“Surgeons are natural innovators, constantly trying to improve, with an intuitive sense for how to make surgery safer, more precise, and more effective,” says Benjamin I. Rapoport, MD, PhD, Assistant Professor of Neurosurgery at the Icahn School of Medicine at Mount Sinai, and Scientific Director of Mount Sinai BioDesign. “Our incubator gives them the opportunity to identify areas for improvement, as well as the resources to model and prototype software and devices for further development and commercialization.”
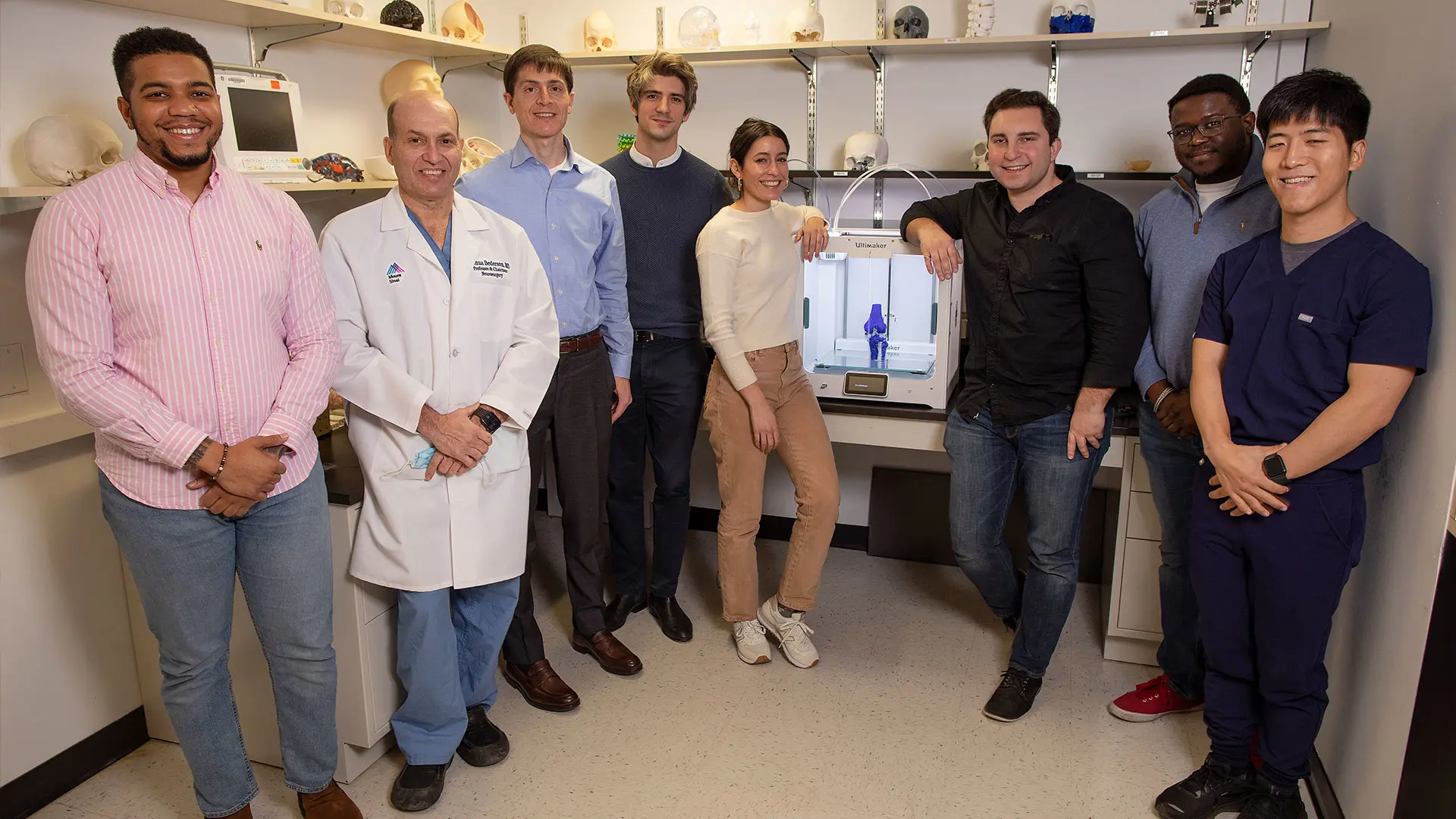
Mount Sinai BioDesign staff from left: Tyree Williams, MEng, Engineering PhD student; Joshua B. Bederson, MD; Benjamin I. Rapoport, MD, PhD; Alexis Bruhat, MEng; Isabella Morgan, BEng; Joseph Borrello, BEng; Denzel Faulkner, Engineering PhD student; and Fred ‘Young Joon’ Kwon, PhD, an MD/PhD candidate.
Dr. Rapoport, an active neurosurgeon, has extensive scientific training, receiving a Master’s degree in Physics from Harvard University; a Master’s degree in Mathematics from Oxford University; a PhD in Electrical Engineering and Computer Science from the Massachusetts Institute of Technology; and his medical degree from Harvard Medical School. He completed his neurosurgery residency, chief residency, and fellowship training in endovascular neurosurgery and endoscopic skull base surgery at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. He has a track record of technology translation in the areas of digital health, including serving as co-founder of Simbionics (acquired by Apple), and of neurotechnology, including serving as a cofounding member of Neuralink.
Coming out of the Department of Neurosurgery’s Neurosurgical Simulation Core, Mount Sinai BioDesign was established in 2018 by Joshua B. Bederson, MD, out of a desire to improve outcomes for neurosurgery patients, first creating virtual anatomical models for use in preoperative planning for complex brain surgeries. Dr. Bederson, the Leonard I. Malis, MD / Corinne and Joseph Graber Professor of Neurosurgery, and Chair of Neurosurgery for the Mount Sinai Health System, eventually transformed Mount Sinai BioDesign into a biomedical incubator now using the most advanced tools and capabilities and drawing on clinical expertise across a wide range of disciplines throughout the Mount Sinai Health System.
“Surgeons stop in throughout the day to talk to engineers and to try out prototypes from our lab. In this kind of environment, product iterations happen within hours or days, not months.”
– Benjamin I. Rapoport, MD, PhD
Among the resources are a full-time team of engineers backed by CAD design and 3D printing and machine prototyping technologies. Significantly, these resources are embedded in The Mount Sinai Hospital, steps away from the operating rooms and interventional radiology suites. “This proximity is intentional. Surgeons stop in throughout the day to talk to engineers and to try out protypes from our lab,” says Dr. Rapoport. “In this kind of environment, product iterations happen within hours or days, not months.”
The two products include:
MitralPrint, an endovascular pressure sensor guidewire to monitor and quantify mitral coaptation force (MCF) intraoperatively during mitral valve repair.
Following transcatheter mitral valve repair (t-MVR), up to 25 percent of patients with initial satisfactory results will develop recurrent regurgitation, suggesting the inadequacy of standard intraoperative transthoracic ultrasound assessment to anticipate mid- and long-term failure. This shortcoming sparked a strong interest among Mount Sinai cardiothoracic
surgeons and interventional cardiologists for an intraoperative assessment tool to effectively guide the t-MVR procedure.
With the help of Mount Sinai BioDesign, Daniel Grinberg, MD, MS, and David H. Adams, MD, developed the MitralPrint guidewire to quantify MCF in real-time during both open heart surgery for mitral valve repair and minimally invasive t-MVR.
MitralPrint heads to commercial development and production
The device is placed within the beating heart to measure the MCF between the two mitral leaflets, serving as a key indicator of surgical efficiency aimed at reducing repair failures and thus the need for secondary valve repair. A start-up company has been launched to support commercial development and production of the device.
Dr. Adams is the Marie-Josée and Henry R. Kravis Professor and Chair of Cardiovascular Surgery, and Cardiac Surgeon-in-Chief for the Mount Sinai Health System. Dr. Grinberg, a former cardiothoracic fellow under Dr. Adams, is currently at the Université Lyon in France.
PharyVac, an intra-pharynx aspiration catheter to ease blood aspiration and reduce viral particle aerosolization.
The aspirator was designed early in the COVID-19 pandemic to prevent aerosolization of the SARS-CoV-2 virus during surgeries in the nasal sinuses and base of the skull. It is the first suction device to obviate the need for throat packs and a separate suction cannula during nasal and upper airway surgery.

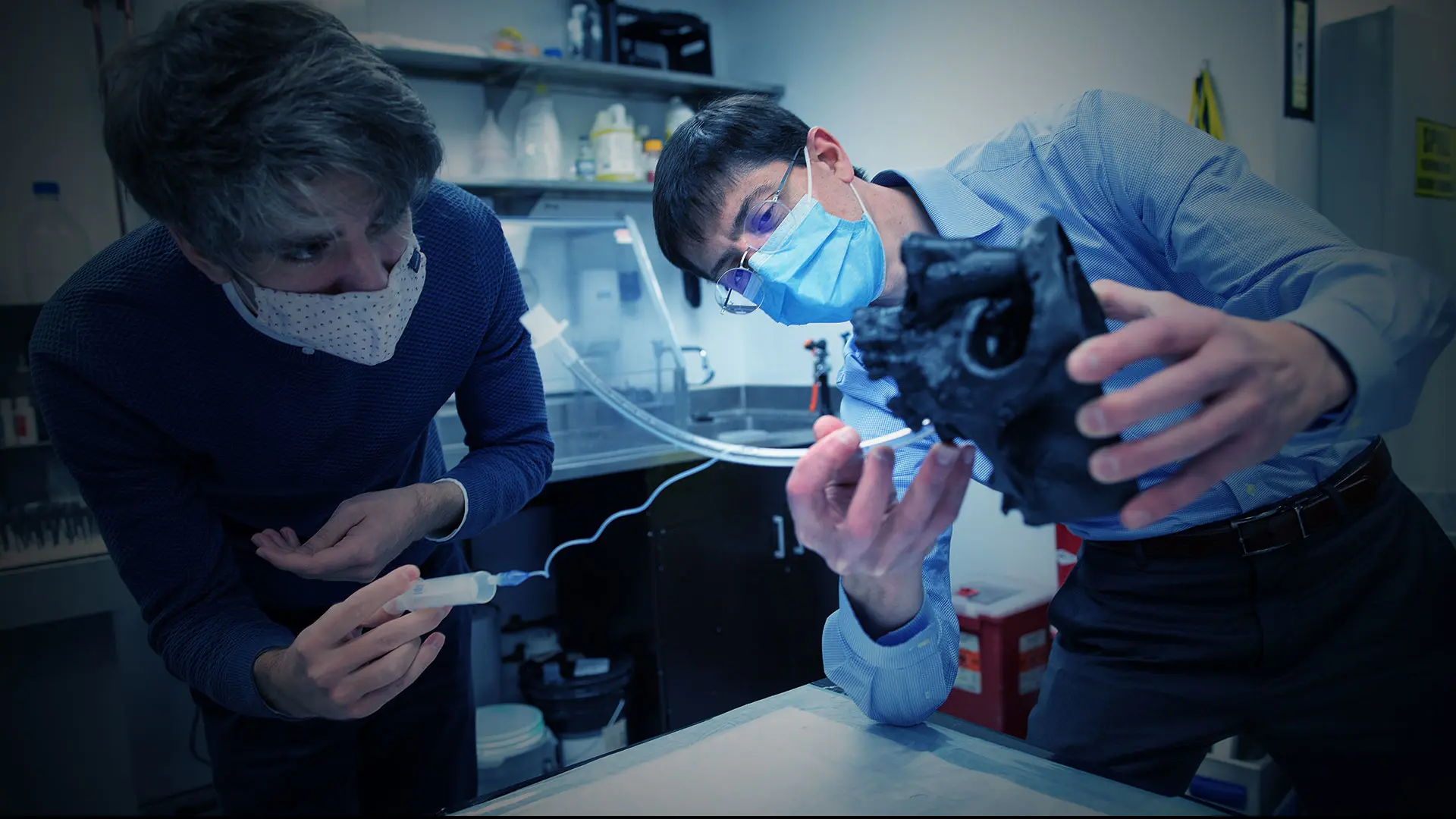
Benjamin I. Rapoport, MD, PhD, Scientific Director of Mount Sinai BioDesign, right, with Alexis Bruhat, MEng, Associate Director, test the pharynx aspirator prototype in an endonasal skullbase phantom model.
It is designed to:
• save surgeons time (there is no need to wait for suction of smoke, dust, or blood),
• increase safety (by reducing visual interference during surgery), and
• improve patient outcomes (by reducing risk of aspiration and accumulation of blood in the stomach).
The device was designed in collaboration with Alfred M.C. Iloreta Jr., MD, Assistant Professor of Otolaryngology, and Neurosurgery, at Icahn Mount Sinai. The first human clinical trial of this device is being set up by Mount Sinai BioDesign, which is in discussion with a major medical device company regarding a partnership arrangement that would lead to its commercialization.