Under normal circumstances, the standard modalities for acute inpatient dialysis at The Mount Sinai Hospital are intermittent hemodialysis or continuous venovenous hemofiltration (CVVH). But the COVID-19 pandemic resulted in a large increase in demand for renal replacement therapy (RRT), since acute kidney injury (AKI) is a complication of the disease.
Moving quickly to meet that demand, Mount Sinai drew on its expertise as one of the largest providers of outpatient peritoneal dialysis (PD) in New York City to offer PD to inpatients who developed AKI.
The sudden surge in cases “put a considerable burden on our inpatient dialysis system,” says Shuchita Sharma, MD, Assistant Professor of Medicine (Nephrology) at the Icahn School of Medicine at Mount Sinai. “We were limited in how many patients we could treat based on trained nursing staff and available resources. At the same time, COVID-19 patients who presented with AKI were hypercoagulable, which limited our ability to provide adequate hemodialysis.”
Realizing a different treatment modality was necessary to keep pace with rising demand for RRT, and to ensure sufficient resources were available to provide hemodialysis to hospitalized maintenance dialysis patients, Mount Sinai nephrologists implemented an acute PD program. The program was open to Mount Sinai patients who required inpatient dialysis but could not tolerate intermittent hemodialysis, or had been experiencing problems with it due to circuit clotting. Patients were excluded if they presented with a percutaneous endoscopic gastrostomy tube or were prone, or if physicians determined it was not safe to insert a PD catheter.
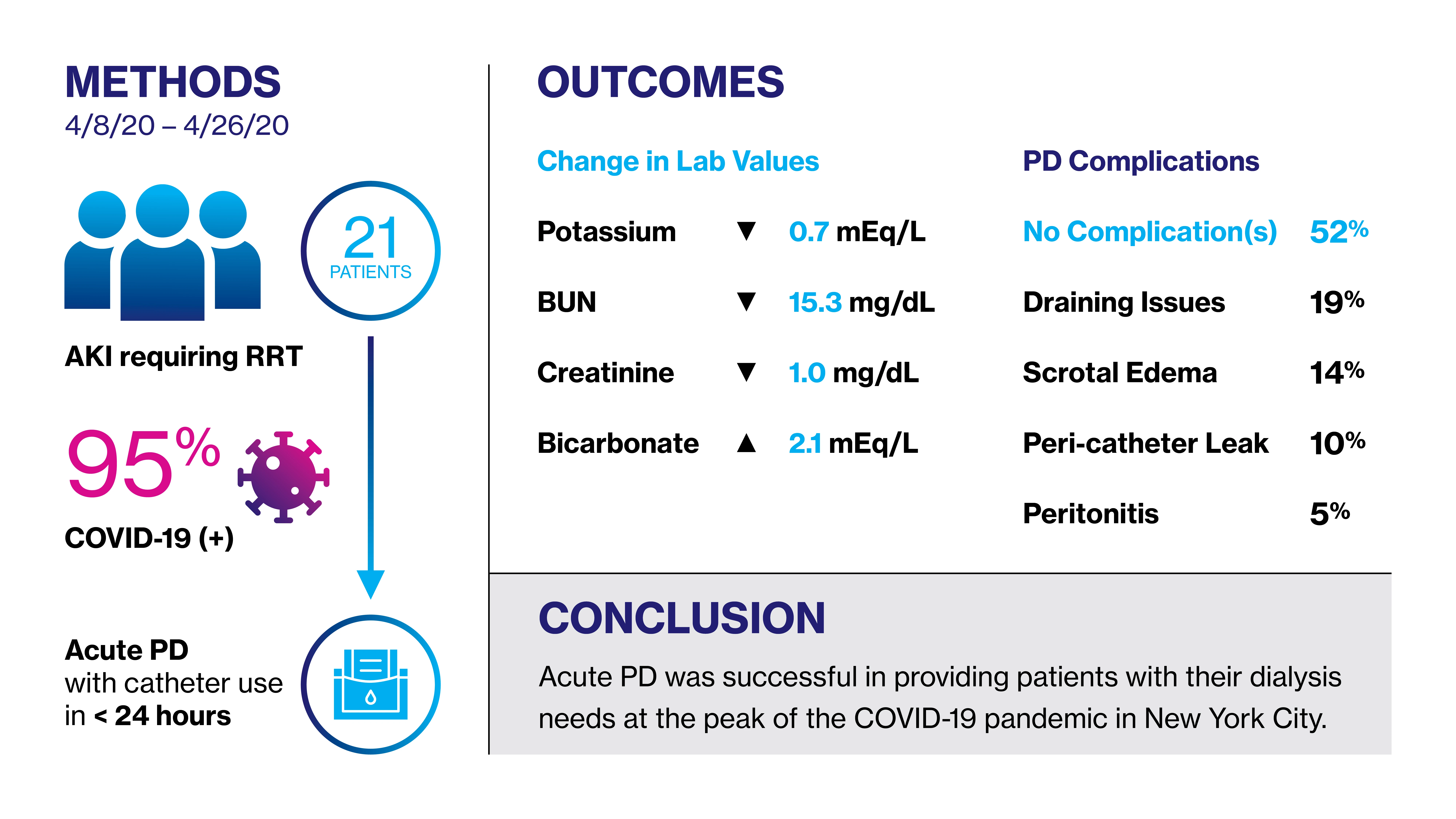
In total, 21 patients were recruited to the program between April 8 and April 26, 2020, some 95 percent of whom were COVID-19-positive, and none of whom had been on dialysis at the time of hospital admission. Participants were placed on continuous cycling PD, which not only helped protect front-line workers from infection but also ensured their workload remained manageable. Prior to the program, 12 patients had been placed on inpatient intermittent hemodialysis, CVVH, or both. Of the 21 participants, 12 presented with diabetes mellitus and 11 with hypertension as comorbidities. Four had a history of abdominal surgery and 16 were receiving mechanical ventilation at the time of catheter placement. The mean age of participants was 62. Forty-five percent of participants were male; 52 percent were Black, 33 percent were Latinx, and 14 percent were non-Latinx white. The mean weight of participants was 95 kg with a body mass index of 33 kg/m².
Source: JASN
The results of the program, which were published in the August 2020 Journal of the American Society of Nephrology, showed that nine patients had died by the date of submission. Three of the surviving patients achieved renal recovery, two were discharged on RRT, and seven remained hospitalized on RRT. “Historically, we have had a higher recovery rate among patients who undergo inpatient dialysis for AKI,” says Jaime Uribarri, MD, Professor of Medicine (Nephrology) at the Icahn School of Medicine at Mount Sinai. “We believe their comorbidities, coupled with COVID-19 infection, are the reason why the recovery rates are very low among participants in this program.”
Laboratory results among participants were based on mean values from day 3 of PD onward and the difference between values on the day prior to PD initiation and the day following termination. The mean change in potassium was a decrease of 0.7 meq/L. Serum bicarbonate increased by 2.1 meq/L and serum albumin levels were unchanged. However, there was a greater decrease in blood urea nitrogen on the last day of treatment versus the mean of day 3 onward (−15.3 versus −9.9 mg/dl, respectively).
“We have been pushing for increased utilization of peritoneal dialysis, both locally and nationally,” Dr. Uribarri says. “Given that these results are within the same range we typically see for hemodialysis patients, we can say that an inpatient acute PD program is not only completely feasible for meeting the needs of patients during a health care crisis but also as a general modality of therapy, and I believe more hospitals should consider adding it as an acute renal replacement therapy.”
Featured

Shuchita Sharma, MD
Assistant Professor of Medicine (Nephrology)
Jaime Uribarri, MD
Professor of Medicine (Nephrology)
