Mount Sinai was the first in the nation to offer a fellowship program in geriatrics. Nearly 40 years later, the Brookdale Department of Geriatrics and Palliative Medicine at the Icahn School of Medicine at Mount Sinai has the largest geriatrics and palliative medicine training program in the United States and has trained one in five such specialists across the country.
Dedicated to training top clinicians and leaders in the field, the goal of the Brookdale Department is to create a new generation of physicians, educators, researchers, policymakers, advocates, and innovators to address the critical workforce shortage in the field—a shortfall that is expected to grow in the coming years.
The LEAP into Geriatrics and Palliative Care Leadership Fellowship, launched in 2021, is an innovative two-year program that trains doctors to assume leadership positions and promote changes in health care that better meet the needs of older, frail, and seriously ill adults. The curriculum helps fellows “learn, explore, advocate, and promote” (LEAP) into geriatrics and palliative medicine leadership positions. The training emphasizes communication and leadership skills, health care policy and delivery knowledge, and programmatic development and management skills. Training includes a 10-session course administered through the Center to Advance Palliative Care (CAPC), where the emphasis is on health care finance and health system business topics—background that the fellows will need in future leadership roles.
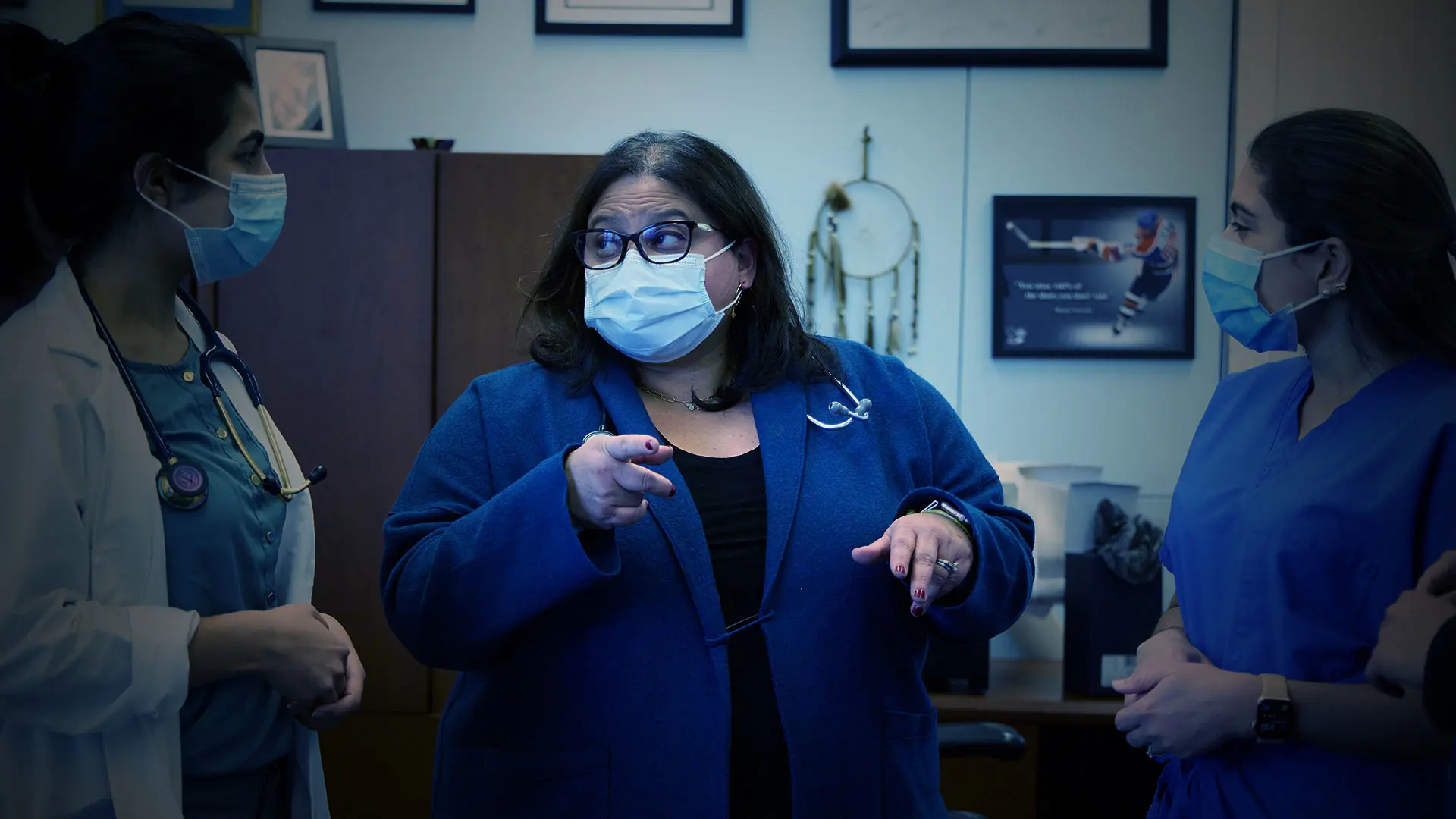
“The goal of the LEAP program is to give graduates the core set of skills to run hospitals, health systems, and quality-improvement programs, and to assume leadership positions within the Mount Sinai Health System,” says Helen M. Fernandez, MD, Vice Chair of Education and Professor of Geriatrics at Icahn Mount Sinai. “The intent is to disseminate this leadership training on a national platform that others can use and modify within their home institutions.”
“We need to push the envelope of training to meet the U.S. population needs," says Helen M. Fernandez, MD, Vice Chair of Education and Professor of Geriatrics at Icahn Mount Sinai.
The LEAP program is available at hospitals throughout the Mount Sinai Health System, including The Mount Sinai Hospital, Mount Sinai Beth Israel, Mount Sinai Morningside, and Mount Sinai West, and has been replicated in 10 hospitals around the country, including New York-Presbyterian/Weill Cornell Medical Center, UCLA Health, and Yale New Haven Health.
In addition to the LEAP program, Mount Sinai also offers a novel Mid-Career Hospice and Palliative Care Medical Fellowship for board certified physicians in internal, emergency, or family medicine who want additional training in palliative care to complement their skills in their original specialties. Mid-career fellows, those who are at least five years past completing their residency or last fellowship, spend approximately 20 percent of their time in training while simultaneously maintaining their existing clinical and professional roles and responsibilities. The program initially developed as a merged pilot with the University of Pennsylvania. Approved by the Accreditation Council for Graduate Medical Education (ACGME) as part of its Advancing Innovation in Residency Education program, this pilot has now expanded to five additional sites nationally.
This part-time, competency-based, time-variable fellowship program is considered a groundbreaking innovation in addressing the shortage of hospice and palliative medicine specialists.

Mollie Biewald, MD, Professor, Geriatrics and Palliative Medicine, and Associate Deputy Director of Palliative Medicine Fellowship Training
“We see mid-career physicians as an important untapped group of potential future specialists,” says Mollie Biewald, MD, Professor of Geriatrics and Palliative Medicine, and Associate Director of Palliative Medicine Fellowship Training. “We’re frequently contacted by practicing physicians across the country who are hospitalists or primary care doctors, or ICU or emergency medicine physicians, and they realize the importance of palliative care and want to get additional specialty training.”
Since the fellowship is part-time and competency-based (not time-based), the training schedule is flexible and allows physicians to gain hospice and palliative medicine training without giving up their ongoing professional responsibilities.
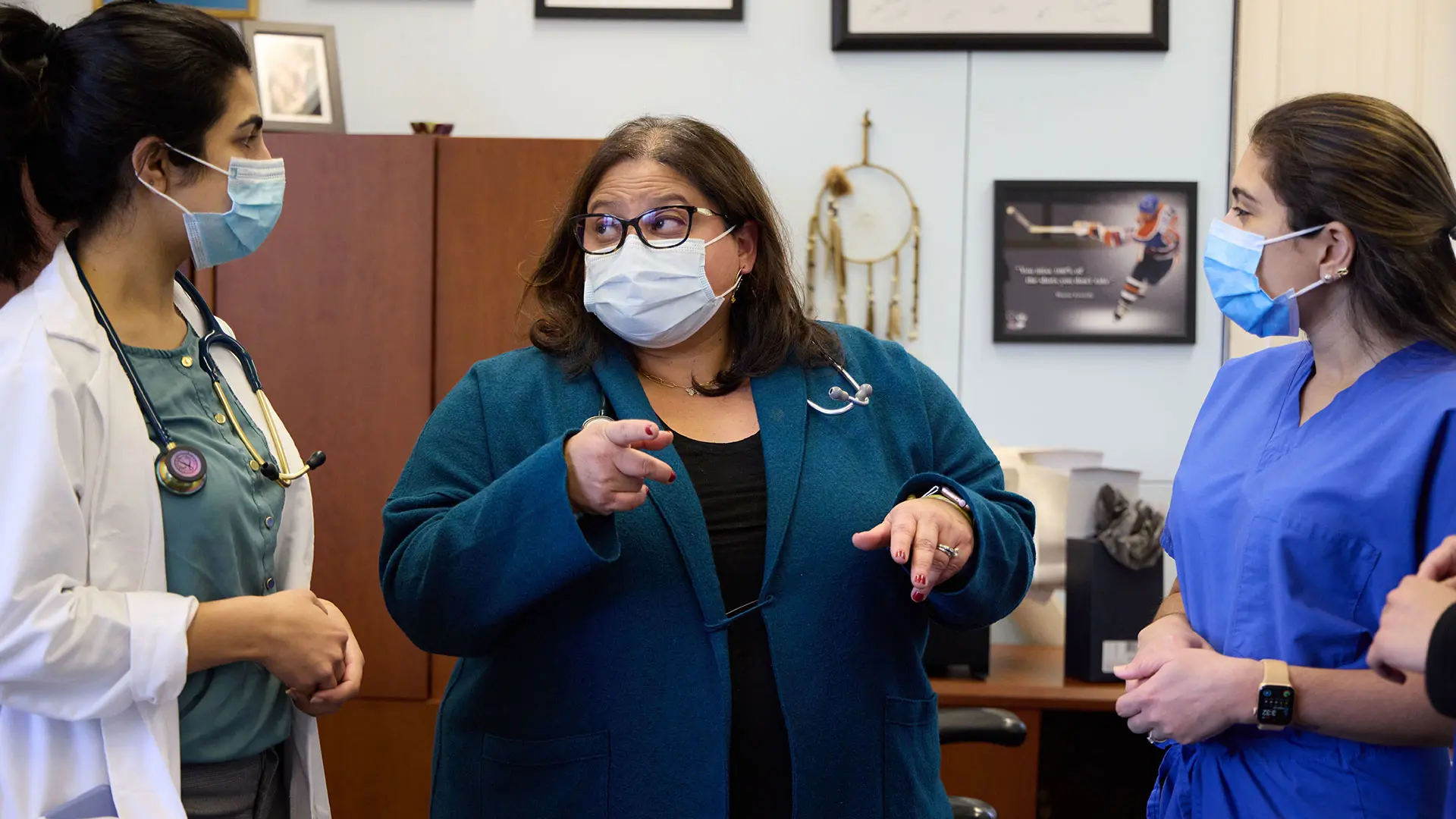
“We are essentially training these doctors while they continue to work in their regular practice, so they’re able to take the new skills they’re learning during their time with us, apply them in their attending practice, and develop themselves as dual-specialty leaders,” explains Vanessa Rodriguez, MD, Associate Director of Geriatrics Fellowship Training. To address a similar workforce shortage in Geriatric Medicine and need for flexible mid-career training models, Mount Sinai’s Geriatric Medicine Fellowship was recently approved by the ACGME to initiate a Mid-Career Fellowship as part of its Residency Education program.
Mount Sinai continues to lead the nation in offering geriatrics and palliative care training. Additional programs include the first-in-the-nation Integrated Geriatrics and Palliative Medicine Fellowship, which has been replicated at nine other institutions: Indiana University, New York University, New York-Presbyterian/Weill Cornell Medical Center, UCLA Health, University of California San Francisco, University of Chicago, University of Michigan, University of Pittsburgh, and Yale New Haven Health.
Ten years ago, Mount Sinai was among the first institutions to offer a Medicine-Geriatrics Residency fellowship, which trains an internal medicine or family medicine resident to become a geriatrician within four years. Today, the Brookdale Department also offers a one-year Geriatrics Fellowship, a one-year Hospice and Palliative Medicine Fellowship, a two-year LEAP Geriatrics Fellowship, a two-year LEAP Hospice and Palliative Medicine Fellowship, and a two-year Integrated Geriatrics and Palliative Medicine Fellowship. Currently, 32 physicians participate in the robust fellowship program.
“We need to push the envelope of training to meet the U.S. population needs. We have a radical belief that medicine should meet people where they are,” says Dr. Fernandez. “Our core values are recognizing that business as usual is not enough, so we challenge the status quo and develop and innovate new approaches to training and promote widespread adoption of these models.”

Vanessa Rodriguez, MD, Associate Director of Geriatrics Fellowship Training