Decades of research into how the activation of hepatic stellate cells leads to the scarring characteristic of liver fibrosis, and potentially to cirrhosis, are beginning to bear fruit, with Mount Sinai researchers taking center stage.
Using the latest single-cell RNA sequencing technologies and 3D imaging, the researchers have discovered a dense network of stellate cell-to-stellate cell (autocrine) signaling that emerges in advanced fibrosis. More importantly, they have identified at least one antifibrotic drug target, and a drug with which to target it—findings that may yield effective treatments for a disease that currently has no approved therapies.
“We are using the newest tools to probe the mechanisms of scarring in a way that hasn’t been done before, and that’s beginning to yield real dividends in uncovering new drug targets and new drugs,” says Scott Friedman, MD, Irene and Dr. Arthur M. Fishberg Professor of Medicine at the Icahn School of Medicine at Mount Sinai and Chief of the Division of Liver Diseases, who first identified hepatic stellate cells in 1985. “When stellate cells get activated, they become a virtual factory for making scar proteins, and if we can turn those cells off, we may have found the pathway to new treatments. By developing in our lab a whole new model for how scarring advances, we’re closer than ever to that holy grail.”
The groundbreaking work that has brought the Mount Sinai team to this stage was described in a paper recently published in Science Translational Medicine. Specifically, researchers found that, in addition to producing scarring proteins, hepatic stellate cells serve as a critical signaling hub that dictates how these cells communicate with one another as part of the autocrine circuit.
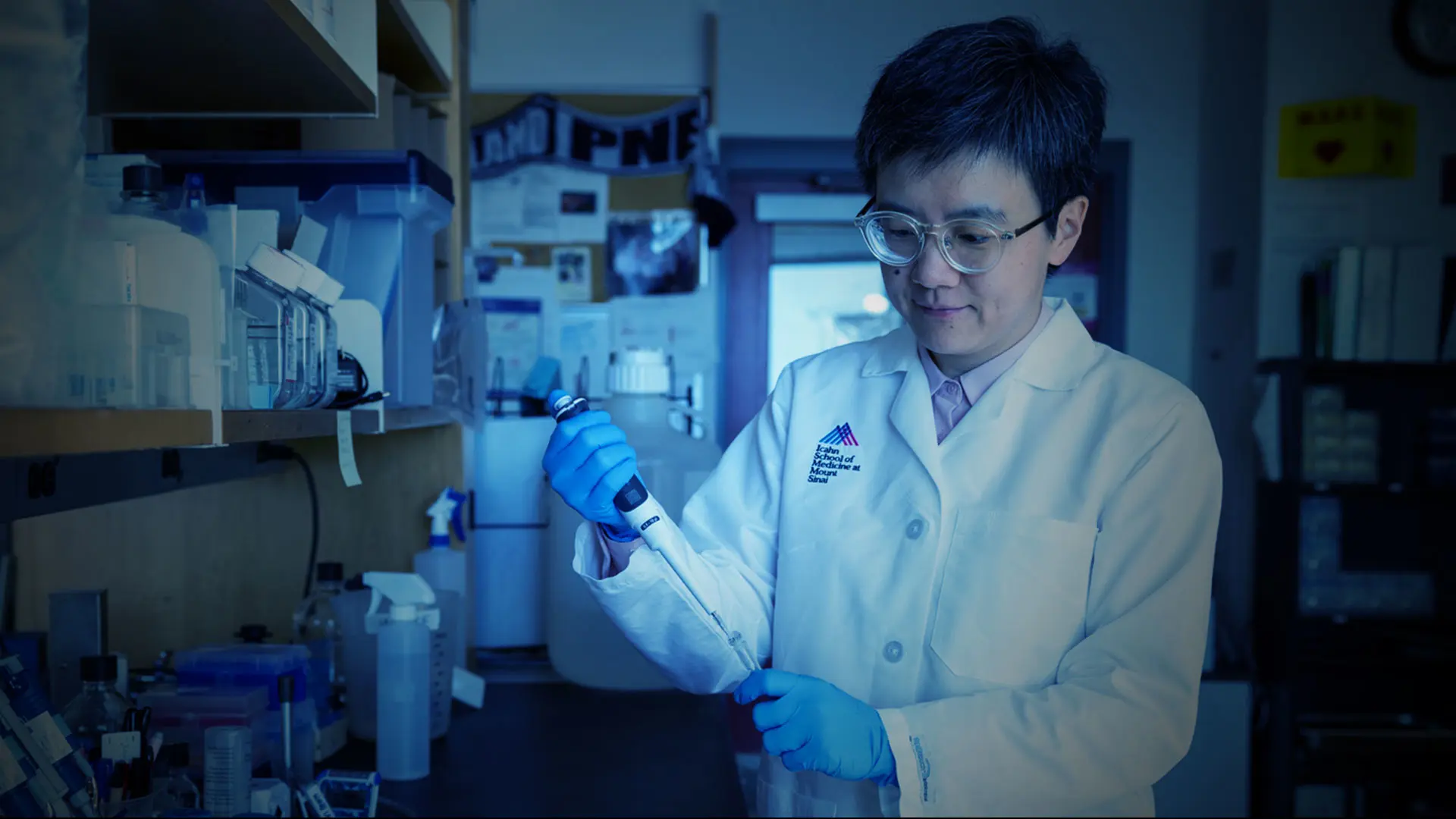
“Our mathematical modeling showed how conditions such as tissue injury could predict the development of a self-sustaining autocrine signaling circuit, and that in advanced liver disease, almost all hepatic stellate cells are enmeshed in that dense interconnected network that supports short-range cell signaling,” explains Shuang (Sammi) Wang, PhD, Assistant Professor of Medicine (Liver Diseases) at Icahn Mount Sinai and lead author of the study. “This finding not only establishes proof of principle for an autocrine pathway in advanced liver fibrosis but, more importantly, suggests that treatment for the disease may be most effective if it leverages autocrine targets that predominate in the late stage.”
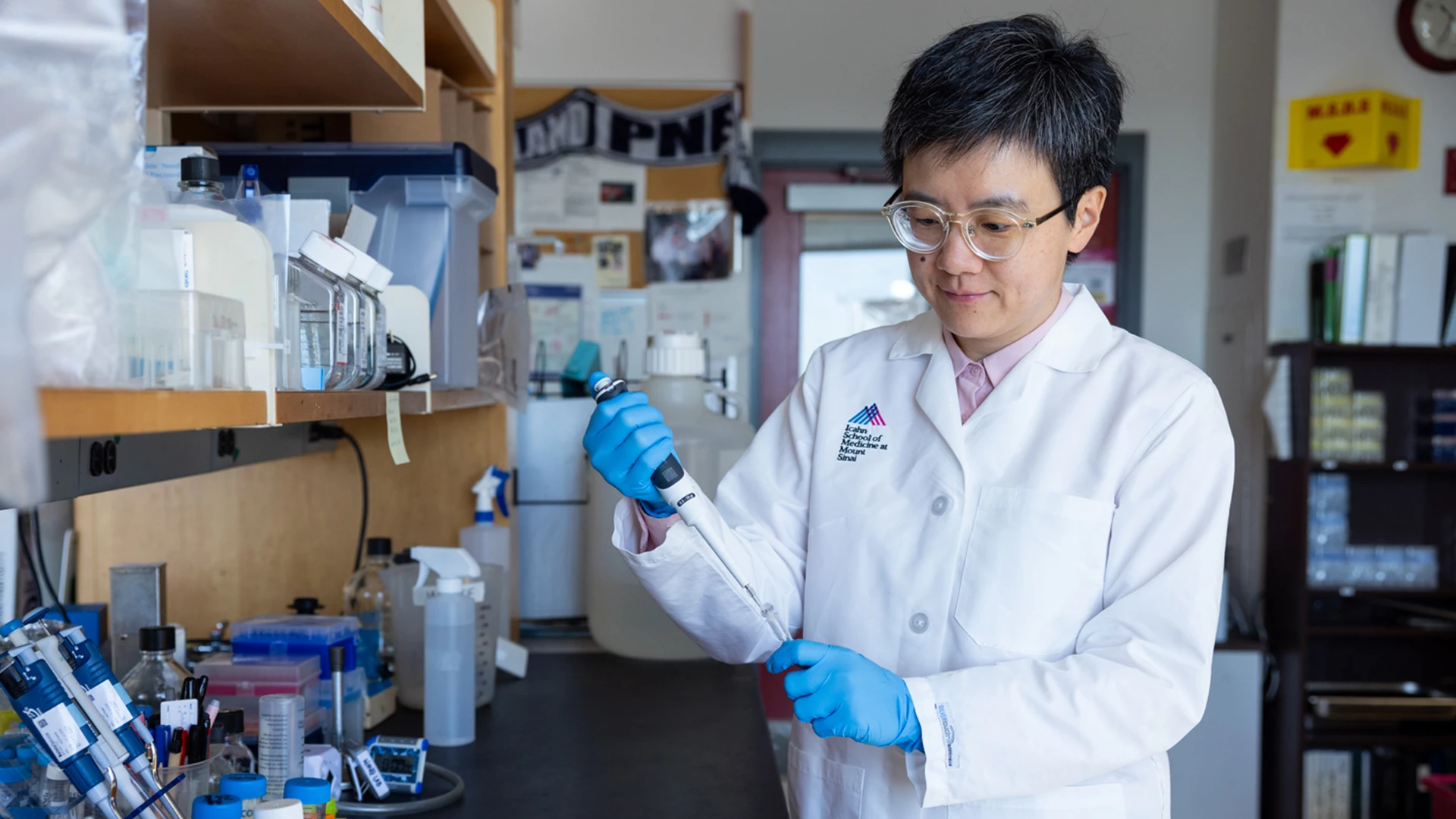
Dr. Wang is part of a Mount Sinai research team that has made recent breakthroughs in the understanding of liver fibrosis.
As a result of the obesity epidemic, about a third of all adults in the United States are believed to have nonalcoholic fatty liver disease, and about 20 percent of that group either have or are developing nonalcoholic steatohepatitis (NASH), characterized by inflammation and progressive scarring. NASH is already the second most common indication for liver transplantation and the fastest growing cause of hepatocellular carcinoma. Among the various histologic features of NASH, fibrosis driven by the activation of hepatic stellate cells into fibrogenic myofibroblasts is the strongest predictor of mortality, establishing it as a critical therapeutic target for the disease.
As part of its ongoing work with the autocrine pathway, the Mount Sinai team is actively exploiting this clinical opportunity. It has focused on the NTRK3-NTF3 protein interaction, one of the 68 hepatic stellate cell autocrine interactions researchers observed in both mouse and human NASH models.
“In these models, NTRK3 was not expressed in the healthy liver but was induced in hepatic stellate cells in NASH,” notes Dr. Wang, who was a postdoctoral fellow in Dr. Friedman’s lab for four years prior to recently starting her own lab, with the help of an R01 grant from the National Institutes of Health. “Working with an NTRK small-molecule inhibitor, LOXO-195, which is a next-generation, clinically tested, FDA-approved drug for treating tumors expressing NTRK fusion proteins, we successfully reversed the fibrosis. We also found that when we treated the human cells we had cultured with this inhibitor, it showed antifibrotic properties against those cells.”
That seminal work continues using different concentrations of the drug, and potentially other agents that are known to clinically inhibit NTRK3. At the same time, Dr. Friedman points to another exciting prospect for the investigation.
“It’s estimated that between 30 and 40 percent of all deaths in the industrialized world are related to scarring of different organs—the heart, lungs, kidney, liver, or bone marrow,” he says. “So, it’s possible that the drug we’re evaluating as a potential treatment for scarring of the liver could also end up being effective with other major organs. The potential of the work we’re doing is enormous, and can be seen as the legacy of what began more than 20 years ago when I came to Mount Sinai with a $1 million gift from a philanthropist to develop a pipeline for drug discovery in fibrosis.”