More than 20,000 World Trade Center (WTC) General Responders—a group of workers and volunteers who were part of the rescue-and-recovery effort that followed the 9/11 attack—charged into a toxic cloud of dust, chemicals, and airborne particulate matter 22 years ago. Today, Mount Sinai researchers continue to uncover the toll that exposure took on the lives of these heroic individuals.
In two of the latest studies, investigators found that the odds of having moderate-to-severe hepatic steatosis, a component of nonalcoholic fatty liver disease, are more than three times higher among WTC General Responders than in a comparison group of nonresponders, and demonstrated that the risk is greatest for those who arrived earlier at the disaster site.
The federally funded World Trade Center Health Program—of which Mount Sinai is one of five Clinical Centers of Excellence—has provided compelling evidence of the epidemiologic link among exposure to the WTC dust cloud and adverse health effects. Prior studies have measured, for example, lung function abnormalities and the nine-year cumulative occurrence of asthma, sinusitis, and gastroesophageal reflux disease. Another Mount Sinai study found an increased risk of prostate cancer in recovery workers and community members living near the WTC site compared to the general public.
The latest studies are the first investigations of hepatic steatosis in members of the Mount Sinai WTC General Responder Cohort. Both studies used chest CT scans to detect moderate-to-severe hepatic steatosis and were supported, in part, by a grant from the National Institute for Occupational Safety and Health, a component of the Centers for Disease Control and Prevention. The first study revealed that 16.2 percent of 154 WTC General Responders studied had hepatic steatosis, compared to 5.3 percent of 170 non-WTC study participants. The study, in Clinical Imaging, was conducted by researchers in the Division of Liver Diseases and the Department of Diagnostic, Molecular and Interventional Radiology at the Icahn School of Medicine at Mount Sinai. The findings accord with data on liver steatosis in WTC-exposed firefighters reported by researchers at NYU Langone Health and the Albert Einstein College of Medicine.
“Likely contributors to the development and higher rates of liver disorders in the General Responder Cohort are the complex pathophysiologic effects of exposure to particulate matter and airborne toxins, including organic chemicals,” says Andrea D. Branch, PhD, Professor of Medicine (Liver Diseases) at Icahn Mount Sinai, and co-author of the study. “Organic chemicals can disrupt cellular metabolism and increase the fat content of hepatocytes, the predominant cell in the liver. This can lead to hepatic steatosis.”
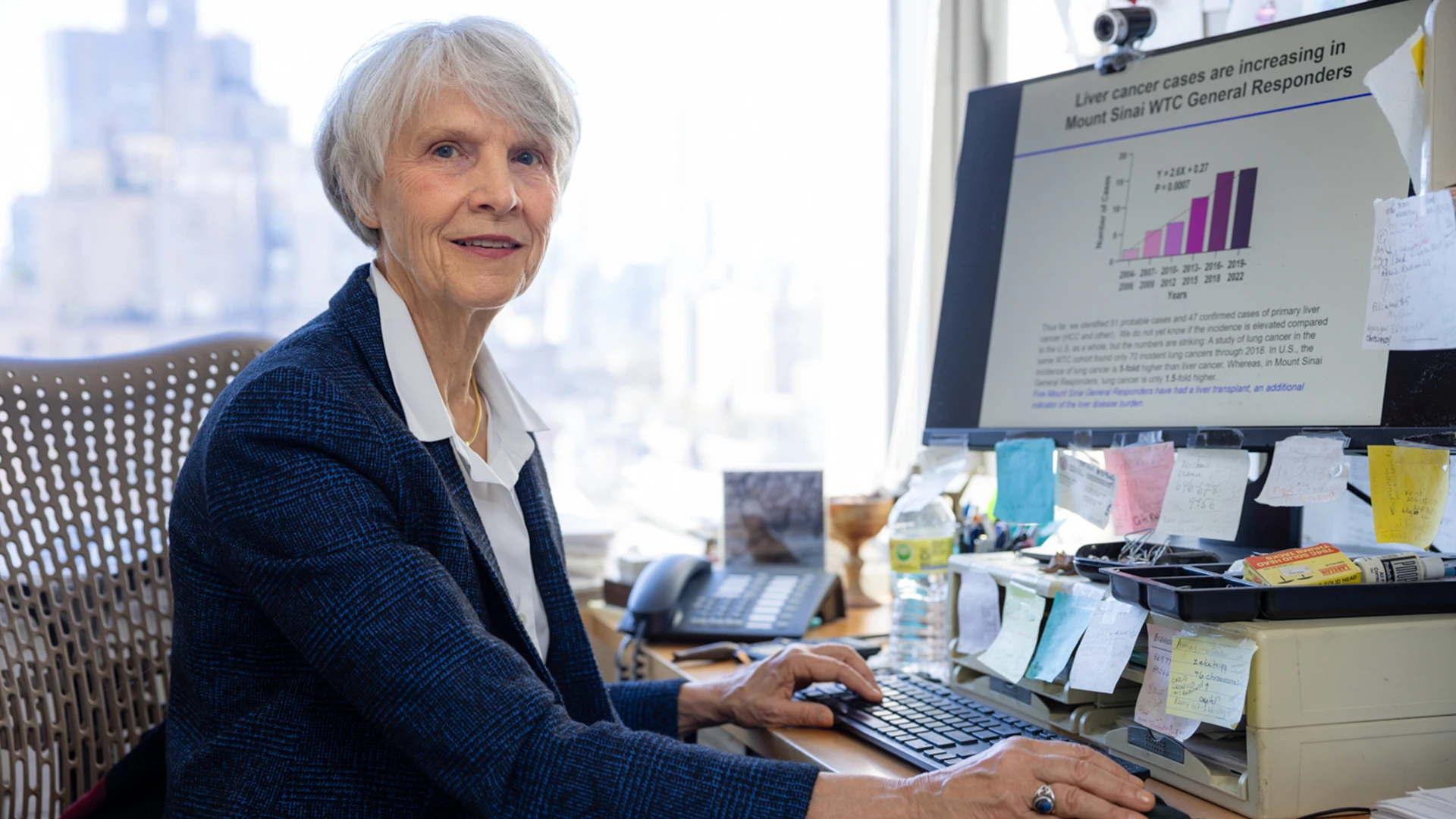
Andrea D. Branch, PhD, is a leader of the first investigations of hepatic steatosis in members of the Mount Sinai WTC General Responder Cohort.
In a further detailed analysis within the same study, the researchers compared WTC General Responders with and without liver steatosis to each other. Interestingly, they found that responders with liver steatosis were more likely to have coronary artery calcification, highlighting the need to comprehensively investigate the long-term effects of exposure to the WTC dust cloud on multiple vital organs.
In the second WTC-related study, the Mount Sinai team examined the relationship between the intensity of WTC dust cloud exposure and the risk of hepatic steatosis in the Mount Sinai General Responder Cohort. What they found, reported in American Journal of Industrial Medicine, was a significant difference in liver steatosis according to the worker’s time of arrival at the WTC site. Specifically, the prevalence of steatosis was highest among those who arrived first and decreased with later arrival times. Greater liver steatosis was indicated by a mean decrease in the attenuation of the CT signal.
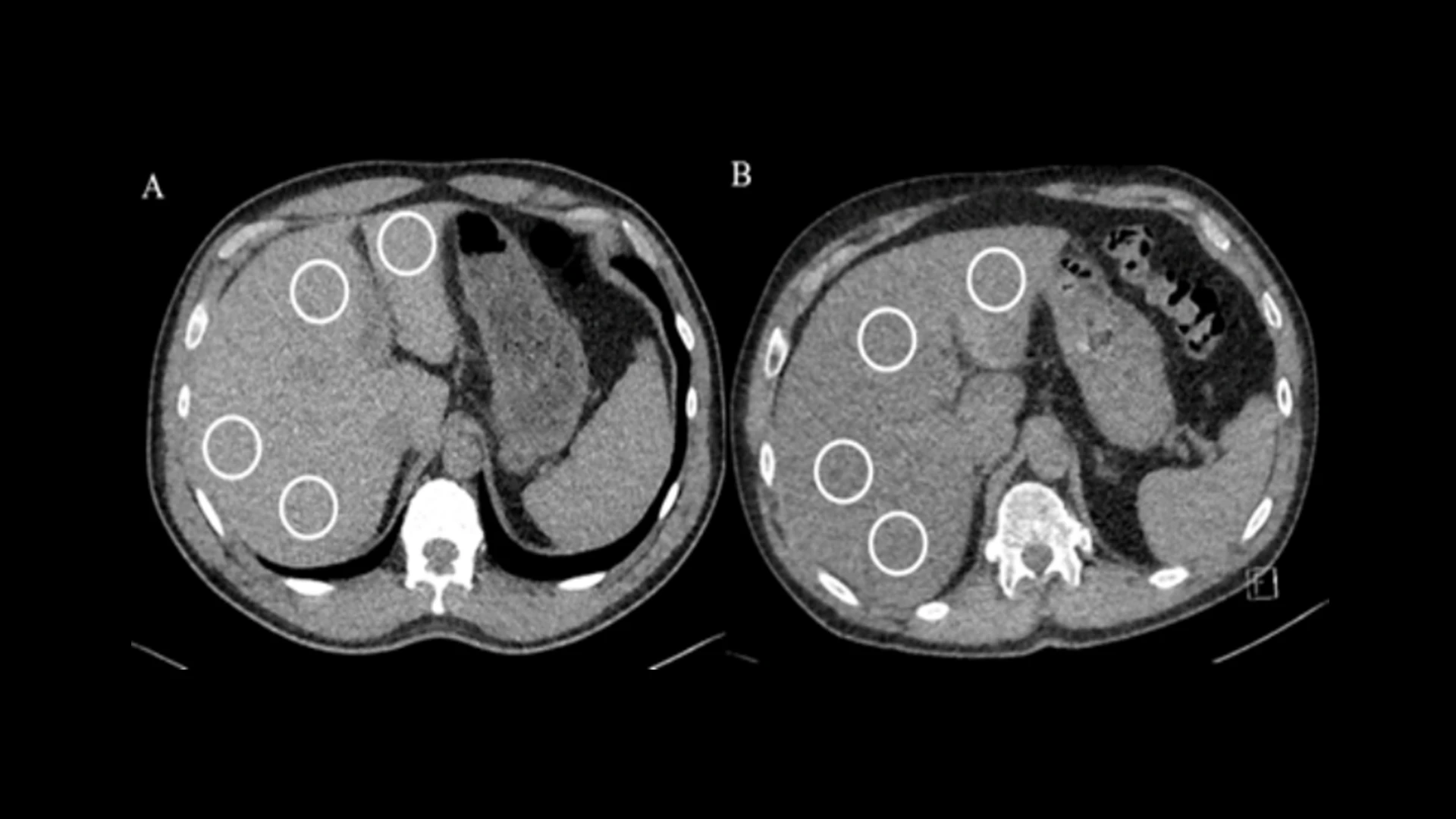
Liver density measurements on non-contrast chest CT in WTC participants. Averaged normal liver attenuation (59.5 HU) was noted in a 56-year-old male (A) and averaged lower liver attenuation (25 HU) was noted in a 57-year-old male (B), consistent with hepatic steatosis. Region of interest (white circles) measurements were placed in the right posterior, right anterior, left medial, and left lateral segments of the liver to determine liver attenuation, avoiding lesions and vessels.
Providing an enabling platform for the pair of Mount Sinai investigations was the creation of an automated algorithm able to quickly and reproducibly measure liver attenuation on non-contrast CT scans. This cutting-edge technology, developed by Claudia Henschke, MD, PhD, Professor of Diagnostic, Molecular and Interventional Radiology at Icahn Mount Sinai, represented a significant improvement over the standard practice of relying on radiologists to manually identify regions of interest in each segment of the liver and then measure the attenuation within each region of interest.
“From this methodology we were able to calculate a more than threefold increase in the odds of a General Responder having moderate-to-severe hepatic steatosis as defined by CT liver attenuation below 40 HU,” explains Dr. Henschke, a pioneer in the field of diagnostic radiology. “While further work is needed, we’re hopeful these results will underscore the importance of referring World Trade Center Responders who are below that clinical threshold to a hepatologist for additional evaluation and possible treatment.”
