Each week, 220 patients visit the Mount Sinai Kidney Center in East Harlem for maintenance hemodialysis therapy—a challenging regimen to maintain under optimal conditions, but even more so during the COVID-19 pandemic. Each visit increases the patients’ risk of infection, and comorbidity increases their risk of mortality.
“Although there are patients who contracted COVID-19 and subsequently developed kidney failure requiring dialysis or additional care, our patients are people whose kidneys failed prior to COVID-19 and who require dialysis three times a week,” says Vijay Lapsia, MD, Associate Professor of Medicine (Nephrology) at the Icahn School of Medicine at Mount Sinai. “Many of them tend to be older, underserved, have low literacy levels, or are at high risk for infection based on pre-existing conditions including race, so we were concerned about health outcomes among this population. We knew we could not account for every possible exposure to COVID-19, such as transportation or subsidized housing, but we could make dialysis as safe as possible for our patients by implementing a comprehensive plan with prevention, screening, testing, and treatment measures.”
The Center began implementing prevention measures in March 2020. Access was limited to patients who were undergoing treatment; all others, such as family members and supporters, were required to wait outside. A mandatory mask policy was introduced, and surgical masks were provided to all patients entering the facility. Although dialysis stations were already situated at least six feet apart, there were concerns that waiting room congestion could result in infections. Dr. Lapsia says the Center addressed this by switching from shift scheduling to block scheduling.
“Previously, we started treatment shifts at 6 am, 10 am, 2 pm, and 6 pm, which meant we had patients gathering in our waiting room,” says Dr. Lapsia, who also is Medical Director for the Center. “By establishing 10-minute scheduling blocks and assigning a time to each patient, we were able to clear out the waiting room and maintain social distancing among patients.”
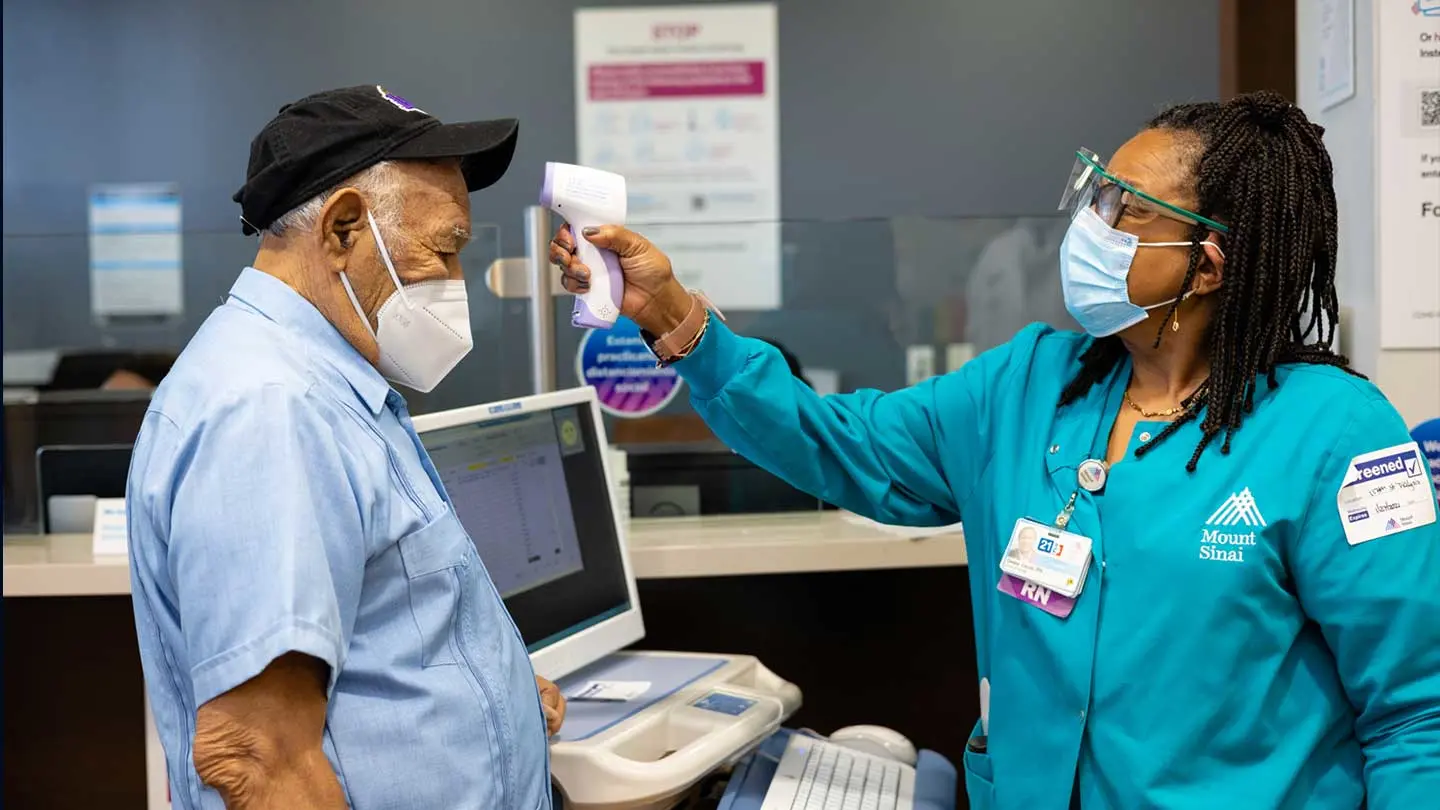
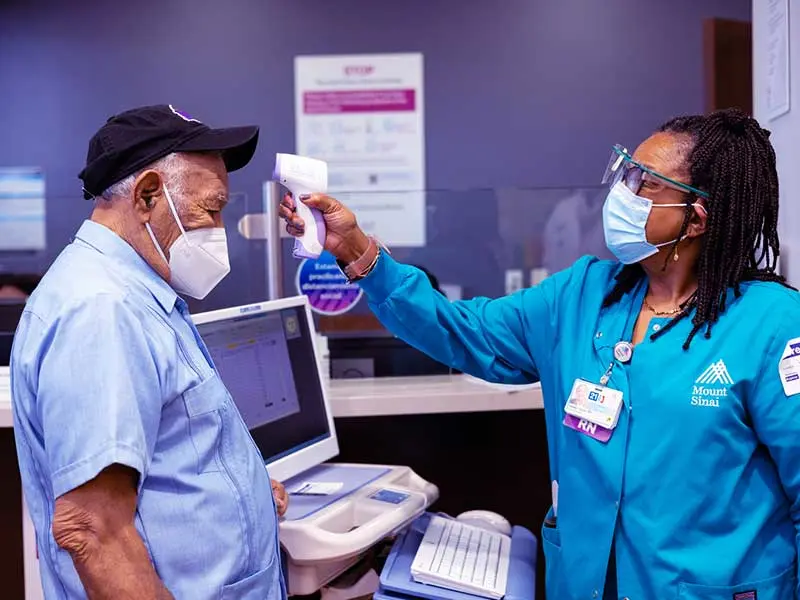
To further reduce risk of infection, daily screening measures—questionnaires and temperature checks—were introduced and patients experiencing COVID-19-associated symptoms were required to call before their scheduled dialysis treatment. Those who had symptoms or elevated temperatures underwent oral referential swab testing at the Center and, depending on the severity of their symptoms, some received dialysis treatment in an isolation room before being referred to The Mount Sinai Hospital’s Emergency Department for further consultation.
“I am not aware of any other dialysis center in New York City that performed testing,” Dr. Lapsia says. “That was groundbreaking, because it enabled us to arrange for direct consultations, meaning no wait for our patients, and we could conduct dialysis treatments safely before patients left the Center, thus reducing their risk of experiencing adverse events due to a gap in treatment.”
220
Weekly hemodialysis patients served by the Mount Sinai Kidney Center
3.6%
mortality rate among them due to COVID-19
Patients who tested positive for COVID-19 but did not require an emergency room referral or hospitalization received dialysis during a dedicated COVID-19 shift at the end of the day. This enabled staff to meet all cleaning and disinfection protocols prior to the next day’s shift. Staff who called out sick due to COVID-19 were assigned to this shift upon returning to work—a further safeguard for patients and other staff who had not been exposed to the disease or were not experiencing symptoms.
Although Dr. Lapsia cannot say with certainty that these measures had a direct impact on outcomes, he notes that only eight of the 12 deaths among the Center’s 220 patients between March and July 2020 were documented as COVID-19-positive—a mortality rate of 3.6 percent. In contrast, early reports from Italy, Spain, and the United Kingdom estimated the mortality rate among maintenance hemodialysis patients at approximately 30 percent. Meanwhile, anecdotal reports collected by Dr. Lapsia suggest mortality rates in New York City have ranged from 15 percent to 18 percent in the Bronx to 28 percent in Brooklyn during this same period.
“I think it helped that most of our patients were referred to Mount Sinai because it is a tertiary center, so it is well prepared to manage a crisis like COVID-19,” Dr. Lapsia says. “But I also believe our outcomes demonstrate the importance of being proactive in addressing a pandemic such as this. The plan now is to keep those measures in place until the pandemic is over, and then continue block scheduling in addition to implementing the mask policy during flu season for the benefit of our patients.”


Featured

Vijay Lapsia, MBBS
Associate Professor of Medicine (Nephrology)