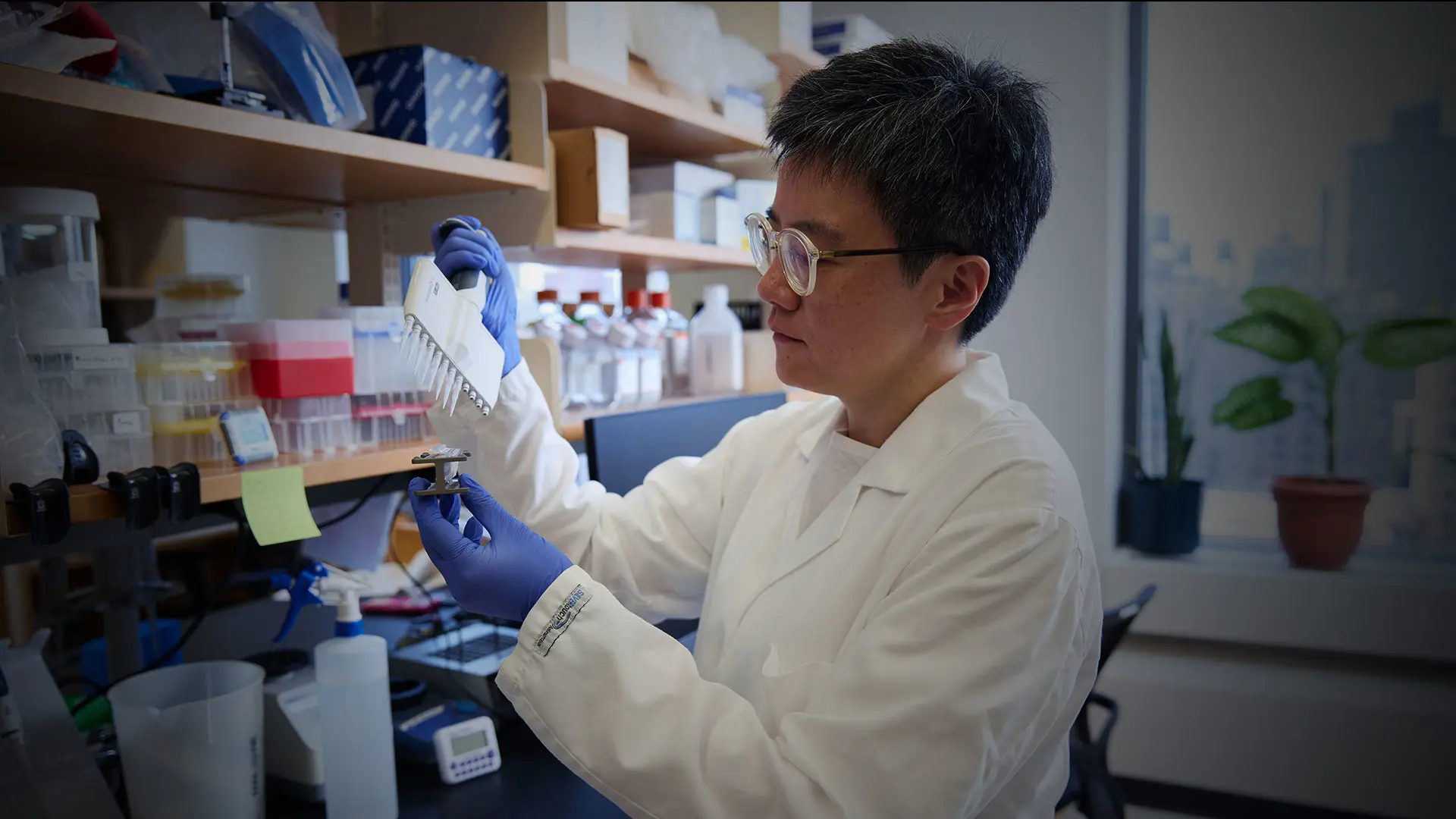
The liver is renowned for its remarkable ability to heal itself. “Even the ancient Greeks had myths about the liver regenerating,” notes translational scientist Shuang (Sammi) Wang, PhD, Assistant Professor of Medicine (Liver Diseases) at the Icahn School of Medicine at Mount Sinai.
But while scientists have made significant strides in detailing the mechanisms of regeneration in healthy livers, there is still much to learn about how liver disease disrupts this process.
In a research program funded by the National Institutes of Health, Dr. Wang is exploring how disorders such as metabolic dysfunction-associated steatohepatitis (MASH) affect the regenerative mechanisms within hepatocytes—and how those mechanisms might be manipulated to improve regeneration in patients with chronic liver disease.
Liver Zonation: Hepatocyte Identity and Function
Researchers have mapped out a detailed description of the cellular processes underlying regeneration in normal liver tissue. When part of the organ is resected, the remaining hepatocytes transiently revert to a more progenitor-like state. They proliferate rapidly to regenerate the missing tissue, then shift back to their normal differentiated functions, Dr. Wang notes.
Less understood is what happens in an ailing liver. In chronic diseases such as MASH, hepatocytes are less able to regenerate as the illness progresses. One question is whether they lose the ability entirely or whether some process—such as fibrosis—is blocking their regenerative capacity. Detangling these possible scenarios may suggest ways to restore regeneration.
To learn more, Dr. Wang is using mouse models of MASH to probe the regenerative capacities of hepatocytes from different zones within the liver. Hepatocytes have distinct identities based on the zone in which they are located. The three major zones are defined by the amounts of oxygen and nutrients the cells receive based on their proximity to major blood vessels.
For Dr. Wang, a key question is how different zones of hepatocytes undergo regeneration, in both healthy livers and those damaged by chronic disease.
“Are certain zones more regenerative? Do hepatocytes with different zonal identities regenerate each other?” she asks. “I am also exploring the more complicated question of what happens in each of those zones when liver disease stops regeneration.”
Dr. Wang is trying to understand the different strategies that liver cells use to regenerate after disease.

Analysis of mouse livers suggests that hepatocytes sometimes become larger, rather than regenerating, in earlier stages of MASH.
Typically, hepatocyte identity is determined by location. In mouse models, Dr. Wang has shown that severe chemical injury disrupts zonation and the proportion of hepatocytes in each zone. Yet changing zonal identity may not be the only way that liver cells respond to disease. In milder, earlier stages of MASH, she found that lipid-laden hepatocytes respond to injury by becoming hypertrophic rather than regenerating. “Initially, to make up for the lack of regeneration, the hepatocytes can expand in size to increase their metabolic function,” she says. These findings begin to unveil several different strategies that the liver can adopt to meet its regenerative needs in the presence of disease.
The discoveries could point toward new therapeutic pathways. While regeneration is a remarkable process, it presents some risk. A subset of people with MASH develops liver cancer—and both regeneration and cancer involve cell proliferation. Treatments that stimulate cell proliferation could have the unintended consequence of increasing cancer risk. Switching cell identity or promoting hypertrophy to increase metabolic function could represent safer targets for new therapies to promote regeneration while avoiding cancer.
Promoting Regeneration for Chronic Liver Diseases
Despite the risk of runaway proliferation, regeneration remains a promising target for treating chronic liver diseases. Indeed, some treatments may already be promoting regeneration, Dr. Wang has found. Resmetirom, the first treatment for MASH, was approved based on its ability to reduce fat content in hepatocytes, she notes. Investigating the drug in her mouse models, she showed that it also promoted proliferation in the livers of sick mice.
“That had not previously been proposed as a mechanism of action for resmetirom. We only knew that it reduced fibrosis,” Dr. Wang says. “This pro-regenerative function suggests it may benefit other kinds of liver diseases, which could really expand its potential use.”
Dr. Wang and her colleagues are currently seeking a clinical partner to test resmetirom (or similar drugs in the development pipeline) in patients with liver diseases other than MASH, to see if they might enhance regeneration and improve patient outcomes. Meanwhile, her laboratory continues to explore the basic science of hepatocyte identity and regeneration.
Mid-zonal hepatocytes, buried deep in the liver farthest from the blood supply, appear to be both larger and more regenerative than cells in the other zones. Her research suggests resmetirom may promote regeneration primarily within those mid-zonal hepatocytes.
“That finding helps connect the dots,” she says. “Now we are looking for different ways to manipulate mid-zonal hepatocytes, both to enhance their function and to make them more regenerative without promoting cancer.”
While much remains to be discovered about the regenerative abilities of hepatocytes, the approval of resmetirom in 2024 has energized the field, Dr. Wang adds.
“There is still a lot of room to explore and grow, but we have uncovered a lot of biology that is ripe for translation,” she says. “It speaks to the importance and value of basic research and underscores how much hope is on the horizon.”