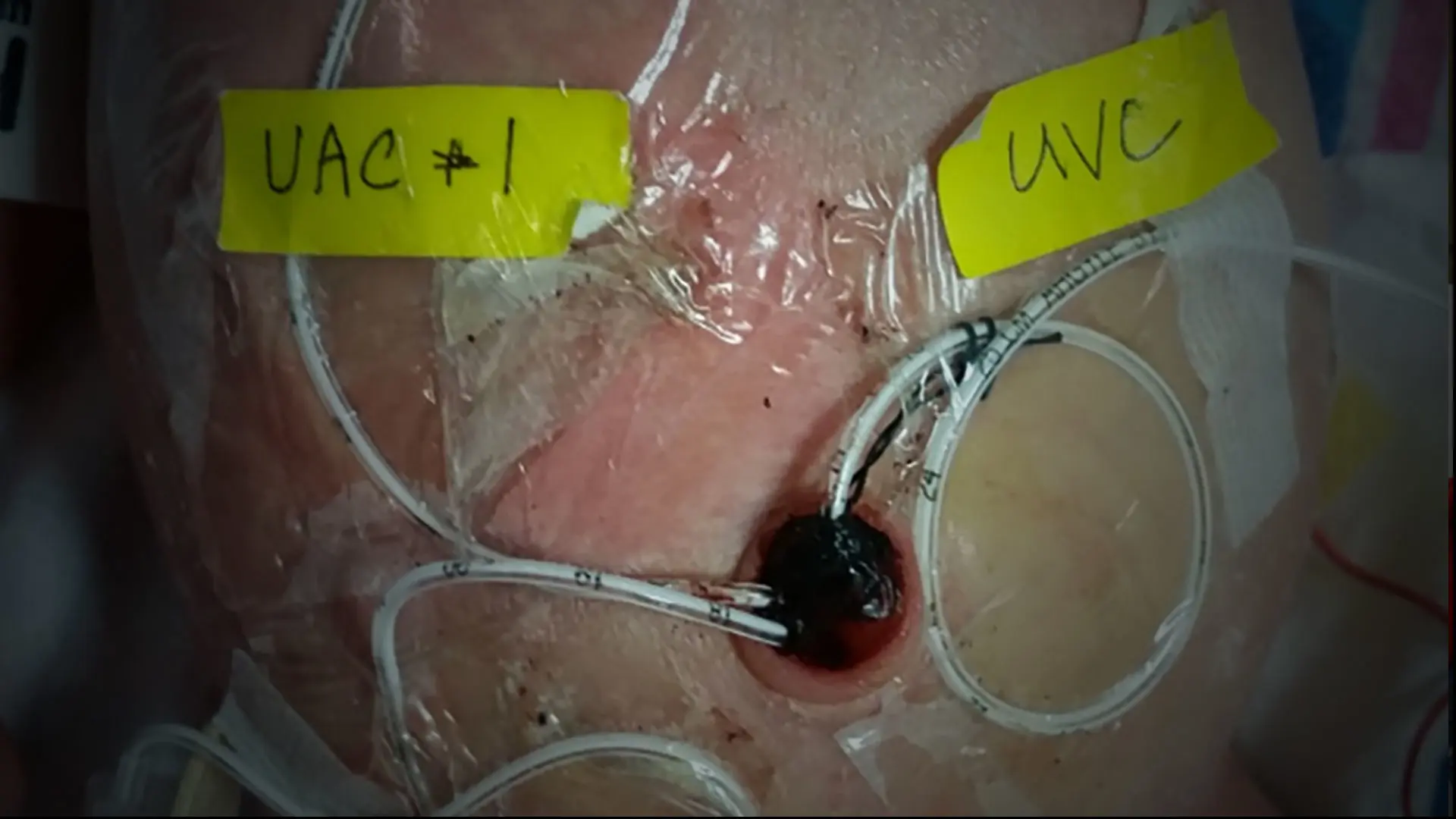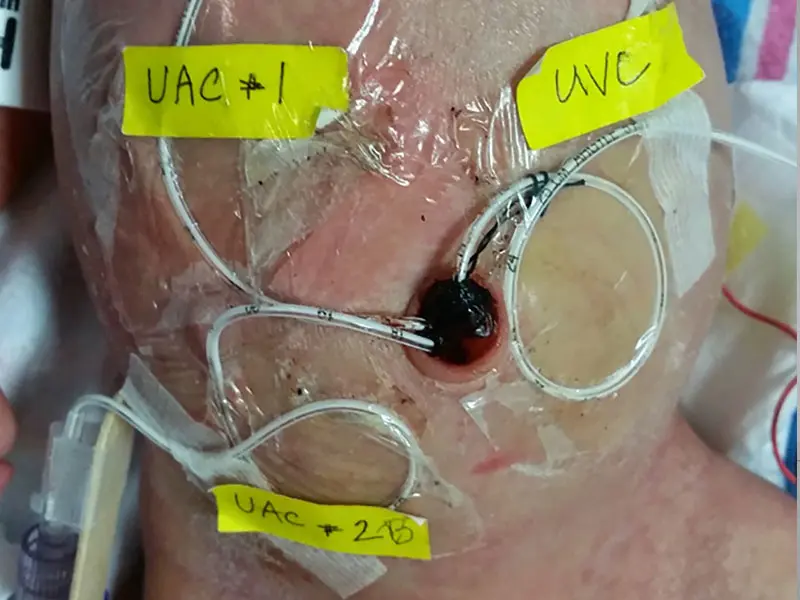
While Baby H was in the NICU, he had arterial lines placed in both umbilical arteries, and one in the umbilical vein, in anticipation of needing endovascular access, a technique that Mount Sinai Health System interventional neuroradiologist Alejandro Berenstein, MD, had pioneered.
Baby H was only 2 days old in June 2013 when pediatricians in the neonatal intensive care unit (NICU) in Sioux Falls, South Dakota, noticed signs of severe congestive heart failure. After an unremarkable prenatal course and routine Cesarean section delivery, he was found to have pulmonary hypertension and an enlarged heart. Although he was neurologically normal, a head ultrasound was obtained, which was suggestive of a vein of Galen malformation (VOGM).
VOGM is congenital, and can be seen in utero at around 27 weeks gestation. They are one of the most severe expressions of all vascular malformations, and given their central location, are not amenable for conventional neurosurgical repair in newborns in severe heart failure. If untreated, patients almost universally die in the neonatal period or in early infancy.
At 4 days old, due to severe, progressive heart failure, Baby H was urgently transferred to Mount Sinai by air ambulance. While Baby H was in the NICU, he had arterial lines placed in both umbilical arteries, and one in the umbilical vein, in anticipation of needing endovascular access, a technique that Mount Sinai Health System interventional neuroradiologist Dr. Berenstein had pioneered. Requiring microcatheterization of small arterial branches, endovascular treatment with embolization has now become the treatment of choice. This technique is best accomplished with liquid tissue adhesives in an effort to decrease the overall blood flow to the VOGM. Baby H received treatment shortly after transfer.
A world expert in the complex endovascular treatment of VOGM, Dr. Berenstein has successfully treated this highly lethal condition in more than 300 pediatric patients. Dr. Berenstein’s strategy is to intervene as soon as possible in these newborns, and, as in the case of Baby H, reverse the neonatal heart failure.
Dr. Berenstein was able to use a micro-guidewire to exchange the umbilical arterial catheter for a larger bore introducer sheath.
First transumbilical embolization
Above, first transumbilical embolization: Based on the preoperative MRI, which demonstrated the largest fistula to the vein of Galen arising from the right posterior cerebral artery, Dr. Berenstein planned a course for fistula embolization using the left vertebral artery for access. Frontal and lateral angiograms of the left vertebral artery show high flow fistulas into the vein of Galen malformation. Angiograms of the microcatheter in the right posterior cerebral artery demonstrate one of the fistulas in frontal and lateral projections. The video shows the injection of cyanoacrylate in frontal, and then, in lateral projections as it closes the fistula. Angiograms of the second fistula and video of second glue injection show the closuring of a second fistula. Third fistula, with glue injection, shows the previous glue helping to prevent distal migration of the additional glue. Frontal and lateral angiograms of the left vertebral artery at the end of the first transumbilical embolization that permitted control of congestive failure. Dr. Berenstein then injected a small amount of 80 percent to 90 percent n-BCA glue into the branch, penetrating into the vein to close the fistula itself. This glue acts like superglue in the vessels, adhering to the endothelium of the artery and vein. (Dr. Berenstein now uses newer microcatheters with a detachable tip.) This was repeated several times in several different fistule until the overall flow to the fistula was decreased.
Given the progressive and extensive nature of VOGMs, children often require multiple endovascular treatment sessions. Dr. Berenstein typically follows these children into adulthood and makes every attempt to cure these malformations with various endovascular strategies, many of which he has pioneered.
With the support of cerebrovascular and interventional neurologist, Johanna T. Fifi, MD, and cerebrovascular neurosurgeon, Tomoyoshi Shigematsu, MD, PhD, Baby H ultimately required 16 procedures over the course of six and a half years to reduce the fistula flow and ultimately cure the malformation, with the final procedure in 2020 utilizing an innovative transvenous embolization.
Embolization 6.5 years later
Above, embolization 6.5 years later: Here, the frontal and lateral digital subtraction angiography (DSA) of the left vertebral artery prior to the last embolization demonstrate marked reduction in the flow with a small residual malformation supplied by thalamoperforating arteries. This prompted Dr. Berenstein and the team to address the residual malformation through a transvenous approach. Video demonstrates the transjugular approach, as Dr. Berenstein and team placed a triaxial system in the straight sinus to embolize the malformation. Final control angiogram of the left vertebral artery (LVA) shows the complete occlusion of the malformation.
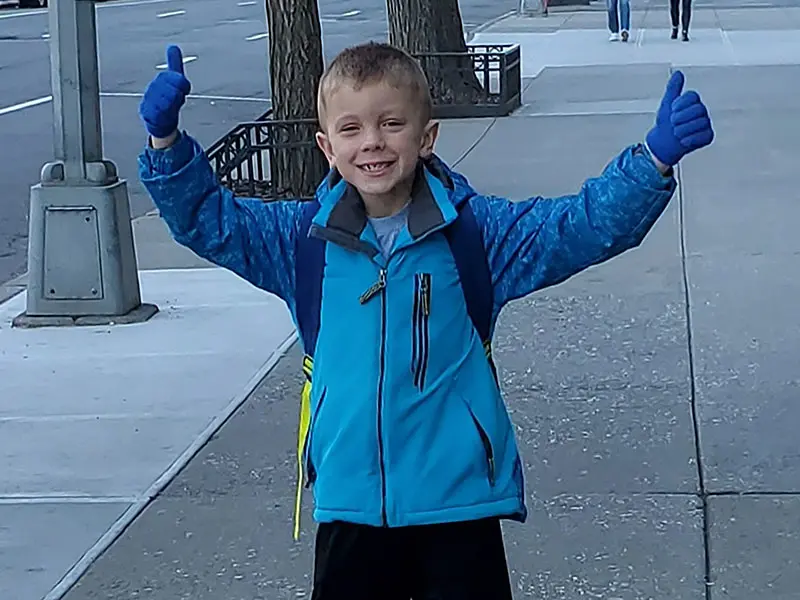
At 6.5 years old, the patient completes a normal neurological exam and is successfully cured from his vein of Galen malformation.
Now, at 7 years old, the patient is cured and living life as a normal child with his parents and siblings in South Dakota.
Featured

Alejandro Berenstein, MD
Professor, Neurosurgery, Radiology, and Pediatrics; and Director, Pediatric Cerebrovascular Program, Mount Sinai Health System

Johanna T. Fifi, MD
Associate Professor, Neurosurgery, Neurology, and Radiology; Associate Director, Cerebrovascular Center; and Director, Endovascular Stroke Program

Tomoyoshi Shigematsu, MD, PhD
Assistant Professor, Neurosurgery; and Diagnostic, Molecular and Interventional Radiology