Due to teamwork and technically advanced care at The Mount Sinai Hospital, a 33-year-old patient delivered a healthy, if premature, baby through Cesarean section while on life support for COVID-19 pneumonia.
The journey began in March 2021 when Yesenia Lopez, a police officer, developed body aches and a fever. These symptoms were followed by a cough that quickly progressed to shortness of breath. She took an at-home COVID-19 test, which came back positive. Yesenia and her husband, Martin, drove in the early morning hours from their Rockland County, New York, home to The Mount Sinai Hospital Emergency Department.
The ED doctors agreed that there was cause for concern and called her obstetrician, Francesco Callipari, MD, Assistant Clinical Professor and Vice Chair of Operations, Obstetrics, Gynecology and Reproductive Science at the Icahn School of Medicine at Mount Sinai. “When I first met Yesenia in the emergency room, I could see that she was very, very sick,” Dr. Callipari says. “She was gasping for air, and an X-ray showed she had severe COVID pneumonia." She was admitted to the surgical intensive care unit.
A few hours later, her oxygen level dropped dangerously low. Doctors gave Yesenia supplemental oxygen, but Yesenia was still struggling to breathe, and the baby’s heart started to show areas of decreased oxygenation. Dr. Callipari realized Yesenia might need to be intubated. “We called her husband to come in right away because we had to make some important decisions,” he says. By this point, more than a dozen doctors, nurses, and support staff—from at least seven medical teams—were caring for Yesenia. “It was really touch and go at some points,” says Dr. Callipari. Yesenia was closely monitored by Lauren Ferrara, MD, a specialist in Maternal Fetal Medicine and Assistant Professor of Obstetrics, Gynecology and Reproductive Science at Icahn Mount Sinai, and Dr. Callipari. The two stayed at the bedside for about 10 hours.
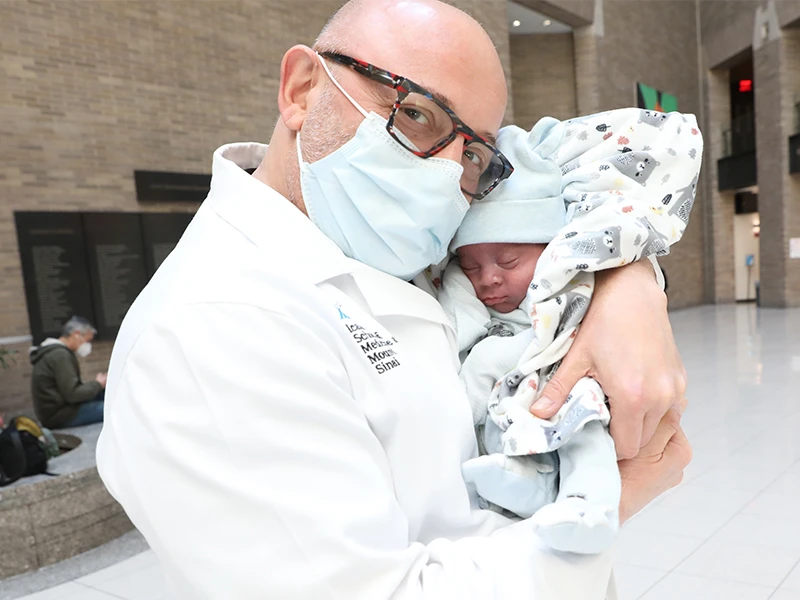
Francesco Callipari, MD, with Elias Lopez in May 2021.

Baby Elias in December 2021.
The baby’s heart rate did not improve. “We decided that it was just safer and more beneficial for Yesenia for the baby to be born early,” says Dr. Callipari. The team considered waiting for natural childbirth, but were concerned that there wasn’t enough time. With Martin’s approval, they elected to do an emergency cesarean section. “Given that her body was having such a hard time delivering oxygen to all the tissues that needed it, including the uterus, the placenta, and the baby, of course, we felt that at that point it was just safer and more beneficial for the baby to be born,” Dr. Callipari said.
“Over the whole time during COVID-19, this was the fastest I had seen a pregnant patient deteriorate,” Dr. Ferrara says. “I am always quite proud of how well all the teams work together, but this day it was exceptional.”
The obstetric anesthesia team placed Yesenia on a ventilator, but it quickly became clear that she still wasn’t getting enough oxygen, says critical care physician Sanam Ahmed, MD, Assistant Professor of Surgery, Icahn Mount Sinai. Dr. Ahmed decided she needed an extracorporeal membrane oxygenation (ECMO) machine.
Dr. Ahmed then called cardiologist Gregory Serrao, MD, Assistant Professor of Medicine (Cardiology), and cardiac surgeon Shinobu Itagaki, MD, MSc, Assistant Professor of Cardiac Surgery. Within minutes, Drs. Serrao and Itagaki were able to take Yesenia to the operating room and place her on ECMO, which helped to stabilize her oxygen levels. Dr. Ahmed says, “It really was amazing that we were able to get her onto ECMO so quickly. This was possible partly because of what Mount Sinai is capable of, and partly due to the great working relationships that were already established among the different services involved in Yesenia’s care.”
ECMO is a technique for providing cardiac and respiratory support to a patient whose heart and lungs are unable to provide enough flow of oxygenated blood to sustain life. It works by withdrawing volumes of blood from the body through large catheters, and running it through the membrane of an external machine to oxygenate red blood cells and remove carbon dioxide. This blood is then returned to the body through another large catheter.
“She was so sick and had such bad consolidation of the lungs—meaning that the spaces were filled with fluid and other material that did not allow for the exchange of carbon dioxide and oxygen—that she needed to be put on ECMO,” Dr. Callipari says. “Only a few medical centers have it for adults. And the Mount Sinai Health System does have it.”
“Take this virus very seriously. It’s very dangerous. My message is to seriously consider getting the vaccine.”
Yesenia Lopez
Very quickly once Yesenia was placed on ECMO, good blood flows were established, and Dr. Callipari and Dr. Ferrara were able to perform an uncomplicated C-section, assisted by Maternal Fetal Medicine Fellow Rachel Meislin, MD. The baby was born at 29 weeks and was immediately taken to the neonatal intensive care unit (NICU), where he spent 20 days feeding and growing. “I think the delivery was a good thing for Yesenia because it helped her body start healing again,” says Dr. Callipari. “She really turned the corner and started getting much, much better.”
The patient spent about a month on ECMO, then her condition improved so markedly that Dr. Ahmed took her off the device and found she could breathe on her own.
Throughout this time, Martin spent his days at The Mount Sinai Hospital, going back and forth between his wife and his baby. Due to COVID-19 safety rules, he could not visit Elias in the NICU, but he could peek in the window and watch his son. “There were so many times that I wished I could trade places with them,” Martin says. He decided not to name the baby until Yesenia had recovered and they could do so together.
When Yesenia came out of the coma and met her son, she and Martin named him Elias. Her recovery was so swift that she left the hospital before the baby did.
Nine months later, Yesenia had not returned to work, but she and Elias were thriving. “He’s getting chunkier,” says Yesenia. She and Martin are grateful to her Mount Sinai health care providers for their compassion and attention. And they learned an important lesson about COVID-19: In the months before Yesenia had the baby, Martin had received his first COVID-19 shot, but Yesenia had decided to wait until after she gave birth, for fear of what effect the vaccine might have on her fetus.
“COVID is a very, very serious illness, especially for pregnant women,” says Dr. Callipari, who advises most of his pregnant patients to get vaccinated. “I really cannot say enough how important it is for pregnant women to really, really strongly consider getting the vaccine.”
Yesenia agrees. “Take this virus very seriously. It’s very dangerous,” she says. “My message is to seriously consider getting the vaccine.”
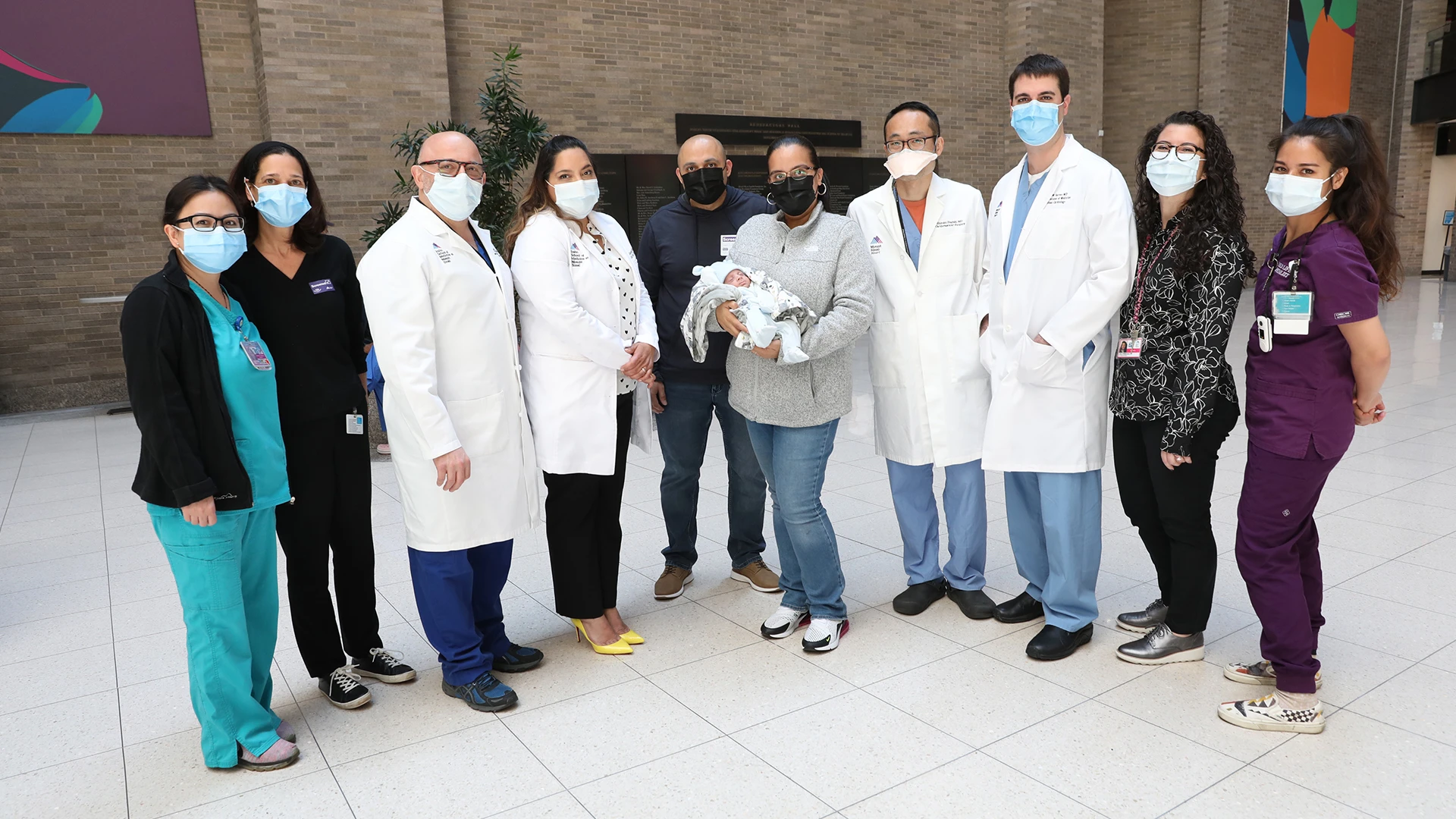
Yesenia, Martin, and Elias Lopez at The Mount Sinai Hospital in May 2021, surrounded by their team, from left: Jannette Valentin, RN; Jill Winston, LCSW; Francesco Callipari, MD; Sanam Ahmed, MD; Shinobu Itagaki, MD; Gregory Serrao; MD; Jenna Mennella, MD ; and Claire Pettengill, Child Life Specialist.
