Telemedicine has transformed the delivery of patient care during the COVID-19 pandemic, maintaining safety while democratizing access to medical expertise, says David H. Adams, MD, the Marie-Josée and Henry R. Kravis Professor and Chair of the Department of Cardiovascular Surgery at the Icahn School of Medicine at Mount Sinai, and Cardiac Surgeon-in-Chief of the Mount Sinai Health System.
Dr. Adams, one of the world’s top mitral valve repair surgeons and the 99th president of the American Association of Thoracic Surgery, has long been a leader in educating surgeons around the world in advanced mitral valve repair techniques. In the last year, however, he has also become a champion of a comparatively simple clinical approach: using telemedicine to deliver better care to more people, in more places, at a lower cost.
“As a heart surgeon who specializes in repairing heart valves, I understand the need for hands-on medical care as much as anyone,” Dr. Adams says. “But in the early days of the current pandemic, when my hospital had to suspend all but the most urgent clinical visits, my team and I were surprised to learn how well we could evaluate and advise patients via telemedicine.”
Using the web to evaluate medical imaging and offer patients face-to-face video consultations proved highly effective, as well as preferable, especially for patients and their families. That is because it reduced their need to come into the hospital for consultation before surgery, Dr. Adams says, a welcome change even for those in New York City, in addition to those from across the region and around the country.
“Telemedicine enabled them to meet with us via video from the comfort of their own homes,”
Dr. Adams says, “reducing anxiety, travel, and unnecessary exposure risk.”
One such patient was 65-year-old Jan B. Her cardiologist, in Glen Falls, New York, had diagnosed her as suffering severe mitral valve regurgitation due to a flail posterior leaflet, as well as mild-to-moderate tricuspid regurgitation. Her echocardiogram also confirmed a reduced left ventricular function with a dilated left atrium. She otherwise remained asymptomatic with intact quality of life.
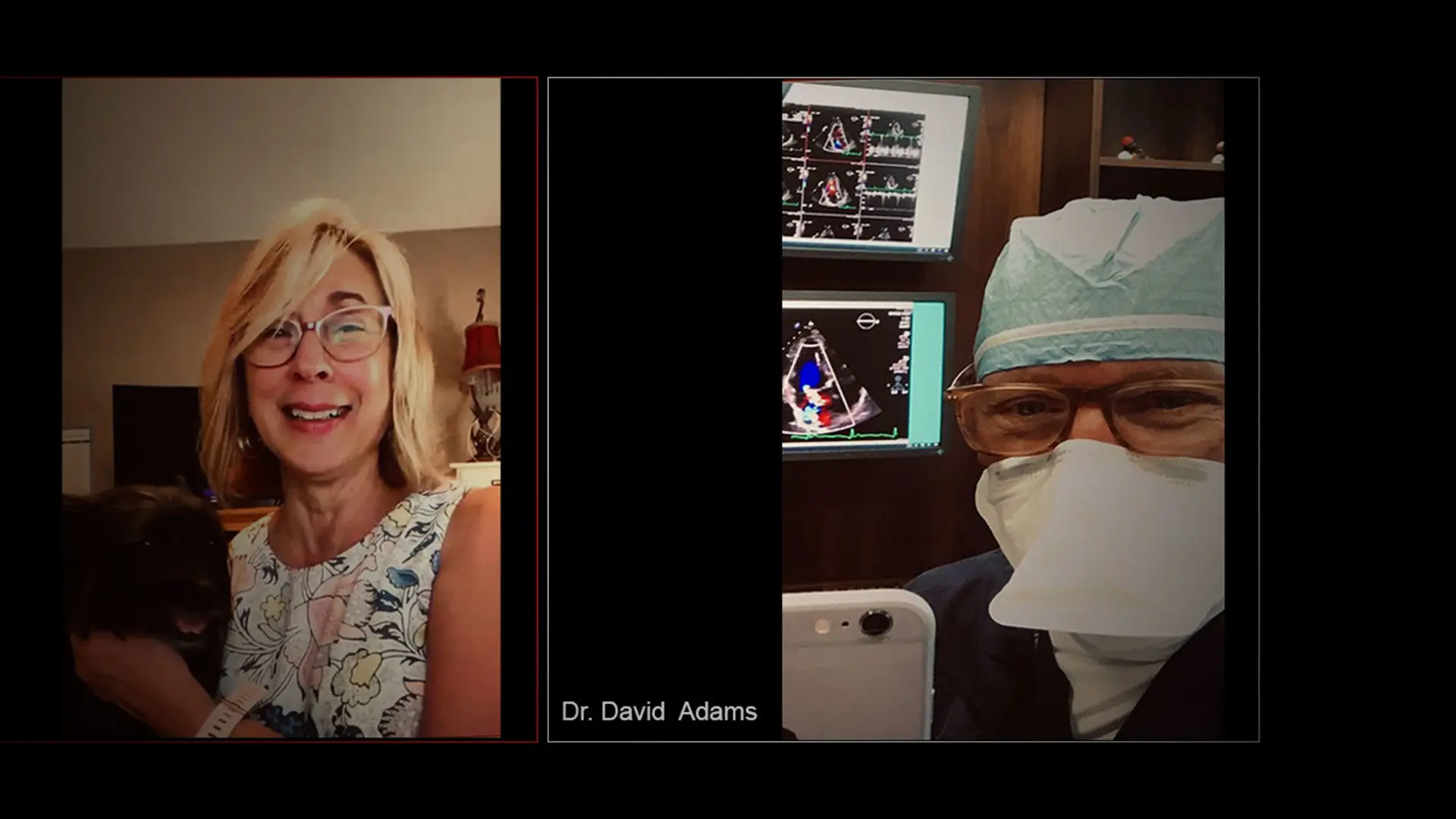
Seeking an expert in mitral valve repair, Jan’s cardiologist referred her to Dr. Adams just as the COVID-19 pandemic was first surging in the state, which made an in-person evaluation—a three-hour drive away—both risky and impractical. But thanks to pandemic-related changes to telehealth restrictions, Jan was able to arrange a video consultation with Dr. Adams and his partner Ahmed El-Eshmawi, MD, Assistant Professor of Cardiovascular Surgery, and Clinical Director of the Mitral Valve Repair Reference Center at The Mount Sinai Hospital.
“If we were to pair reciprocal licensing with permanent telehealth authority, providers everywhere could better collaborate to optimize health care for all Americans.”
David H. Adams, MD
“I liked being in my own space,” says Jan, who first spoke with Dr. Adams and Dr. El-Eshmawi from her living room, in June. “I had my dog, Cooper, on my lap. My husband, Mike, was there. And because the appointment was over video, I didn’t have to wear a mask. I would have liked to have met Dr. Adams in person first, but I loved him through telehealth,” she says. Ultimately, Dr. Adams and his team repaired her mitral valve with a minimally invasive procedure in July. The next week she was back in her home in upstate New York with a normally functioning mitral valve.
Two months after surgery, Jan was walking four miles per day, had completed her cardiac therapy, and had resumed light workouts. While acknowledging that telemedicine will never replace the need for hands-on examination, imaging, and surgery, Dr. Adams says it has the potential to strengthen diagnostic, preventive, and follow-up care—enhancing health outcomes and lowering long-term costs for all stakeholders.
The Centers for Medicare and Medicaid Services (CMS) approved delivery of more than 80 new services via telemedicine in 2020, and since then, more than 11.3 million of the program’s beneficiaries have accessed such care from the safety of their own homes. However this ability to offer remote care has only been granted on a temporary, emergency basis during the pandemic.
“Based on what we’ve learned, many of my colleagues across the country are urging federal and state authorities to make this authority permanent,” Dr. Adams says. “By permanently expanding medically appropriate telehealth options, we can dramatically improve our health care system.”
While financial data related to COVID-related telehealth measures is not yet available, an analysis in 2016 found that previous telehealth programs in the Veterans Administration had reduced hospitalizations by as much as 40 percent, saving $6,500 per enrollee in just one year. More broadly, telehealth can also help reduce unnecessary emergency room trips for patients with chronic conditions, by improving long-term, high-quality, cost-effective preventive care.
Another reform being sought is nationwide reciprocity in medical licensing. Currently, state-by-state licensing requirements prevent most specialists and other medical experts from providing diagnostic services, even second opinions, outside of their own state. Advocates for reform say this denies Americans in rural and other underserved areas equal access to a full range of medical expertise and advanced care. During the COVID-19 pandemic, CMS and many states have removed such barriers by recognizing the credentials of certified health professionals regardless of which state licensed them. However, this waiver is also temporary.
At the height of the pandemic, Dr. Adams organized a national coalition of more than 200 cardiovascular leaders—including more than 70 current or past presidents from major cardiovascular societies, such as the American College of Cardiology, the American Heart Association, and the American Society of Echocardiography—that urged members of Congress to make recent, temporary telehealth changes permanent. To date, that has not yet happened.
“If this pandemic has taught us anything, it’s that a piecemeal or parochial approach to public health undermines everyone’s safety,” Dr. Adams says. “By contrast, if the United States were to pair reciprocal licensing with permanent telehealth authority, providers everywhere could better collaborate to optimize health care for all Americans, including those who need to visit hospitals for hands-on treatment, or just get a second opinion to make a more informed decision about their own care. Telehealth just makes common sense for patients, providers, and third-party payers alike.”
Featured

David H. Adams, MD
Marie-Josée and Henry R. Kravis Professor and Chair of Cardiovascular Surgery, and Cardiac Surgeon-in-Chief, Mount Sinai Health System

Ahmed El-Eshmawi, MD
Assistant Professor of Cardiovascular Surgery, and Clinical Director of the Mitral Valve Repair Reference Center