With a Yale-Brown OCD score of 30/40, his failed treatments included clomipramine, transcranial magnetic stimulation, electroconvulsive therapy, exposure and response prevention, and other pharmacological therapy. DBS for OCD has been approved since 2009 by the U.S. Food and Drug Administration under a humanitarian device exemption.
Brian H. Kopell, MD, Director of Mount Sinai’s Center for Neuromodulation, collaborated on this case with Martijn Figee, MD, PhD, Director of the Mount Sinai Interventional Psychiatry Program. They are part of a large team working within the Nash Center for Advanced Circuit Therapeutics (C-ACT), which was established as a hub to bring neurosurgeons, neurologists, psychiatrists, and psychologists together with neuroimaging specialists, electrophysiologists, data scientists, engineers, and basic neuroscientists to specifically rethink the way neuromodulation treatments are developed, personalized, and delivered to patients. Its founding director, Helen S. Mayberg, MD, is internationally renowned for her study of brain circuits and her pioneering research into DBS, and was recently elected to the National Academy of Sciences.
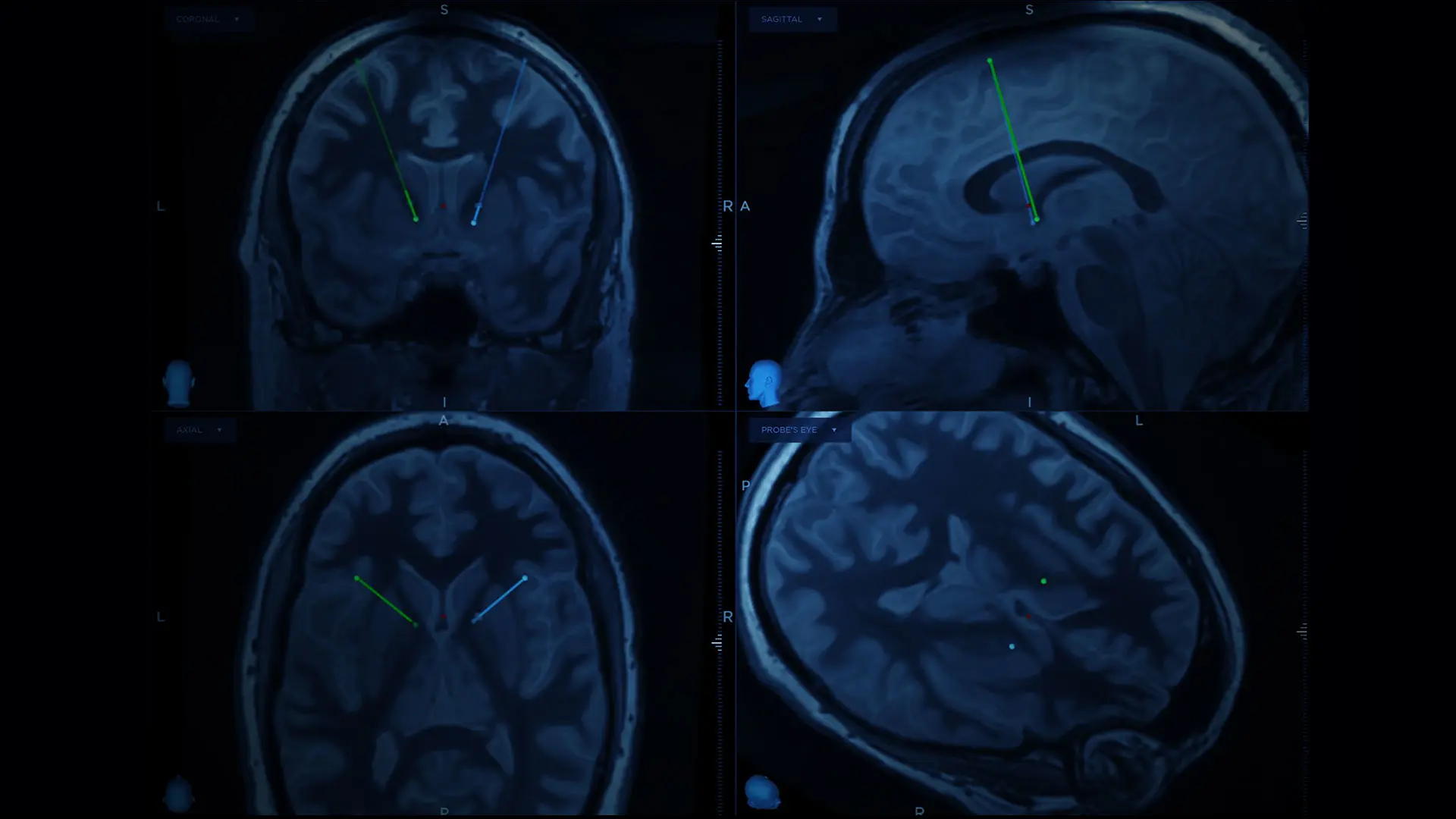
In a narrated video, Drs. Kopell and Figee describe the preoperative planning, the surgical approach, the postoperative programming, and the outcome, which shows at 6-month follow-up the patient is almost free of OCD and has no eye-poking compulsions. Residual habitual rituals persist, they report, but they are shorter and unrelated to obsessions or strong urges.
Watch the video.
Deep Brain Stimulation (DBS) for Obsessive-Compulsive Disorder (OCD)