In 1982, Mount Sinai was the first hospital in the United States to establish a department of geriatrics. Under the leadership of Robert N. Butler, MD, considered the father of modern geriatrics, the Department of Geriatrics and Adult Development, as it was then called, transformed the field for clinical care for older adults, and medical training for the doctors who treat them. A strong advocate for policies that improve health care for older adults and one of the first geriatricians to recognize the importance of palliative care, Dr. Butler laid the foundation for what would become the Brookdale Department of Geriatrics and Palliative Medicine at the Icahn School of Medicine at Mount Sinai, one of the most advanced geriatrics departments in the world.
“So much of what this Department has accomplished over the past 40 years traces right back to Dr. Butler’s vision and to the work of his successors,” says R. Sean Morrison, MD, Ellen and Howard C. Katz Chair of the Brookdale Department. “First and foremost, he created a workforce that has the specific knowledge and skills to both care for older adults and to develop programs across the country.”
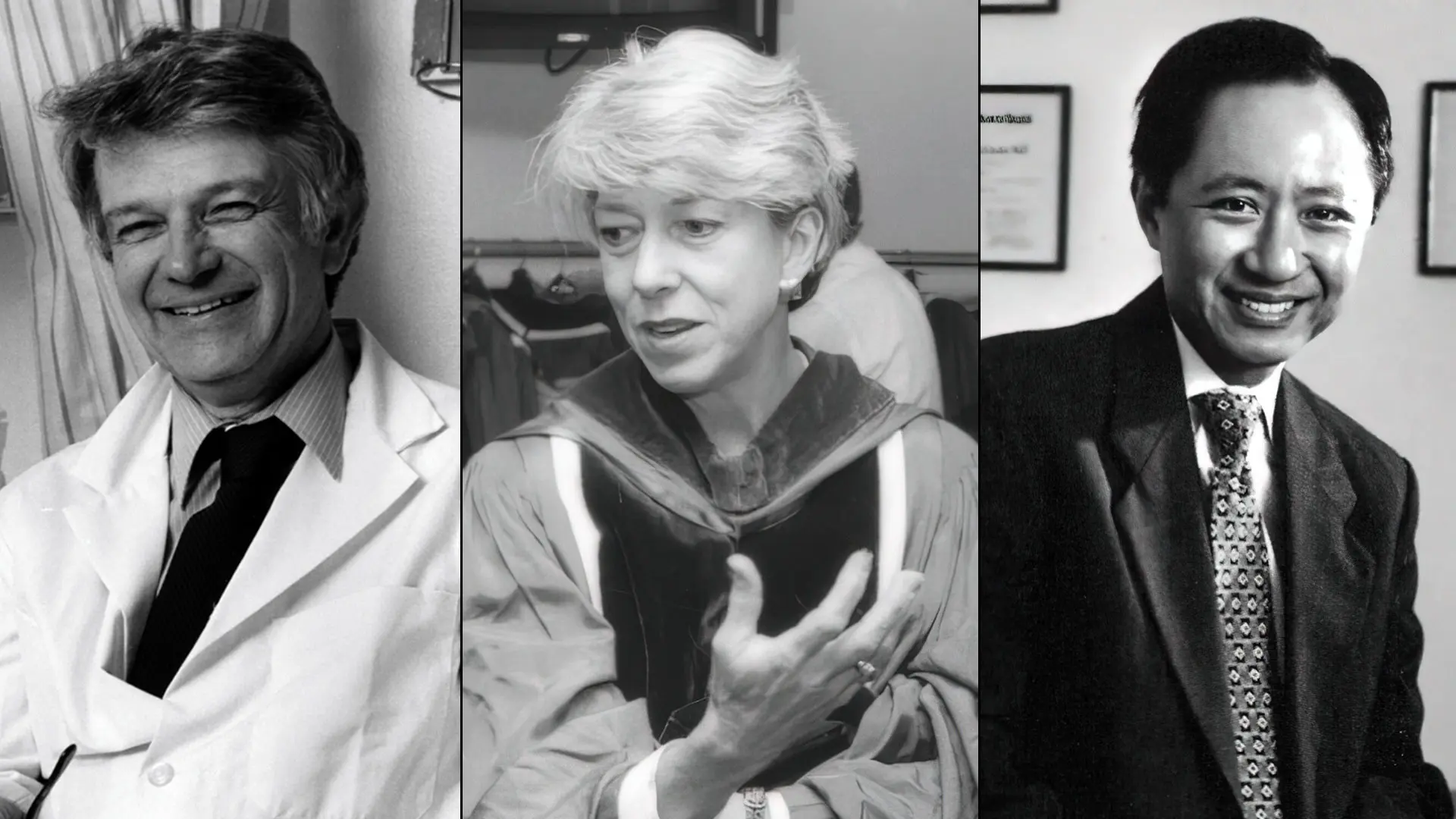
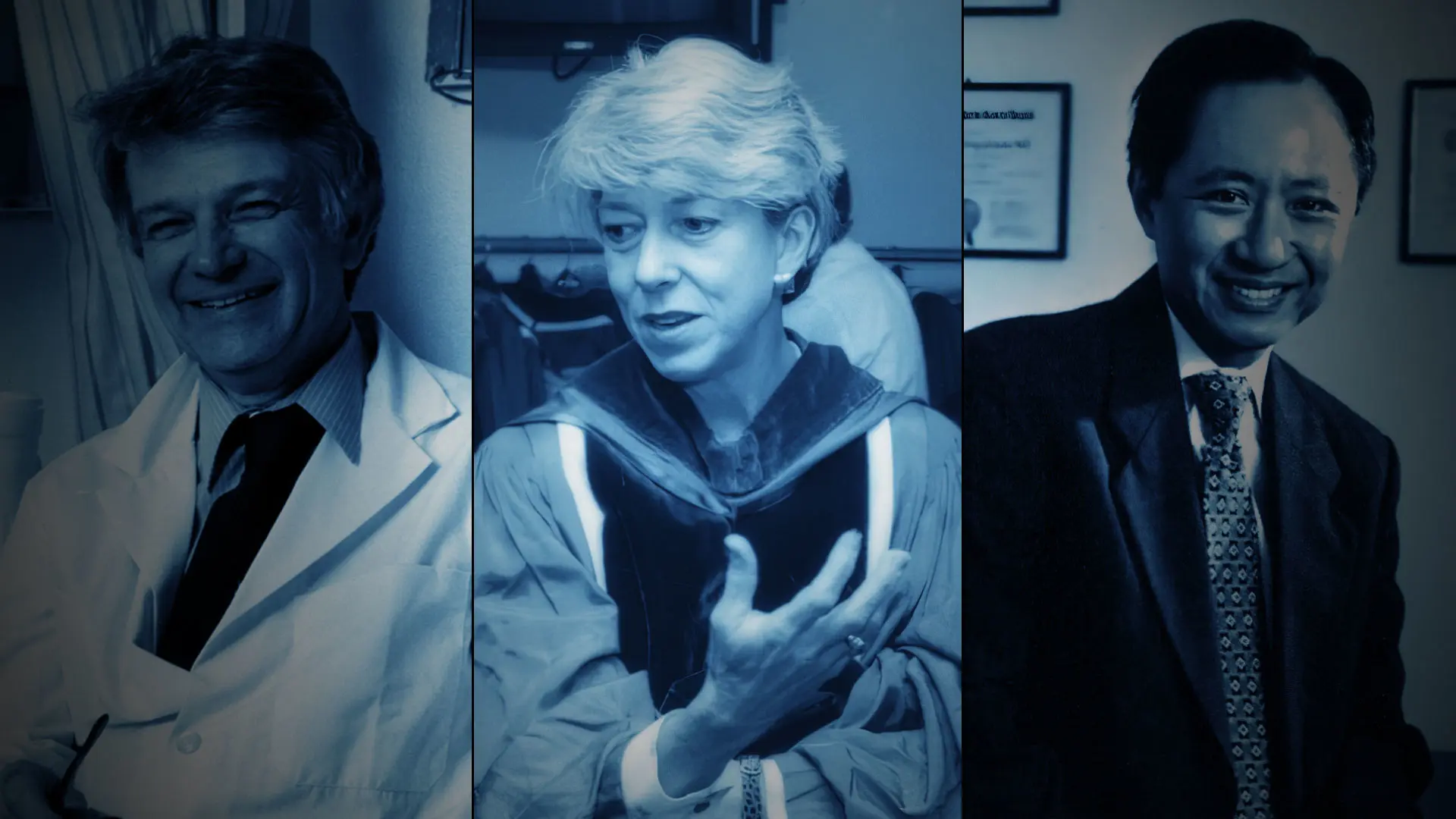
Much of the accomplishments of the Brookdale Department of Geriatrics and Palliative Medicine over the past 40 years trace back to Robert N. Butler, MD, left, who laid the foundation for what would become the Department, and his successors, Christine K. Cassel, MD, and Albert L. Siu, MD.
In the past 40 years, Mount Sinai has trained one in five geriatricians in the United States. With its focus on leadership, in addition to clinical skills, Mount Sinai has trained many of the nation’s leading geriatricians, including Amy S. Kelley, MD, recently named Deputy Director for the National Institute on Aging, part of the National Institutes of Health (NIH). Brookdale-trained geriatricians hold key leadership positions throughout the Mount Sinai Health System, including Jeremy Boal, MD, President, Mount Sinai Beth Israel and Mount Sinai Downtown; Cameron R. Hernandez, MD, Executive Director and Chief Operating Officer of Mount Sinai Queens; Reena Karani, MD, Director of the Institute for Medical Education; and Rainier P. Soriano, MD, Senior Associate Dean for Curricular Affairs.
Mount Sinai has one of the most diverse teaching staffs and is approaching its goal of a faculty that reflects the population for which it cares. Icahn Mount Sinai’s transformative approach to education has changed the way doctors are trained in the fields of geriatrics and palliative medicine, not just for specialists in that field, but for all physicians, by inserting palliative care and geriatrics specialists into the genome of American medicine.
In the past five years, the Brookdale Department has expanded its renowned fellowship program, which remains the largest in the nation, and created four new training programs, bringing the total number of fellows to 32. The Mount Sinai fellowship training programs have been replicated in 13 teaching centers nationwide.
In the area of clinical care, Dr. Morrison credits the Brookdale Department with creating the business case for palliative care that ensured its exponential growth. “Mount Sinai has the largest suite of geriatrics and palliative care services in the country,” he says. “We created many of the clinical models that are now routine throughout the United States—programs that meet patients where they are, rather than making patients come to us.”
Innovations have included the launch of telehealth and e-consult programs that enable patients to get medical attention without having to travel to a clinic or doctor’s office; the Mount Sinai Visiting Doctors Program, one of the largest home-visit programs in the nation; and Palliative Care at Home and Hospitalization at Home, which provide acute and hospital-level in-home care from a team of doctors, nurse practitioners, nurses, social workers, and other professionals. There has also been an emphasis on creating programs that treat older adults in community settings, including clinics, nursing homes, and Veterans Administration hospitals.
When a hospital stay is required, instead of treating geriatrics patients in a separate unit, Mount Sinai has shifted its approach to sending an interdisciplinary geriatrics team to patients, whether it’s in the intensive care unit, a surgical floor, or elsewhere in the hospital. Meanwhile, inpatient geriatrics consults have increased by 25 percent across most Mount Sinai sites due to the close collaboration and trusted relationships that have developed throughout the Health System.

“Clinicians from anywhere in America—in rural areas, small towns, or big cities; local hospitals or large health systems—will now have unprecedented access to Brookdale Department experts and the country’s very best geriatric leadership training,” says R. Sean Morrison, MD, Ellen and Howard C. Katz Chair of the Brookdale Department.
Today, geriatrics and palliative medicine services are offered across five Mount Sinai hospital campuses: The Mount Sinai Hospital, Mount Sinai Beth Israel, Mount Sinai Morningside, Mount Sinai West, and Mount Sinai Queens. Additionally, inpatient palliative care and outpatient geriatrics are offered at the James J. Peters VA Medical Center, which is affiliated with Mount Sinai.
Mount Sinai is also recognized for its groundbreaking research focused on the most vulnerable patient populations and helping to create a new generation of scientists focused on enhancing care for those living with serious illness. Since 2007, the Brookdale Department has served as the home for the National Palliative Care Research Center—a philanthropically supported national research center that has supported more than 140 investigators throughout the United States and stimulated more than $200 million in NIH research. Over the past five years, the Department has doubled its research funding from the NIH, doubled its number of NIH-funded investigators, and doubled the number of publications produced by its investigators each year.
“We’ve been able to put a spotlight on those who the health care system is really not caring for very well,” says Dr. Morrison. “A lot of the research that we're doing looks at how we can better support the needs of patients, and the family and paid caregivers who are caring for them.”
According to the U.S. Census Bureau, by 2030, baby boomers will be older than age 65, one in every five Americans will be of retirement age and, for the first time in U.S. history, adults over 65 will outnumber children.
“We need to redesign our health care system so it focuses on the needs of older adults, rather than on the needs of middle-aged adults, which is where it’s focused now,” says Dr. Morrison. “As we look to the future, our goal is to continue to grow the Department and to ensure that we are providing the highest quality of care for the people in our community, even as we serve as a national model for others.”