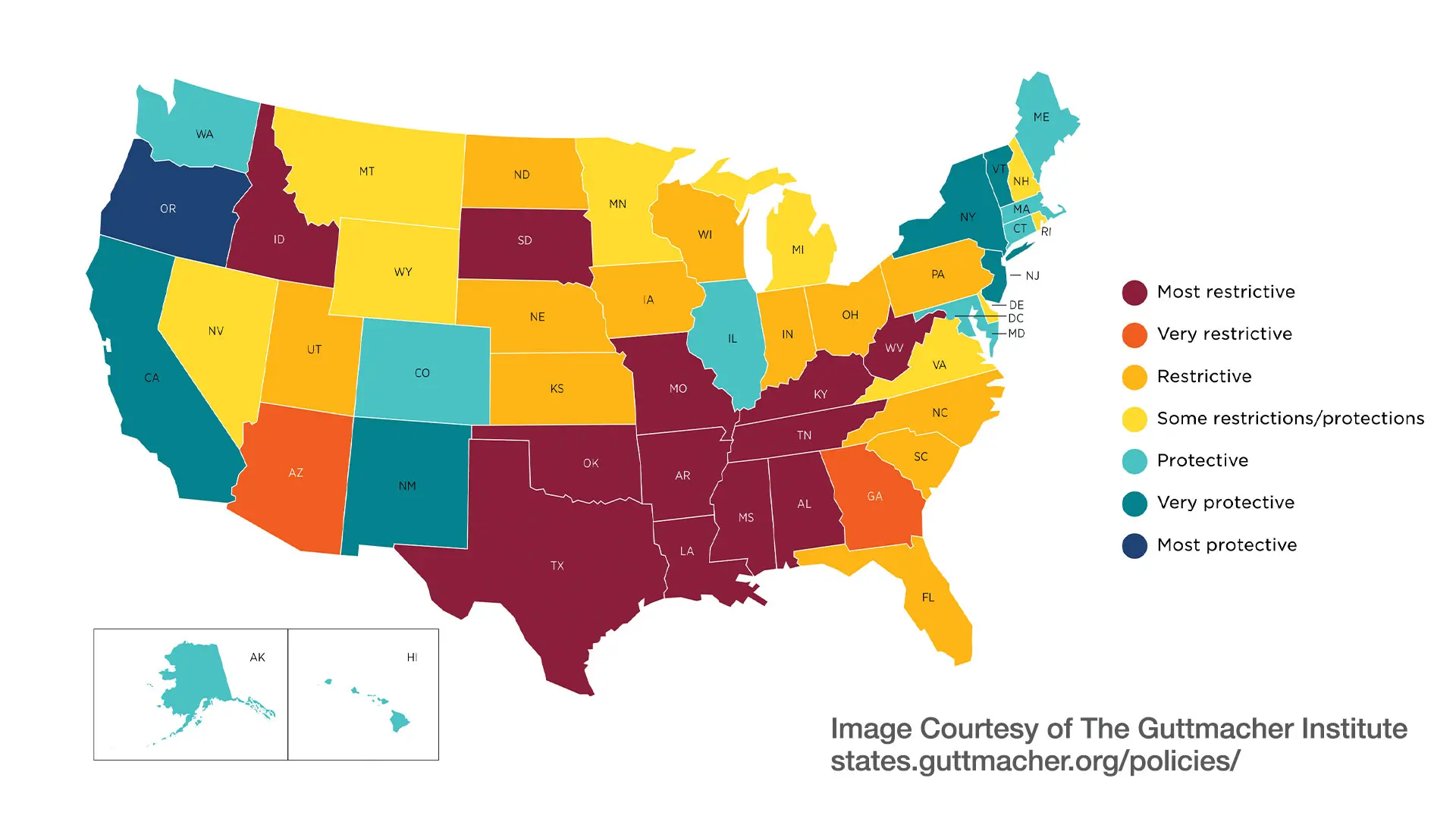
A map reflecting state policies on abortion in effect as of January 29, 2023, according to the Guttmacher Institute.
Dr. Dragoman, in a February panel discussion, you shared the story of a patient of yours from Texas, and I understand that another patient has shared their story with you. Would you be willing to read it to us?
Dr. Dragoman: I think we all can talk about the importance of the care we're providing and what it means for patients, but there really is no substitute for hearing a personal account of what it takes to access essential health care in the times that we're living in right now.
What I’m going to read comes from a recent patient and her partner, who traveled from Georgia to Mount Sinai for an abortion when they learned that their pregnancy was complicated by a fetal anomaly. We have permission to share her story, but I paraphrased a bit of the testimony for time:
“My husband and I both come from families of messy divorces and have dreamed of nothing more than having our own family, our own children. We were married in December of 2021, and in April of 2022, the pregnancy test turned positive. We couldn't wait to share the news; there was so much to look forward to, and we were so excited. At 20 weeks, our amniocentesis results showed we were having a son, but he had a chromosomal deletion. We researched what this could mean as we waited to do a fetal MRI.
The day of our MRI, the doctor showed us the images and highlighted that our son was missing half of his brain and had no nose or bony structure in his face. He would not survive outside the womb, and we needed to make a difficult decision to have a termination or give birth and know he would die in our arms shortly thereafter.
I distinctly remember saying, ‘But we live in Georgia,' and the response being, ‘Yes, I'll text you the national abortion hotline number, but that's all I can do from a resource perspective.’ We had three Georgia providers promise to call or email us with resources that never came. I called locations across New York and Connecticut, knowing that we had at most two weeks before the decision was made for us to carry to term and watch our first child die in pain. Then I called Mount Sinai, and they helped us. They helped us show our son mercy and never having to experience the full pain of this condition.”
One heart-wrenching story—that reflects the experience of patients who are dealing with the realities of the restrictive landscape in real time.
Before moving on, I do want to share some information about an additional resource we have at Mount Sinai that is a real centerpiece for patients in this circumstance—our Perinatal Bereavement Program. This program is designed for women and families who may be struggling with fetal abnormalities, difficult pregnancies, and miscarriage. The program offers individual or couples counseling, support groups, and memorial services. It has been a very special resource at our institution for years, and it is even more important as we're seeing patients in these dire circumstances show up on our doorstep for care.
In-person care is not the only change that we're seeing. How have telehealth services changed recently?
Dr. Dragoman: We have to go back a little bit and appreciate that it all starts with decades of work to develop and refine a variety of medical options for abortion and medical management of pregnancy loss. Methopristone and misoprostol, the medicines we use in combination for this process, are truly the revolutionary reproductive health technologies of our time. Decades of accumulated and abundant evidence demonstrate that early medical abortion is safe and effective when quality medicines are available and accurate information is provided, when medications are used according to evidence-based guidelines, and when systems are in place to recognize and manage the very uncommon complications that can coexist with navigating this process.
If there is one silver lining of the COVID-19 pandemic, it is that it compelled development of more simplified protocols, with fewer exams and tests, to safely offer early medical abortion—without an in-person visit for people who have otherwise uncomplicated care. Truly, through the intersection of circumstance and the dedicated work of clinical researchers, and advocates, we've been able to streamline and advance the protocols and possibilities for people in need of medical abortion.
At Mount Sinai, we have for several years been offering medical abortion via telemedicine to navigate various aspects of that process. In 2023, we plan to pilot a direct-to-consumer telehealth medical abortion model. Effectively, what that means is patients will be able to communicate with a trusted physician when they are looking for medical abortion and be able to consult for their care and receive their medication at home to initiate their procedure in the privacy and convenience of their own house. We are going to be structuring that for patients within the Mount Sinai Health System who are also residents of New York State.
Could you please speak to the impact of the Dobbs decision and future legislation on OB/GYN training programs, and how Icahn Mount Sinai is responding?
Dr. Dragoman: I will say it has put the entire state of training into a place of tremendous chaos. In the mid-1990s the Accreditation Council for Graduate Medical Education made training in abortion and reproductive health services an accreditation requirement for all OB/GYN residencies. Now programs in states where those services are no longer able to be provided are scrambling to figure out appropriate solutions to ensure that their trainees have access to appropriate education and training to be able to fulfill their professional requirements.
There are exciting and creative possibilities on the table. At Mount Sinai, we are exploring possibilities to open up opportunities for training to external rotators who are interested in this—as a one-off opportunity for individuals as well as potential formal partnerships with particular institutions. At the same time, we will continue our current commitment to train 17 residents per year, from our Mount Sinai West and Mount Sinai Hospital residency training programs, as well as our two fellows each year, providing them with the highest quality evidence-based training. Certainly, it's a delicate dance as we are expanding our faculty and also our footprint across the Health System, which will help us both meet our patient care demands as well as expand possibilities for training. This is a core value for all of us and something we are committed to.
Featured

Joanne L. Stone, MD, MS
Chair and Professor of the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology and Reproductive Science
Monica Dragoman, MD, MPH
Director of the Division of Complex Family Planning, and Assistant Professor of Obstetrics, Gynecology and Reproductive Science
Adam Jacobs, MD
Medical Director of the Division of Complex Family Planning, Associate Professor of Obstetrics, Gynecology and Reproductive Science, Pediatrics, and Medical Education