Over the course of the pandemic, Mount Sinai’s Neurosurgery Department, led by Joshua B. Bederson, MD, continued to see patients and expertly manage their care. “We have performed virtual consults for patients in New York State, as well as across the country and
internationally,” says Dr. Bederson.
One such patient, Katelyn, had found Dr. Bederson through social media and subsequently was consulted by a multidisciplinary team and underwent surgery in June 2020.
A 20-year-old student at a New York City suburban college with a known history of migraines, Katelyn experienced a witnessed seizure that lasted approximately three minutes with tonic clonic movements on Sunday, March 1, 2020, while in school. The patient reports that she was in the dining area of her college when she started seeing flashes of lights and color, which she describes as a visual aura. Not feeling well, she went to the bathroom and proceeded to lower herself to the ground when she lost consciousness. Her friends witnessed her face “turning blue,” as well as convulsions. She woke up surrounded by paramedics and police officers, having no recollection of losing consciousness and no memory of what occurred during her presumed seizure.
She was taken to a local hospital and underwent a CT of the head that revealed a hemorrhage component within the left occipital cavernous malformation. The following day she underwent an MRI of the brain w/wo contrast that confirmed the presence of a 14 mm lesion within the occipital lobe most consistent with a cavernous malformation aka
cavernoma. The patient was placed on Topiramate 100 mg BID for seizure management by her local neurologist.
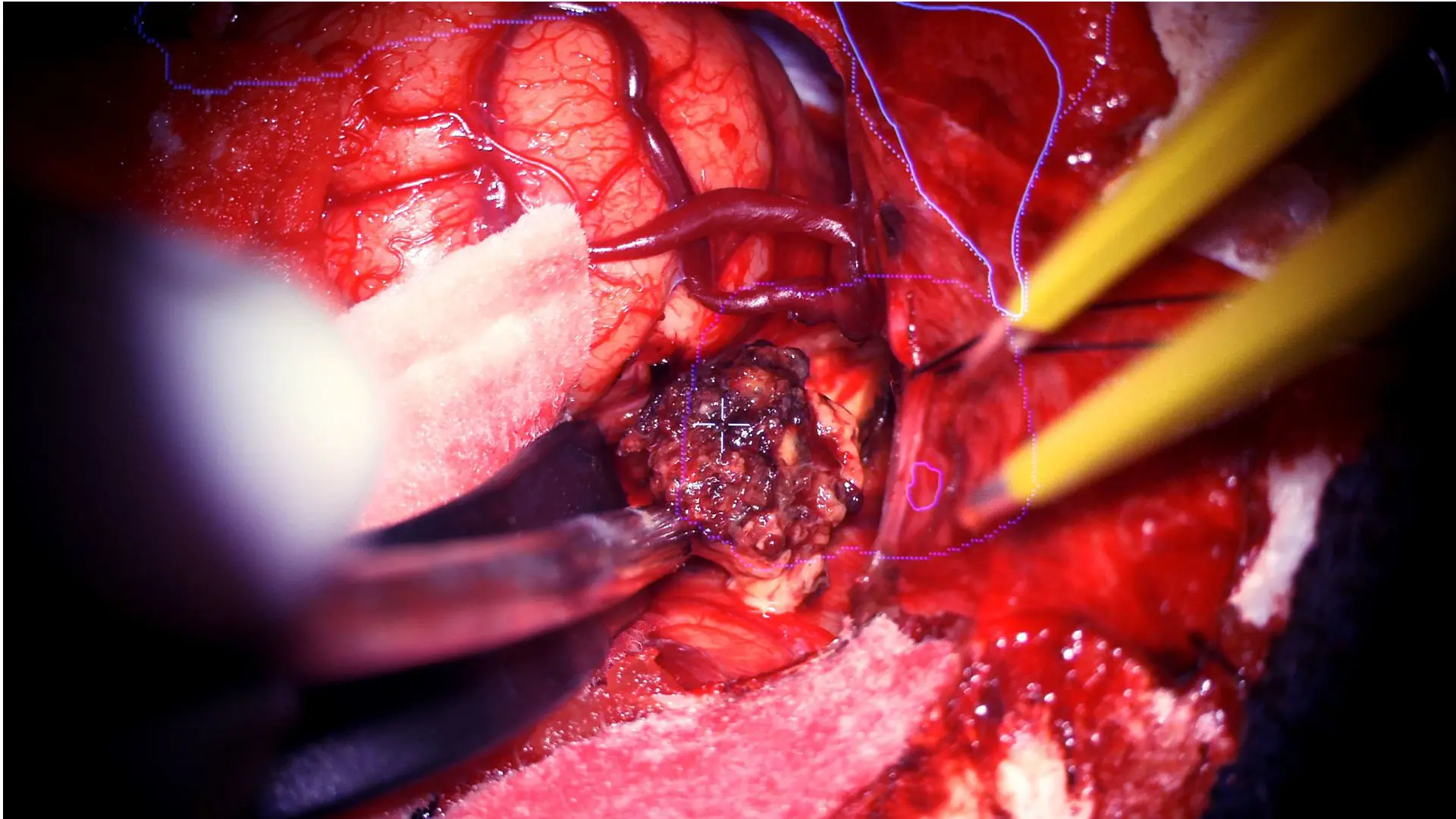
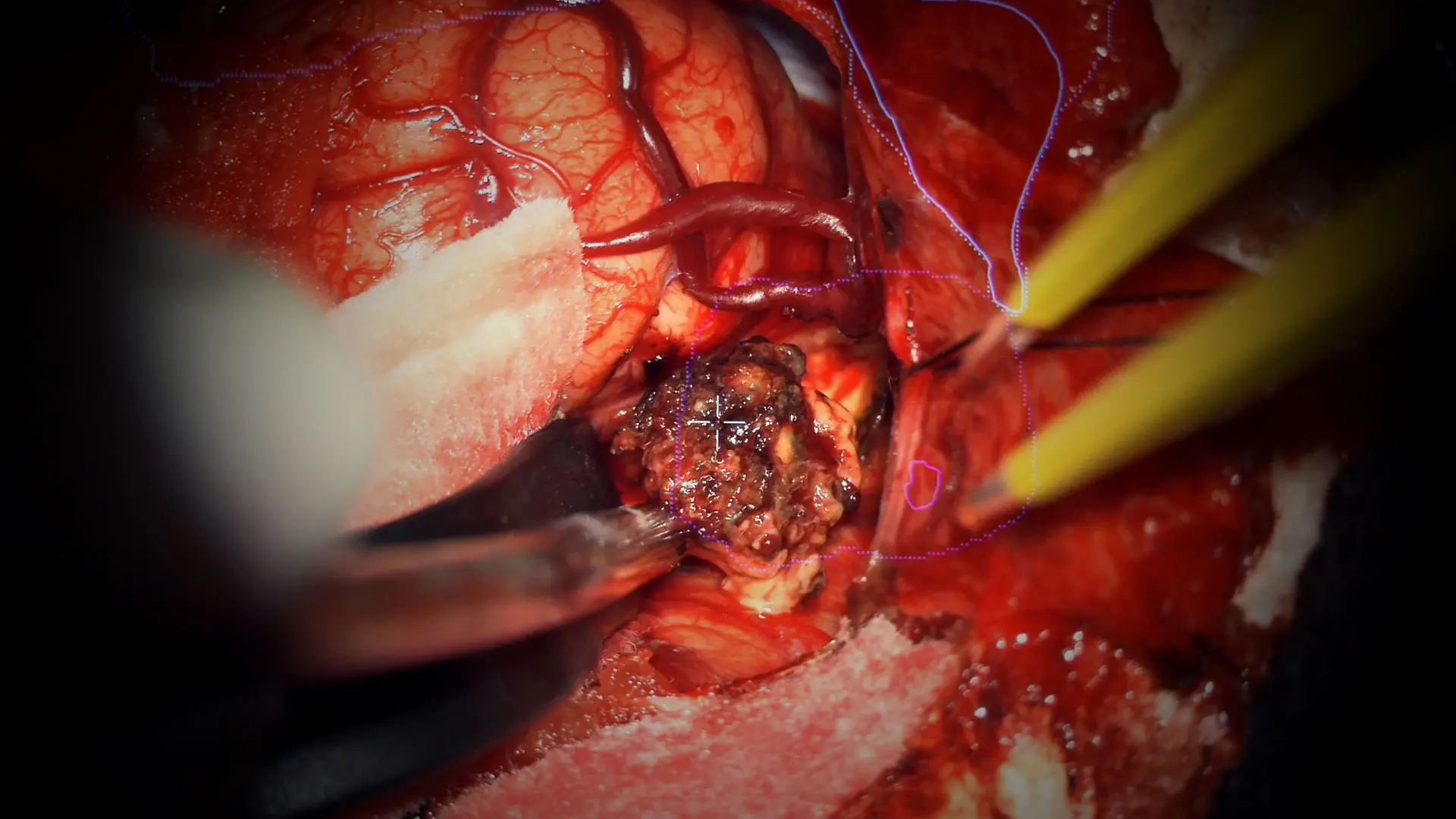
The borders of the cavernous malformation are identified, and the lesion is removed.
Katelyn continued to be bothered by migraine headaches with associated nausea and vomiting, as well as frequent visual auras since her seizure event. The symptoms had worsened after the seizure event, and she was experiencing severe anxiety. She had her first appointment with Dr. Bederson and Leslie Schlachter, PA-C, by telehealth on Monday, May 18, 2020, to discuss treatment plans and schedule surgery. Later that week, during a virtual appointment with Ms. Schlachter, Katelyn was able to see the 3D simulation created by the neurosurgery team that displayed Katelyn’s brain anatomy with the cavernoma—typically conducted during an in-person consultation—reassuring Katelyn and raising her confidence.
During a virtual appointment with the patient, the neurosurgery team shared the 3D simulation they had created that displayed the brain anatomy and the cavernoma, greatly reassuring the patient and raising her confidence.
All of Katelyn’s complex treatment plans included coordination of care from neurologist Madeline Fields, MD, including an EEG, and an onsite exam from neuro-ophthalmologist Mark Kupersmith, MD.
The Mount Sinai Neurosurgery Department enforced strict safety precautions for patients who required onsite care, identifying eligible candidates in general good health in need of immediate surgery able to be cared for in an isolated intensive care unit setting. In May 2020, Katelyn followed protocol to receive a SARS-CoV-2 polymerase chain reaction (PCR) test prior to her arrival in the hospital. On Tuesday, June 2, 2020, she arrived at The Mount
Sinai Hospital and met Dr. Bederson in person for the first time.
Dr. Bederson performed a suboccipital craniotomy for resection of the 1.6 cm cavernous malformation using highly advanced navigation, and alternate reality and heads-up display simulations for visualization intraoperatively. The Department of Neurosurgery collaborates
with industry partners and also develops these novel technologies in-house that
enhance a surgeon’s ability to perform surgeries, including providing detailed, real-time information about critical structures.

During the two-week postoperative visit, Joshua B. Bederson, MD, and Leslie Schlachter, PA-C, inspect Katelyn’s incision to ensure it is healing properly.
Postoperatively, Katelyn experienced no complications, and 48 hours after surgery she returned to quarantined life. An MRI and an in-person, follow-up exam three months later revealed a healthy brain and no recurrence of her cavernoma. She will remain on antiepileptics for at least one year postop. Her appointments continue virtually.
While the use of telemedicine seldom occurred prior to the start of the pandemic, Dr. Bederson and Ms. Schlachter quickly adapted to seeing patients solely in this format, successfully evaluating them pre- and postoperatively without sacrificing the quality of their care or surgeries. Collectively, the team has had 731 telemedicine appointments between March 17, 2020, and December 31, 2020.
Joshua B. Bederson, MD, Professor and Chair of Neurosurgery for the Mount Sinai Health System, owns equity in, and receives financial compensation as a lecturer for, Surgical Theater, LLC.
Featured

Joshua B. Bederson, MD
Leonard I. Malis, MD / Corinne and Joseph Graber Professor of Neurosurgery and Chair, Department of Neurosurgery at the Mount Sinai Health System

Leslie Schlachter, PA-C
Clinical Director and Chief Physician Assistant for the Department of Neurosurgery

Madeline Fields, MD
Associate Professor of Neurology, and Co-Director of Mount Sinai’s Epilepsy program

Mark Kupersmith, MD
Professor of Neurology, Neurosurgery, and Ophthalmology, and Director of Neuro-Ophthalmology