Also:
Patients with a history of depression, smoking, and alcoholism were more likely to be readmitted, while advanced age and discharge home were protective.
There was no observed significant difference in SA readmissions between groups.
The research was led by Mount Sinai researcher Laura K. Stein, MD, MPH, under the senior mentorship of Mandip S. Dhamoon, MD, DrPH, and published August 27, 2020, in Cerebrovascular Diseases Extra.
The study was launched to address the lack of nationally representative data comparing rates of depression and SA among patients who have experienced these ischemic vascular events.
Accessing the 2013 Nationwide Readmissions Database, which contains more than 14 million admissions for all payers and the uninsured, the team used International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) Codes, to identify index admission with IS (n = 434,495) or MI (n = 539,550) and readmission for depression or SA. The team calculated weighted frequencies of readmission for depression and SA
following IS and MI and performed adjusted Cox regression to calculate the hazard ratio (HR) for readmission for depression and SA 1 year following IS versus MI. Analyses were stratified by discharge home versus elsewhere.
Dr. Stein, Assistant Professor of Neurology at the Icahn School of Medicine at Mount Sinai, noted that depression readmission rates were higher at 30, 60, and 90 days among patients who had experienced IS versus those who experienced MI (0.04 percent, 0.09 percent, and 0.12 percent vs. 0.03 percent, 0.05 percent, and 0.07 percent, respectively).
“...these findings emphasize the importance of screening patients for depression following a stroke or MI so that we can intervene and, hopefully, impact quality of life and outcomes.”
- Laura K. Stein, MD, MPH
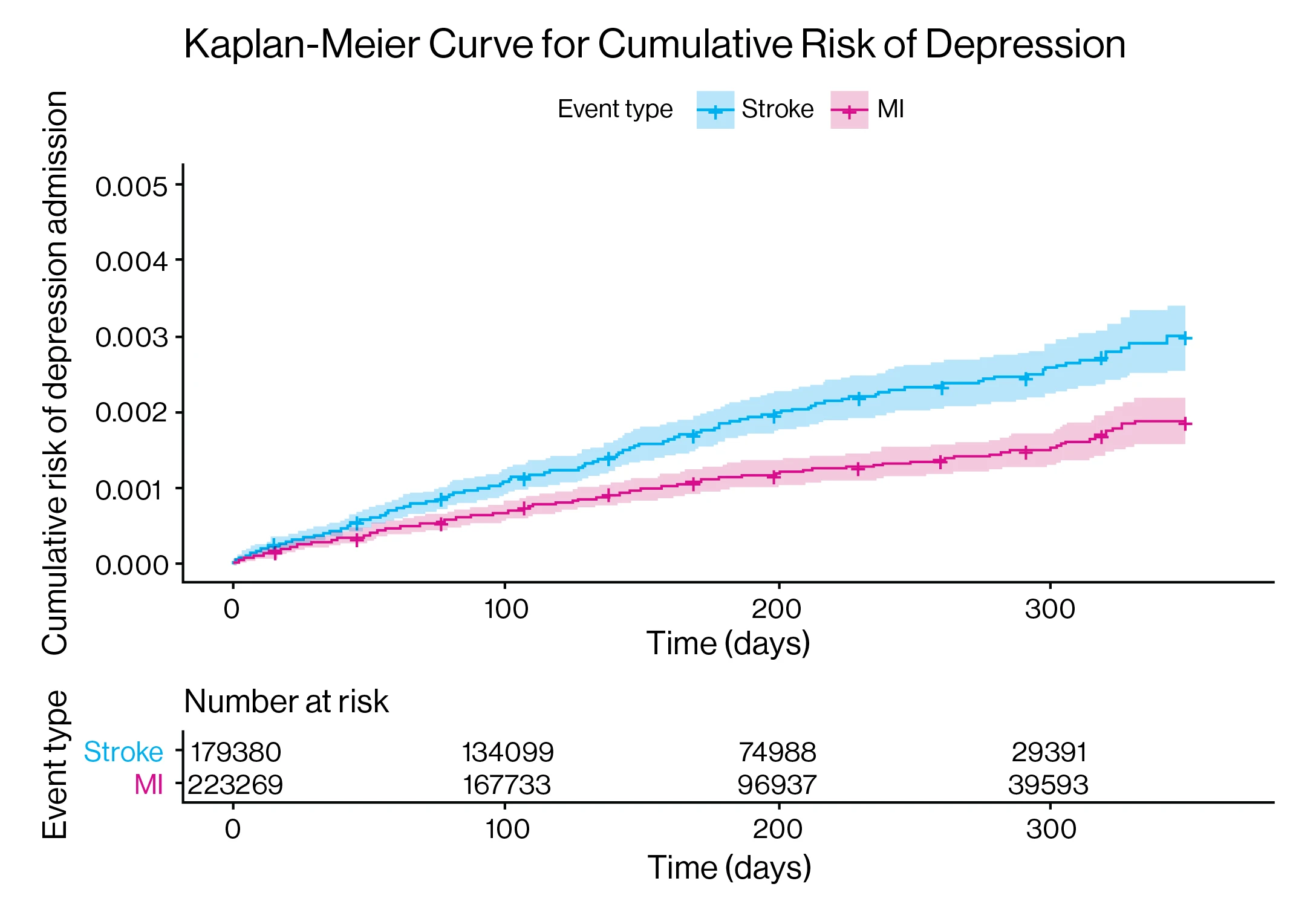
Kaplan-Meier cumulative risk of depression.
Above: Kaplan-Meier cumulative risk of depression. Kaplan-Meier curves of cumulative risk of the outcome of depression readmission following index admission for stroke and myocardial infarction (MI) are shown. The x axis depicts the time in days and corresponding number of index stroke and MI patients at risk and the y axis the cumulative risk of readmission for depression. log-rank p< 0.0001.
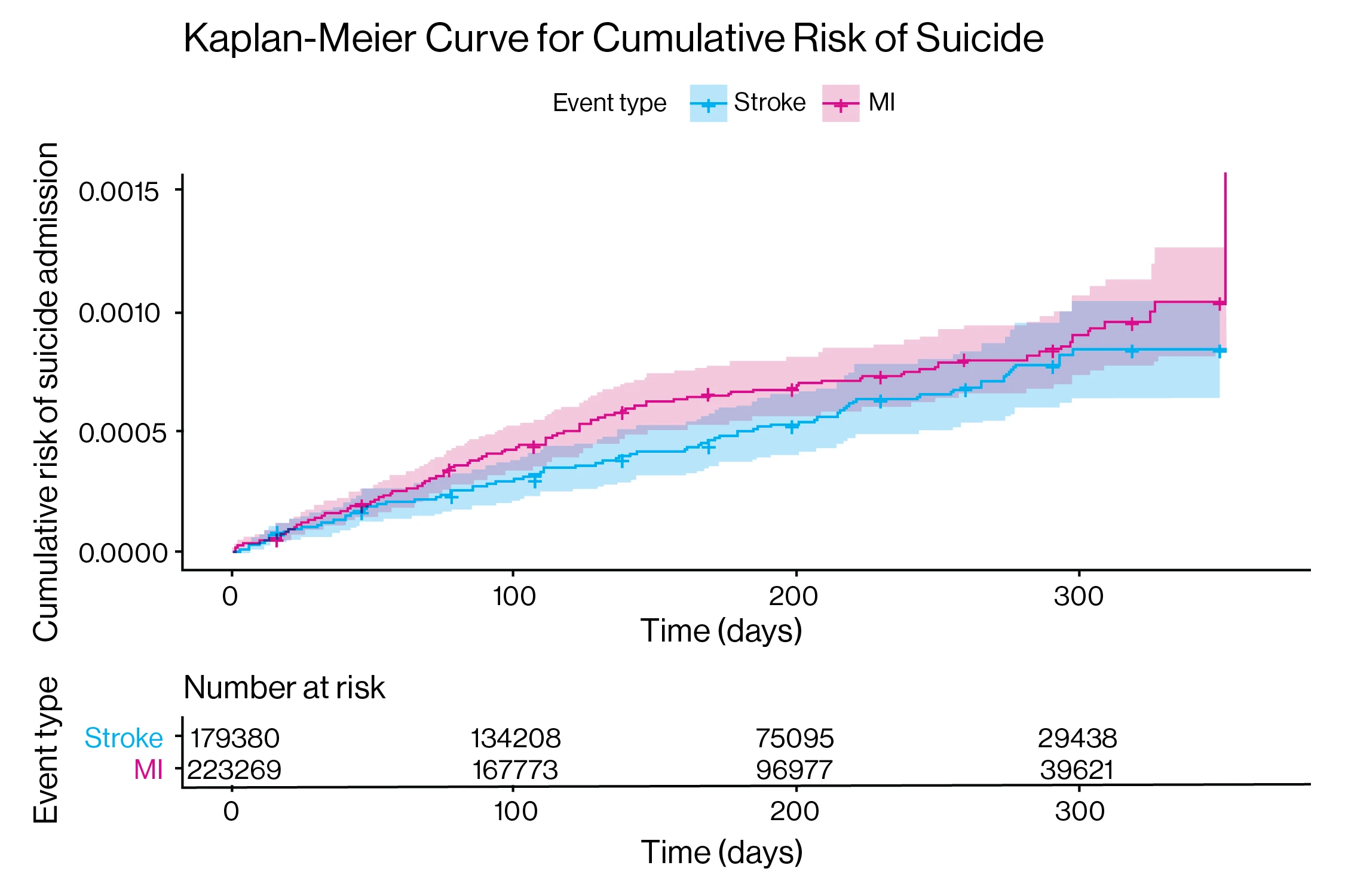
Kaplan-Meier cumulative risk of suicide attempt (SA).
Above: Kaplan-Meier cumulative risk of suicide attempt (SA). Kaplan-Meier curves of cumulative risk of the outcome of SA following index admission for stroke and MI are shown. The x axis depicts the time in days and corresponding number of index stroke and MI patients at risk and the y axis the cumulative risk of readmission for SA. log-rank p = 0.13.
“We know that 20 percent to 30 percent of patients who experience a stroke or MI subsequently experience depression, and that depression is three times more common in these populations than the general population,” Dr. Stein says. “Given that depression is underdiagnosed and treated in general, these findings emphasize the importance of screening patients for depression following a stroke or MI so that we can intervene and, hopefully, impact quality of life and outcomes.”
Dr. Stein also observed that advanced age (i.e., patients older than 70) (0.46 [0.37–0.56]) and discharge home (0.69 [0.57–0.83]) were associated with reduced hazards of readmission, saying, “One hypothesis is that the impact of a stroke on quality of life among that demographic is less pronounced than that among younger patients who might be more active in society.”
Overall, she says, “There is much more work to be done. It is unclear to what extent differences in type of ischemic tissue damage and disability contribute, and further investigation is warranted.”
Featured
Mandip S. Dhamoon, MD, DrPH
Associate Professor of Neurology, Icahn School of Medicine at Mount Sinai

Laura K. Stein, MD, MPH
Assistant Professor of Neurology, Icahn School of Medicine at Mount Sinai