Forty years ago, Robert Butler, MD, became the first chair of what is now known as the Brookdale Department of Geriatrics and Palliative Medicine at Mount Sinai. Having previously founded and chaired the National Institute on Aging, Dr. Butler quickly established a highly successful culture of research: identify and meet patients’ needs, specifically among underserved populations; create models of care that make a difference; and pursue policy-relevant work.
That culture subsequently flourished under Dr. Butler’s successors, Christine Cassel, MD, and Albert Siu, MD, and it continues to thrive under R. Sean Morrison, MD. “I want to see a health care system that ensures everybody has access to high-quality care,” says Dr. Morrison, the Ellen and Howard C. Katz Professor and Chair of the Brookdale Department at the Icahn School of Medicine at Mount Sinai, and Director of the National Palliative Care Research Center. “Our research is focused on achieving that.”
There are several major studies that Dr. Morrison cites as examples of the Brookdale Department’s ongoing commitment to advancing the quality of, and access to, care both at Mount Sinai and nationwide. One was a three-year undertaking to assess the benefits of a hospitalization-at-home care model bundled with a 30-day post-acute period of home-based transitional care among patients versus traditional inpatient care. Funded by a Health Care Innovation Award from the Center for Medicare and Medicaid Innovation and The John A. Hartford Foundation, the study included more than 500 participants with the broadest set of admitting diagnoses ever to be researched.
For the study, Mount Sinai’s research team created a hospitalization-at-home model of care to conduct the comparison and subsequently found that it achieved reductions in length of hospital stay, hospital readmissions, emergency department visits, and transfers to nursing facilities. The team also observed an improvement in patient experience among the at-home cohort versus the cohort that received traditional inpatient care. The results, published in the JAMA Internal Medicine in August 2018, made a compelling case for delivery of hospital-level care in the home.
“We showed that patients achieved better outcomes at home, experienced fewer hospital-acquired infections, and demonstrated a faster, better recovery,” says Dr. Siu, Professor and Chair Emeritus of the Brookdale Department and study lead. “That model of care has been disseminated across the country, with hospitals creating their own programs, and the Brookdale Department’s work served as a template for those efforts.”

Albert Siu, MD, Professor and Chair Emeritus of the Brookdale Department
The Brookdale Department also led a series of studies assessing the economic and patient benefits of palliative care programs, which provided a template for other medical centers to launch their own initiatives. One study found that earlier palliative care consultation during hospital admissions is associated with lower-cost hospital stays among patients with advanced cancer diagnoses. Intervention within two days was associated with a $2,280 reduction in hospital costs (24 percent) versus no intervention, and intervention within six days was associated with a $1,312 reduction (14 percent). The findings were published in the Journal of Clinical Oncology in June 2015.
“These studies led to significant growth in the number of hospitals nationwide with palliative care teams, rising from 5 percent to more than 75 percent, and 95 percent of hospital systems such as Mount Sinai that provide tertiary or quaternary care have palliative care programs,” says Dr. Morrison, who was the study’s lead author. “That was the result of studies we conducted that focused on the effectiveness of this model of care delivery for people with serious illness.”
Another important study assessed the financial challenges that families and patients with dementia face during the last five years of the patients’ lives compared to patients who do not have dementia. Supported by the National Institute on Aging, the data were supplied by the Health and Retirement Study, a national sample of U.S. adults ages 70 and older linked to Medicare claims. Amy S. Kelley, MD, MSHS, was the study’s lead author. She is now the Deputy Director of the National Institute on Aging.
The study found that out-of-pocket spending for patients with dementia was 81 percent higher than for those who died from other causes. The burden of this spending, measured as the proportion of household wealth devoted to out-of-pocket costs, was particularly high for dementia patients who were Black, had less than a high school education, or were unmarried or widowed women. The results were published in Annals of Internal Medicine in November 2015.
“Our findings highlighted the importance of creating care delivery models that meet people where they are,” Dr. Morrison says. “High-quality care in the setting of a serious illness should not be predicated on whether a patient is dying.”

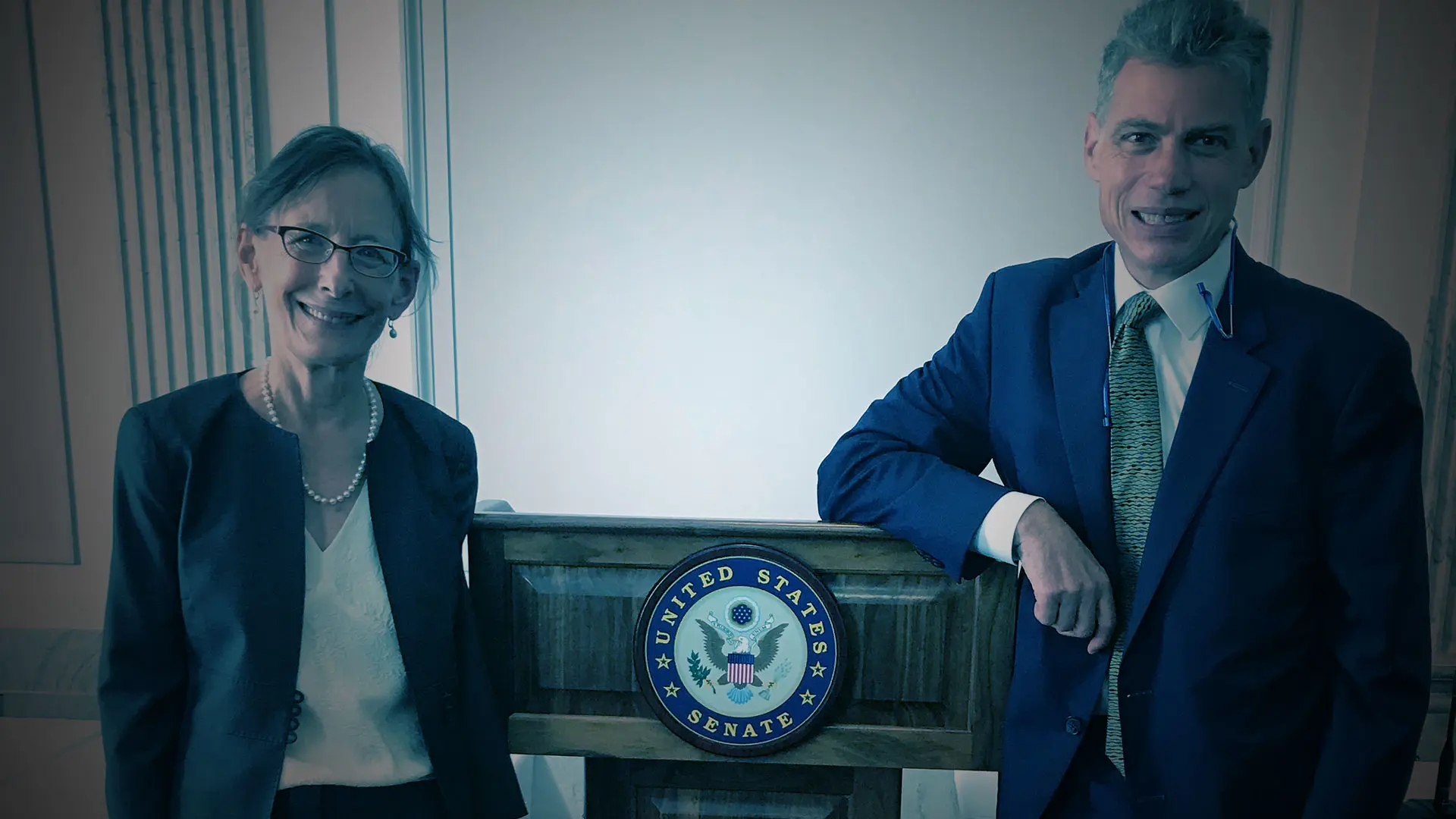
Diane Meier, MD, Director of the Center to Advance Palliative Care, and R. Sean Morrison, MD, the Ellen and Howard C. Katz Professor and Chair of the Brookdale Department of Geriatrics and Palliative Medicine, helped to educate legislators in Washington on research and changing health policy.
One other study that comes to mind as Dr. Morrison reflects on the Brookdale Department’s 40-year legacy of impactful research: is an undertaking led by Dr. Siu that significantly changed the process of care related to hip fractures among older patients. Published by the Journal of the American Medical Association in 2012, the study recommended a multidisciplinary co-management approach that extended beyond orthopedic repair to enhance patient recovery and outcomes. Recommended care elements included perioperative correction of abnormalities and administration of antibiotics; tailored rehabilitation strategies for patients; and postoperative pain management.
“Prior to that study, there was considerable resistance to administering opioids or analgesics for people with fractures,” Dr. Morrison says. “The thinking was that the patients would become delirious or that it would impair recovery. What we found was that untreated pain increased the risk of delirium dramatically, because pain was a bigger risk factor than the side effects of the opioids. That study changed how we regard one of the most morbid diseases among older adults.”
Another key achievement of the Brookdale Department’s research efforts has been the development of the Population-Based Research in Geriatric Palliative Care Program. It brings together the national population-based survey data from ongoing longitudinal studies, including the Health and Retirement Study; the National Health and Aging Trends Study; the Medicare Current Beneficiary Study; the data management and analytic teams; and department investigators to obtain funding to conduct needed research.
As a result, Department investigators are at the forefront of the national surge in palliative care research across a wide range of geriatric palliative care issues related to health policy; financing systems; organizational structures and processes; costs of care; intensity of care; caregiver outcomes; and patterns and disparities in health care for older adults with serious illness. The program has also been instrumental in attracting new investigators interested in health services research careers in geriatric palliative care.
“Geriatric palliative care research requires a broad perspective incorporating patient and family clinical, social, and economic characteristics known to influence health, health care decision-making, and overall quality of life,” says Melissa Aldridge, PhD, MBA, Professor of Geriatrics and Palliative Medicine, and Vice Chair for Research at the Brookdale Department.
“Single site and even small multisite studies are often unable to enroll a large enough sample to study individuals with a wide range of diagnoses, comorbid conditions, and functional limitations, or to collect information on social determinants of health or caregiver characteristics and outcomes,” she adds. “Over the past 10 years, we have built a program to employ existing population-based studies to conduct this type of needed research and, in doing so, have sparked innovative approaches to improving care for an aging population.”
“Geriatric palliative care research requires a broad perspective incorporating patient and family clinical, social, and economic characteristics known to influence health, health care decision-making, and overall quality of life.”
- Melissa Aldridge, PhD, MBA, Vice Chair, Research
The Brookdale Department is continuing to pursue research that has the potential to change approaches to care delivery, create new templates for other centers to adopt, and address accessibility gaps. For example, Dr. Siu is exploring the link between hospital practices and the patient populations they serve, and several faculty members are exploring pain treatment and disparities in access to related therapeutics among different racial, ethnic, and socioeconomic groups.
“Addressing and resolving inequities is our priority going forward,” Dr. Morrison says. “I am not naïve to think we can achieve this for the entire country. But we can make a dent for people who are living with serious illness and for older adults, and we can develop models that others can adopt to achieve that goal.”