Private equity ownership of health care providers is a rapidly growing if poorly understood phenomenon in the United States, conjuring up a Pandora’s box of questions over the quality of care rendered by a sector committed to the bottom line.
Nowhere are the concerns greater than in the hospice industry, where private equity acquisition has been fierce, drawn to what investors perceive as a lucrative field with a steady revenue stream underwritten mostly by the Medicare hospice benefits program. Once the province of nonprofit organizations, as many as two-thirds of hospice programs are believed to be under for-profit control today.
“Widespread changes in organizational ownership are rapidly reconfiguring the landscape of hospice care delivery in the United States,” says Melissa Aldridge, PhD, MBA, Professor and Vice Chair of Research at the Brookdale Department of Geriatrics and Palliative Medicine at the Icahn School of Medicine at Mount Sinai, and lead author of a study in Health Affairs that defines the contours of private equity investment in hospice.
“Research examining this national trend has been extremely limited, however, due to the absence of transparent, validated data around private equity ownership in the hospice sector. Our study is helping to fill that gap by creating a novel database of private equity firms and hospice agencies involved in private equity transactions. This resource will help researchers to better understand and track the impact of for-profit and private equity ownership on the quality of and access to end-of-life care for older Americans.”
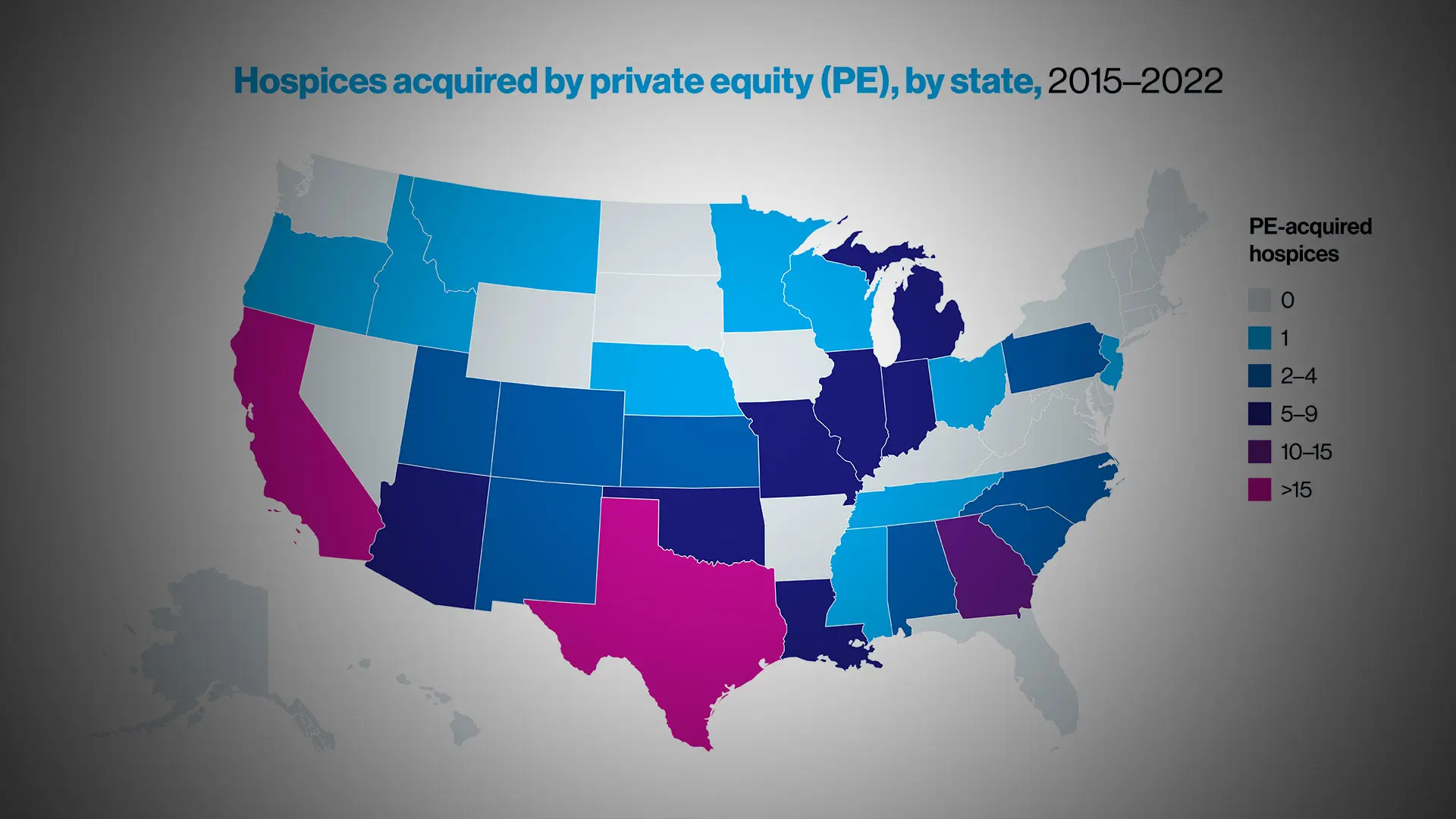
Hospices acquired by private equity (PE), by state, 2015-2022
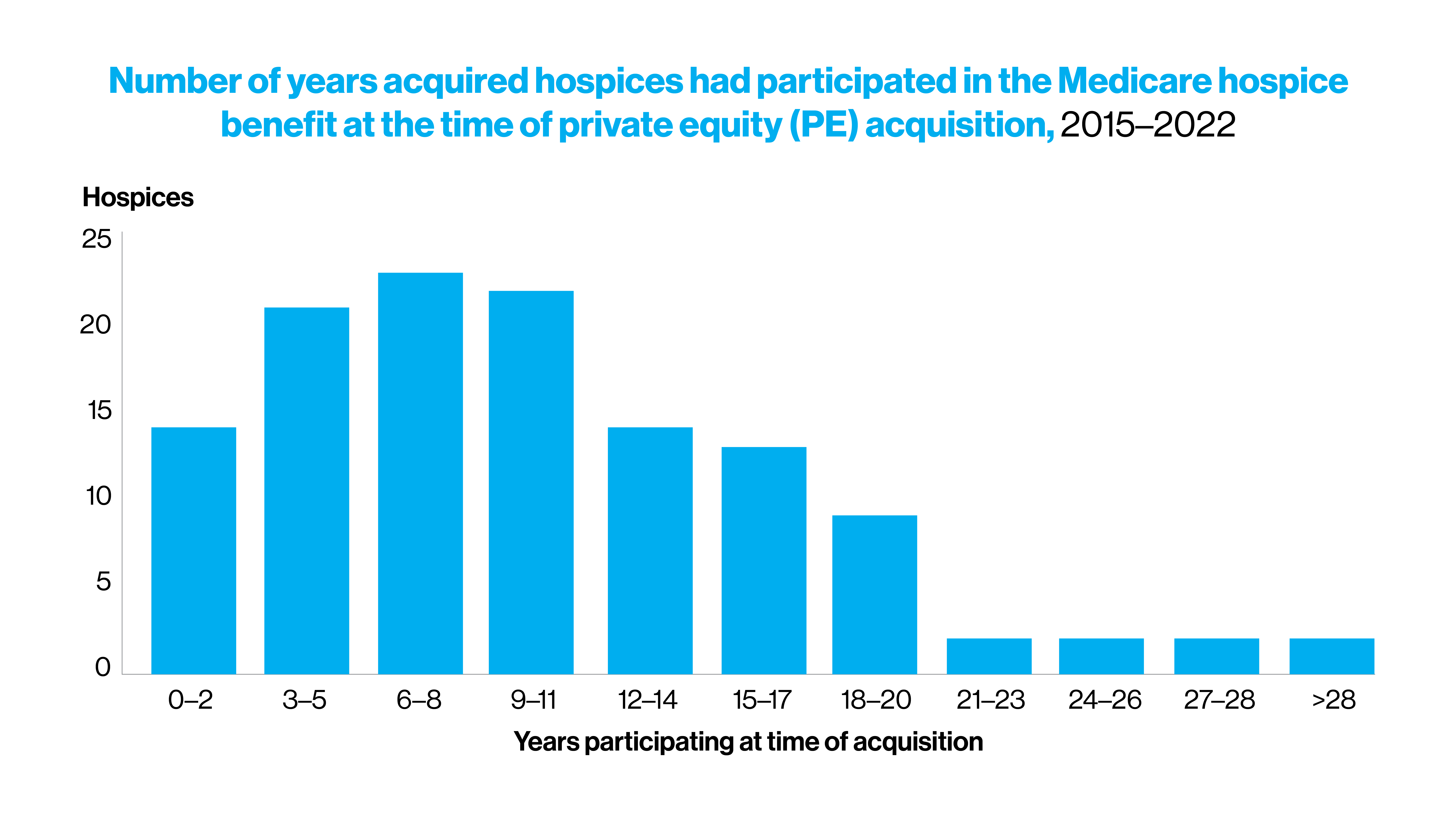
Number of years acquired hospices had participated in the Medicare hospice benefit at the time of private equity (PE) acquisition, 2015-2022
Concern over that issue has mounted as evidence has grown that hospice access and care quality differ significantly between nonprofit and for-profit entities, including private equity. One study found that 90 percent of hospices with the lowest spending on direct patient care (including home visits) and highest rates of hospital use were for-profit hospices. Moreover, there have been growing concerns about profiteering driving fraudulent behaviors among some hospices.
As described in the study, for-profit hospices provide a narrower range of services along with fewer community benefits, such as training, research and charity care. For-profits are also more likely than their nonprofit counterparts to care for patients with lower acuity over longer enrollment periods, to discharge patients prior to death, and to have higher rates of hospital and emergency use as well as complaints and deficiencies.
“In each of these cases, the drive to maximize profits offers a clear and cogent rationale for lower quality care,” says Dr. Aldrige. “The profit motivation is magnified in the case of private equity firms that enter the hospice space since they have a shorter time horizon—typically three-to-five years—to show a profit to their equity owners. This translates into disincentives to hire more staff or to put money into improving patient care and training.”

Melissa Aldridge, PhD, MBA, Professor of Geriatrics and Palliative Medicine and Vice Chair for Research
Integral to the team’s research was identifying a data source that could be used to gauge the breadth and depth of private equity penetration into hospice care. That source was the LevinPro proprietary database, commonly used in the investment banking industry, which captures details regarding all publicly reported private equity transactions where a majority stake in an organization is acquired.
The study found that from 2015 to 2022, there were 124 acquisitions of U.S. hospices by 47 private equity firms. While most firms acquired only one or two hospices, one investment company scooped up more than 22 hospices across 10 states and another 14 hospices spanning four states. This suggested to researchers that consolidation within the hospice industry was gathering considerable steam, with some private equity firms becoming potentially dominant players.
Another promising step toward publicly airing data around private equity ownership is the newly released Medicare Provider Enrollment, Chain, and Ownership System (PECOS), Medicare’s online enrollment management system. As the Mount Study elaborates, hospice providers are required to report a change in ownership or control to the Centers for Medicare & Medicaid Services (CMS) within 30 days, and this information is publicly posted on a quarterly basis.
The need for reliable information on changing ownership has never been greater than now because of its implications for not just hospices, but other vital parts of our healthcare system, according to Dr. Aldridge.
“Hospice acquisitions are not being done in isolation, but as part of a broader strategy to invest across multiple healthcare services, including skilled nursing homes, assisted living, and home health,” she says. “Tracking the complexities of this horizontal and vertical integration is important to understanding how it is influencing the quality of end-of-life care for both patients and their families.”