At the height of the 2020 pandemic, a team of researchers at Mount Sinai found that patients with heart failure (HF) who contracted COVID-19 were at a significantly higher risk of complications. Their study—the largest of its kind—found that a history of heart failure was associated with a twofold greater risk of mechanical ventilation, a nearly twofold increased rate of death, and a length of hospital stay that averaged two days longer than those without heart failure. The findings were published in November 2020 in the Journal of the American College of Cardiology.
“Because heart failure patients have a high prevalence of frailty, renal dysfunction, and other comorbidities, it was assumed their prognosis is worse if they contract COVID-19, though there was little data to confirm that,” says Anuradha Lala, MD, Assistant Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai, and senior author of the study. “Through our work, we showed the magnitude of that risk. The implications are that we need to think very carefully about how we triage and treat these patients once hospitalized, possibly translating to more aggressive therapy.”
The authors conducted a retrospective analysis of 6,439 adult patients age 18 and older admitted for COVID-19 at one of five Mount Sinai hospitals between February 27 and June 26, 2020. Clinical characteristics and outcomes (length of stay, need for intensive care unit, mechanical ventilation, and in-hospital mortality) were captured from electronic health records.
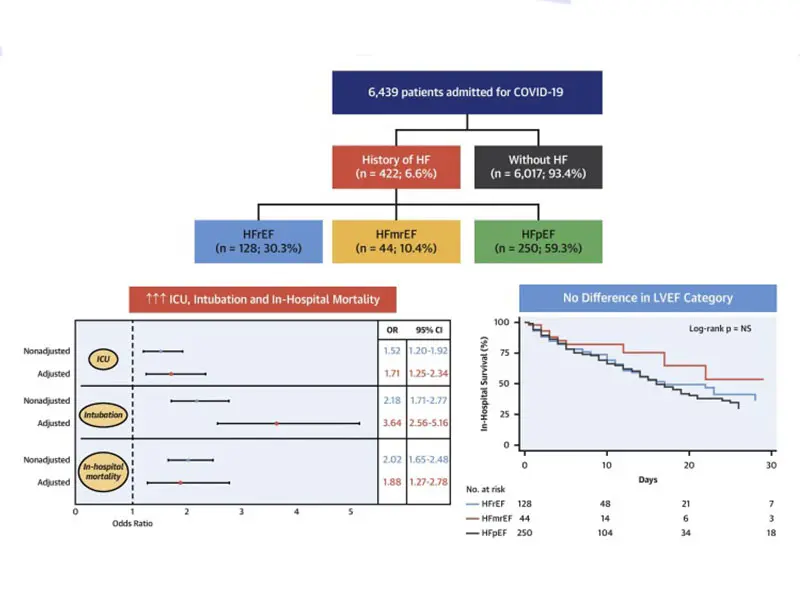
Graphical abstract of the study. Top panel: Consort diagram of the study population. Bottom right panel: Kaplan-Meier survival curves in patients hospitalized with COVID-19, according to left ventricle ejection fraction. Bottom left panel: The effect of history of heart failure on outcomes in patients admitted for COVID-19.
The mean age of the patients was 63.5 years, and 45 percent were women. Compared with patients without HF, those with previous HF experienced a longer length of stay (eight days vs. six days), an increased risk of mechanical ventilation (22.8 percent vs. 11.9 percent), and mortality (40 percent vs. 24.9 percent).
The highest risk cohort consisted of patients with New York Heart Association functional class III or IV heart failure symptoms and/or moderate or severe mitral regurgitation. Importantly, the study found no major differences in clinical outcomes among patients with preserved, reduced, or mild left ventricular ejection fraction. Additionally, researchers found that there was no association between indicated medications for heart failure, specifically renin-angiotensin-aldosterone system inhibitors (RAASi), and worse outcomes for COVID-19 patients.
“Our study reinforced the importance of maintaining RAASi in patients where their use is strongly indicated,” says Jesús Álvarez-García, MD, PhD, postdoctoral fellow in Advanced Heart Failure and Transplantation at the Icahn School of Medicine at Mount Sinai, and lead author of the study.
Through a better understanding of the mechanisms underlying the high risk of COVID-19 in patients with heart failure, physicians will gain fresh insights into what therapies might be effective, Dr. Lala says. “Inflammation is common to both chronic heart failure and acute COVID-19. As such, anti-inflammatory drugs might be particularly effective in mitigating adverse events in this population” she says.
Dr. Lala also emphasized the importance of basic preventive and safety measures, pointing out that physicians should remind this highly vulnerable patient cohort to wear masks, maintain social distancing, and wash their hands frequently. “I take time out of each visit with our heart failure patients to reinforce this message,” she points out, “and to make clear to them the importance of an ongoing dialogue with their physician in the midst of a pandemic.”
Featured

Anuradha Lala, MD
Assistant Professor of Medicine (Cardiology), Icahn School of Medicine at Mount Sinai

Jesús Álvarez-García, MD, PhD
Postdoctoral Fellow in Advanced Heart Failure and Transplantation, Icahn School of Medicine at Mount Sinai