“There was a real need for a home-monitoring program for patients who had been infected with the virus,” says Dr. Kellner, Assistant Professor of Neurosurgery at the Icahn School of Medicine at Mount Sinai. “It was Dr. Putrino who immediately realized that our initiative could be used for that purpose, so we sat down to see how that would work.” Dr. Putrino is an Assistant Professor in the Department of Rehabilitation and Human Performance.
Precision Recovery takes a hands-on approach to monitoring patients who have experienced an ischemic or hemorrhagic stroke during their post-discharge recovery. These patients are at high risk for a second stroke if risk factors are not tightly controlled. They also benefit from seeing the neurologic and functional progress they are making and gain access to advanced physical therapy programs and technology.
Once enrolled in the program, patients use a customized app to report their blood pressure and answer a few questions about symptoms each day, then record themselves doing an abbreviated neurologic exam once a week. Every four weeks, patients review the data with their personal Precision Recovery provider, receive education about stroke and therapy options, and have an opportunity to ask questions.
800+
number of COVID-19 patients monitored remotely over 10 months
For the COVID-19 module, participants diagnosed with COVID-19 or symptoms suspicious
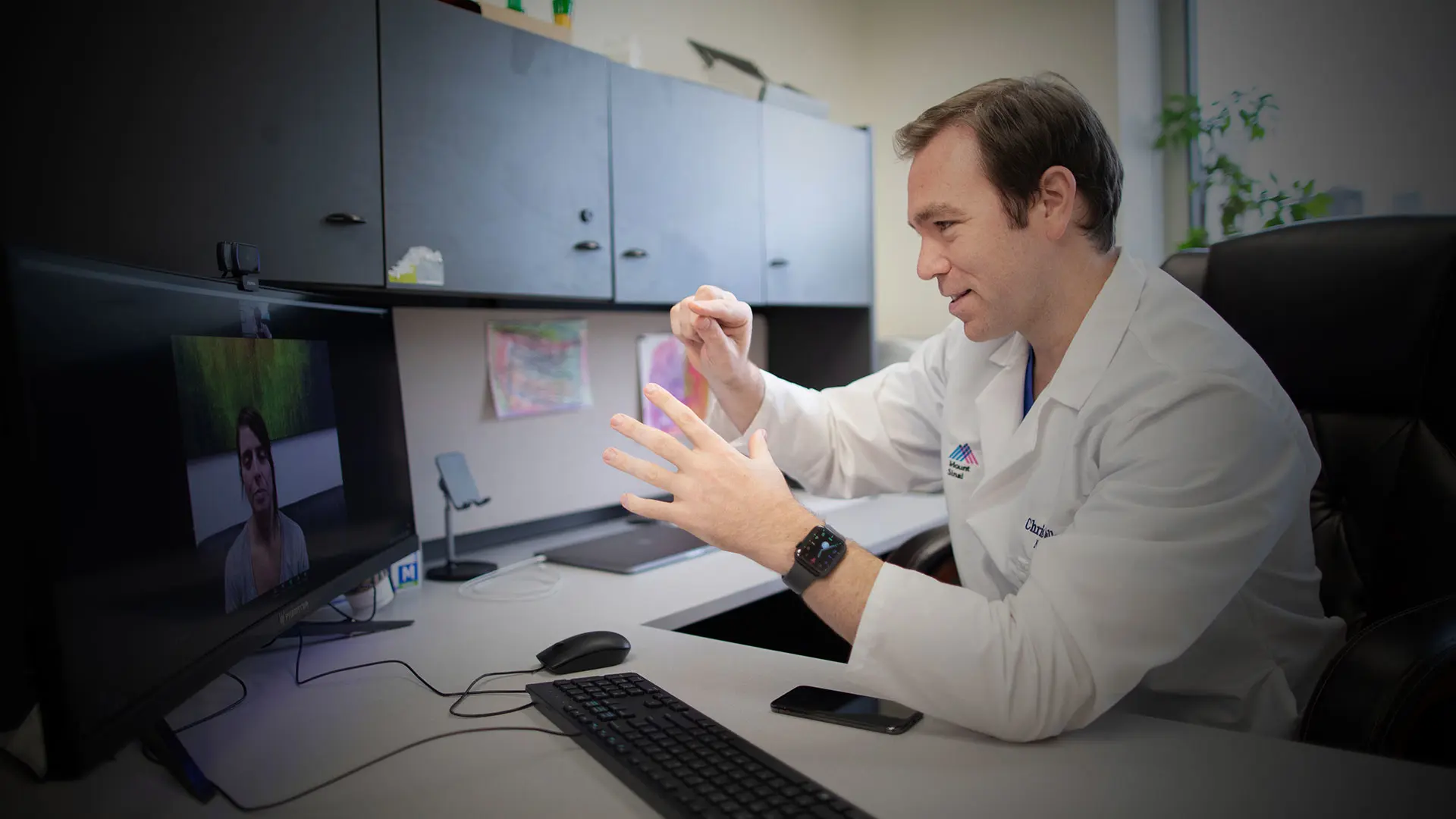
for COVID-19 download the same app but receive a monitoring plan specific to COVID-19. A care provider is assigned to each patient and remains with them throughout the course of the illness. Through the app, patients complete daily surveys regarding the symptoms they are experiencing and report thermometer and pulse oximeter data when possible. Their assigned care provider reviews their data daily and has brief weekly video calls to check in for a one-on-one conversation about the patient’s symptoms and physiologic data. When patients report severe or worsening symptoms, their Precision Recovery provider contacts the patient via video chat to assess if the patient needs an escalation in the care they are receiving. The provider also has the capability to add a physician to the video chat, make recommendations for medication changes, or triage the patient to the emergency room. This continuity-of-care model allows an interdisciplinary approach to care as patient care can be escalated to a specialist if required, while always maintaining contact with their designated provider.
“By monitoring the trajectory of their symptoms, assigned care providers are able to catch patients at the point their condition begins to worsen and advise them on whether they should go to the hospital,” Dr. Kellner says. “We are also able to address patient questions and anxiety about the disease and related symptoms. That educational component is important. The feedback we have received is that this psychosocial supportive aspect is really beneficial in helping patients understand the course of this new and potentially dangerous disease.”
A perioperative protocol was launched in 2021 for spine surgery.
The program has also provided Dr. Kellner and his Mount Sinai colleagues with invaluable insights on how patients are affected by COVID-19, not just fluctuations in symptoms that
occur over the course of the disease but also the types of prolonged symptoms that patients experience. “Our group was one of the first to observe this chronic COVID-19 phenomenon, and that observation led to media coverage and greater awareness that this was occurring among patients,” Dr. Kellner says. “As Precision Recovery is a continuous monitoring program, enrolled patients who were not improving were quickly identified.” During a 10-month period, the program has monitored more than 800 patients.
The COVID-19 module of Precision Recovery was the proof of concept that patients
like remote monitoring, says Dr. Kellner. And, the team is considering the program for other areas. “We have developed a perioperative protocol, and we have already started rolling it out for spine surgery in the Neurosurgery department,” he says. “Through our experience triaging COVID-19 patients during the height of the pandemic, we learned a lot about what is needed to set up this program for specific patients, and I think the future holds considerable potential for broadening the application of this type of care."
In November 2020, Precision Recovery went back to its roots in the Neurosurgery department and launched the Spine Surgery module with spine neurosurgeons Tanvir F. Choudhri, MD, Associate Professor of Neurosurgery, and Co-Director of the Neurosurgery
Spine Program; and Jeremy M. Steinberger, MD, Assistant Professor of Neurosurgery,
Orthopedics, and Rehabilitation Medicine, and Director of Minimally Invasive Spine Surgery at the Mount Sinai Health System.
“Prior to spine surgery, we begin monitoring patient information like pain, posture, and mobility to see how we can 'pre-habilitate' a patient prior to surgery,” says Dr. Choudhri. “The data generated by this platform—while the patient remains safely at home—provide the surgeon and physiatrist with a granular recovery profile created to give the patient the best possible outcomes.”
To learn more about the Precision Recovery Program for COVID-19, go to https://www.liebertpub.com/doi/full/10.1089/tmj.2020.0339.
Featured

Christopher P. Kellner, MD
Director of Mount Sinai's Intracerebral Hemorrhage Program and Assistant Professor of Neurosurgery

David Putrino, PhD
Director of Rehabilitation Innovation, and Assistant Professor, Department of Rehabilitation and Human Performance