Mount Sinai launched the Institute for Liver Research in early 2024 to harness the wealth of clinical and research strengths across the institution, potentially benefiting countless individuals coping with chronic liver disease.
The first two pilot projects now underway offer ample evidence of where the Institute’s strategic priorities lie. Both were chosen from among 11 applications submitted by basic, translational, or clinical research teams, and awarded one-year grants of $30,000 each in hopes of generating preliminary data sufficient to stimulate broader funding and research collaborations.
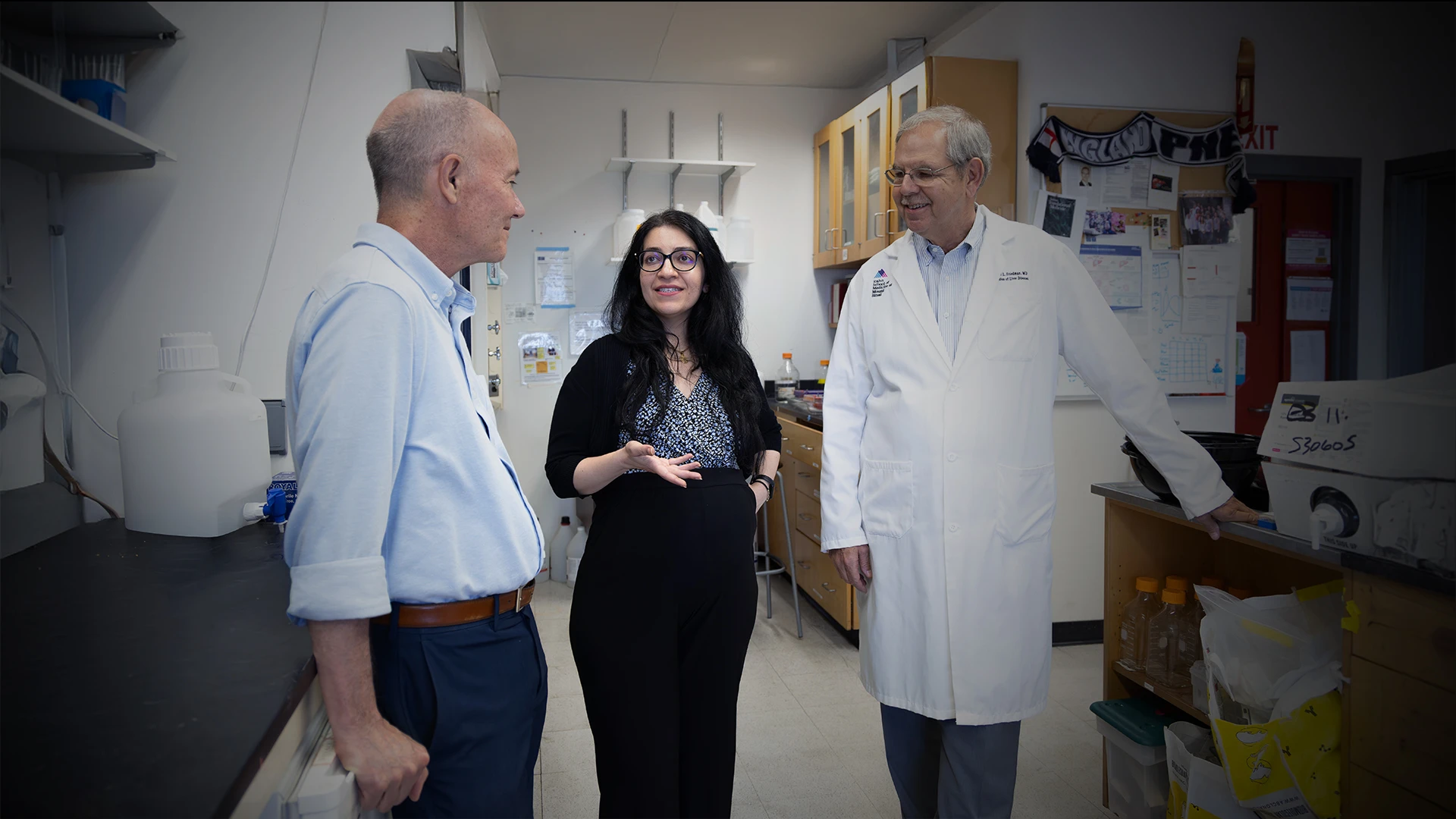
“These projects couldn’t be more different in terms of their scope and the resources they draw on, yet both will significantly enhance our knowledge about the diagnosis and treatment of liver disease,” says Scott Friedman, MD, Director of the Institute for Liver Research at the Icahn School of Medicine at Mount Sinai.
“One project brings together our capabilities in genomics and genetic sequencing of patients to determine how many and which abnormalities are linked to liver disease, while the other proposes to develop a lipid nanoparticle platform for hepatic stellate cell-specific drug delivery in humans to reduce fibrosis in patients with chronic liver disease,” says Dr. Friedman, who stepped down in 2024 after 23 years as Chief of the Division of Liver Diseases to assume his new role.
In keeping with its cross-disciplinary research focus, the Institute required that all projects be performed as a new collaboration by two or more faculty members in separate laboratories at Mount Sinai. Seasoned scientists reviewed each of the applications and made their recommendations based on novelty, innovation, and the likelihood of eventual extramural or industry funding.
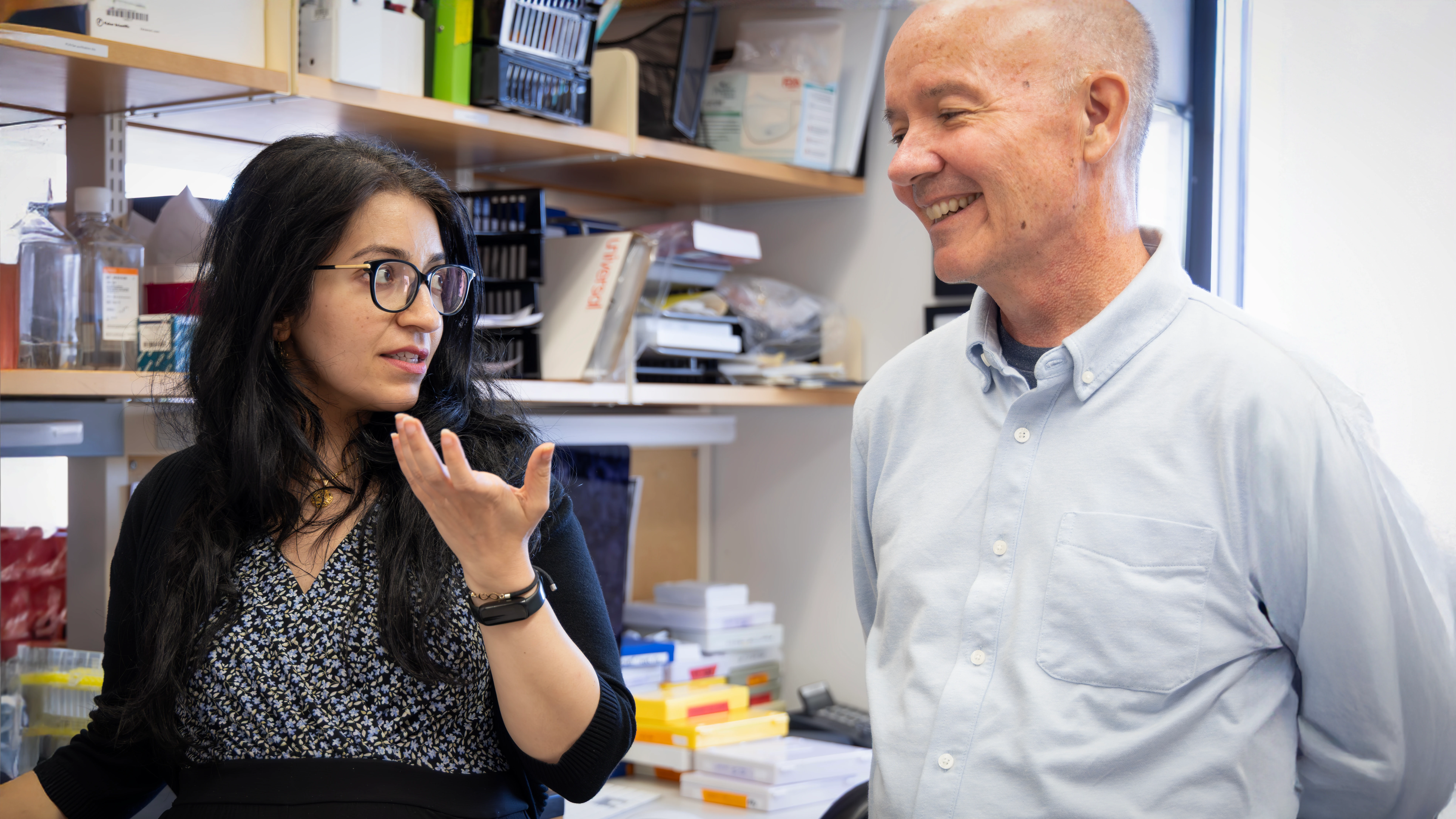
The project on somatic mutations and the risk of chronic liver disease pairs two eminently qualified researchers with complementary skills and knowledge sets. Samira Asgari, PhD, Assistant Professor of Genetics and Genomic Sciences, is an expert in human genomics and statistical genetics whose lab was the first to report rare genetic variants that can cause extreme susceptibility to common respiratory viruses in otherwise healthy children; it also identified genetic factors leading to life-threatening sepsis in children. In her new Institute study, she plans to build on her expertise to better understand the biological mechanisms that connect germline and somatic genetic variants in patients with chronic liver disease.
Her partner is Michael Murray, MD, who joined Mount Sinai in 2023 as Clinical Director of the Institute for Genomic Health following years of cutting-edge clinical integration work in genomic medicine at Harvard and Yale medical schools and Geisinger Health System. In his new role, Dr. Murray heads up a team whose members are developing a prioritized list of genes associated with significant risk of disease.
“He is more of a clinical geneticist whose background is uniquely bound to the goals of this project, namely linking changes in DNA sequences to the presentation of liver disease,” says Dr. Friedman. To that end, Dr. Murray will extensively leverage the Mount Sinai Million Health Discoveries Program, one of the largest and most culturally diverse biobanks in the world, which is accelerating the effort to join genetics with mainstream medicine.
The second pilot project, on developing lipid nanoparticles for treating liver disease, also joins two highly experienced Mount Sinai scientists. Shuang (Sammi) Wang, PhD, Assistant Professor of Medicine (Liver Diseases), is a translational researcher with a long-standing history of using mouse models to study hepatic stellate cell (HSC) biology, especially in the context of liver fibrosis, the strongest predictor of patient mortality in chronic liver disease. Her partner is Xucheng Hou, PhD, Assistant Professor of Immunology and Immunotherapy, an expert in integrating novel lipid materials, mRNA structure engineering, and lipid nanoparticle (LNP)-mRNA-based cell therapies. Their combined strengths in LNP design and HSC target selection will be pivotal in their new study pursuing HSC-specific lipid nanoparticle formulations that can provide a novel platform for developing much-needed antifibrotic drugs to combat liver disease.
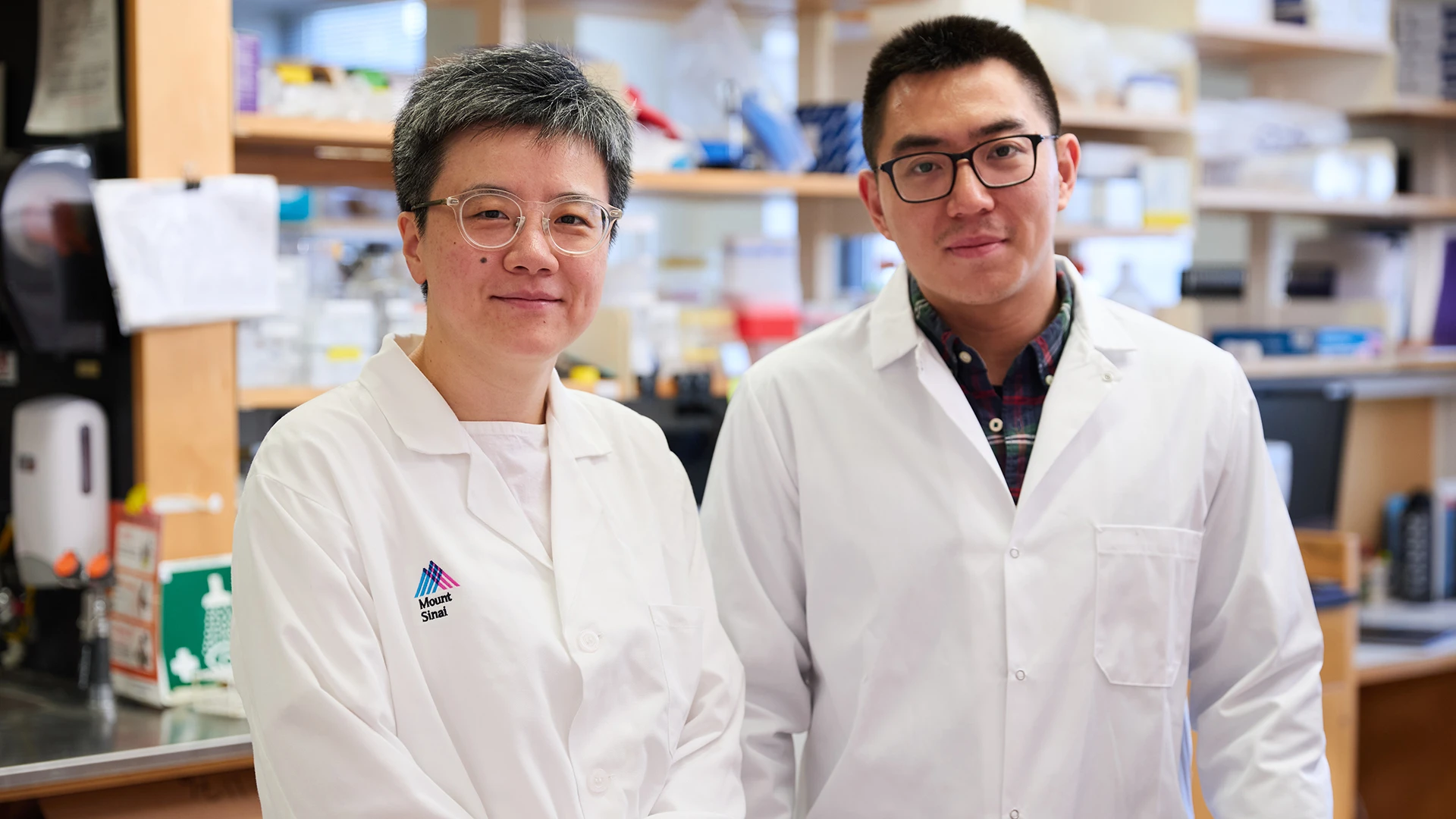
Dr. Wang, left, and Dr. Hou are studying lipid nanoparticles with the ultimate aim of developing new antifibrotic drugs for liver disease.
Beyond these two funded projects, Dr. Friedman lauds each of the nine that weren’t selected and holds out hope that some could be reconsidered down the road. One project he views as quite promising is focused on primary sclerosing cholangitis (PSC), a challenging liver disease. It explores the function of a novel autoantibody against a protein known as integrin αvβ6, which is present in patients with PSC and ulcerative colitis. This suggests it may be contributing to the pathophysiology of both diseases, especially since both frequently occur in the same patient. Another project he finds intriguing is research underway at Mount Sinai that is taking livers rejected for human transplantation and perfusing them with isotopes to better understand the metabolism of liver cells and inflammatory cells in the liver.
“What became apparent to me as we began organizing the Institute is the extraordinary amount of talent we have across so many different domains within the medical school and the Mount Sinai Health System that can be deployed to study liver disease,” emphasizes Dr. Friedman, whose pioneering research helped pave the way for a new era of antifibrotic therapies for liver disease, now in clinical trials. “Our goal is not to reinvent things from scratch, but to leverage the resources and strengths we already have in genetics, molecular biology, imaging, and other fields to advance the science of liver disease and the discovery of innovative new therapies.”
Featured
Scott Friedman, MD
Irene and Dr. Arthur M. Fishberg Professor of Medicine; Dean for Therapeutic Discovery; Director, Institute for Liver Research