Telemedicine use among adults in the United States has seen widespread adoption since the beginning of the pandemic, providing a safe alternative for patient visits while ensuring continuity of care.
“There was a five-fold increase in the number of older adults who used telemedicine at the beginning of the pandemic,” says Julia L. Frydman, MD, Assistant Professor, Brookdale Department of Geriatrics and Palliative Medicine, who has studied this issue. “We need to make sure we keep that progress going and expand access to the rest of the population of older adults.”
Julia L. Frydman, MD, Assistant Professor, Brookdale Department of Geriatrics and Palliative Medicine
Thanks to a decision by the Centers for Medicare and Medicaid (CMS) in November 2021, a new rule will extend Medicare reimbursement for telemedicine for an additional two years. In its announcement, CMS suggests that telemedicine may be here to stay—stating that a two-year extension through the end of 2023 will allow additional time to evaluate whether the services should be permanently added to the Medicare telehealth services list.
In a study published in the Annals of Internal Medicine in November 2021, Dr. Frydman and researchers at Mount Sinai tapped the National Health and Aging Trends Study (NHATS), which surveys Medicare enrollees, to understand the predictors and prevalence of telemedicine use among older adults.
The study found that of 2,350 respondents, 23.9 percent reported telemedicine use during the pandemic, up from 5.94 percent before the pandemic, while 59.9 percent reported in person-visits.
“Telemedicine really took off during the pandemic. Yet, the vast majority of Medicare enrollees did not avail themselves of this safer option to see their providers,” says Dr. Frydman. “More than half went to see their health care provider in person, despite the risks associated with travel to clinics and hospitals, many of which were overwhelmed with sick patients.”
23.9%
Respondents who reported telemedicine use during the pandemic
5.94%
Respondents using telemedicine before the pandemic
Dr. Frydman’s study underlines critical barriers and disparities. For example, older adults with lower education, without a partner or spouse, or living in rural communities, were among those who did not use telemedicine.
“As telemedicine use expands, we need to ensure we address barriers in access to telemedicine so as to reduce health care disparities rather than exacerbate them,” says Dr. Frydman.
In a separate study published in the Journal of Pain and Symptom Management in October 2021, Dr. Frydman and researchers at Mount Sinai examined the factors associated with telemedicine use in patients with cancer in the ambulatory palliative care setting. This work was an important inquiry for the researchers in light of the shortage of specialty palliative care clinicians.
“We wanted to know if the availability of telemedicine would move the needle,” says Dr. Frydman.
After analyzing nearly 500 patient visits, where the opportunity for telemedicine was presented to patients, they found that those less likely to use telemedicine were male, Spanish-speaking, uninsured, or without an activated patient portal.
“The difference between getting palliative care and not getting it when you are a cancer patient is huge,” says Dr. Frydman. “These results suggest we need to do more to bridge health disparities so that everyone has access. Equity must be at the forefront as we assess the true, long-lasting value of telemedicine.”
Overall, there has been a significant expansion of telemedicine use, and clinicians now need to focus on continuing to meet patients’ needs, according to Dr. Frydman.
“It’s now our job to understand the ongoing barriers to telemedicine access, including the digital divide and the usability of telemedicine platforms, and design interventions that overcome them,” she says. “At the same time, we need to make sure we are understanding and respecting the preferences of older adults in terms of how they access health care.”
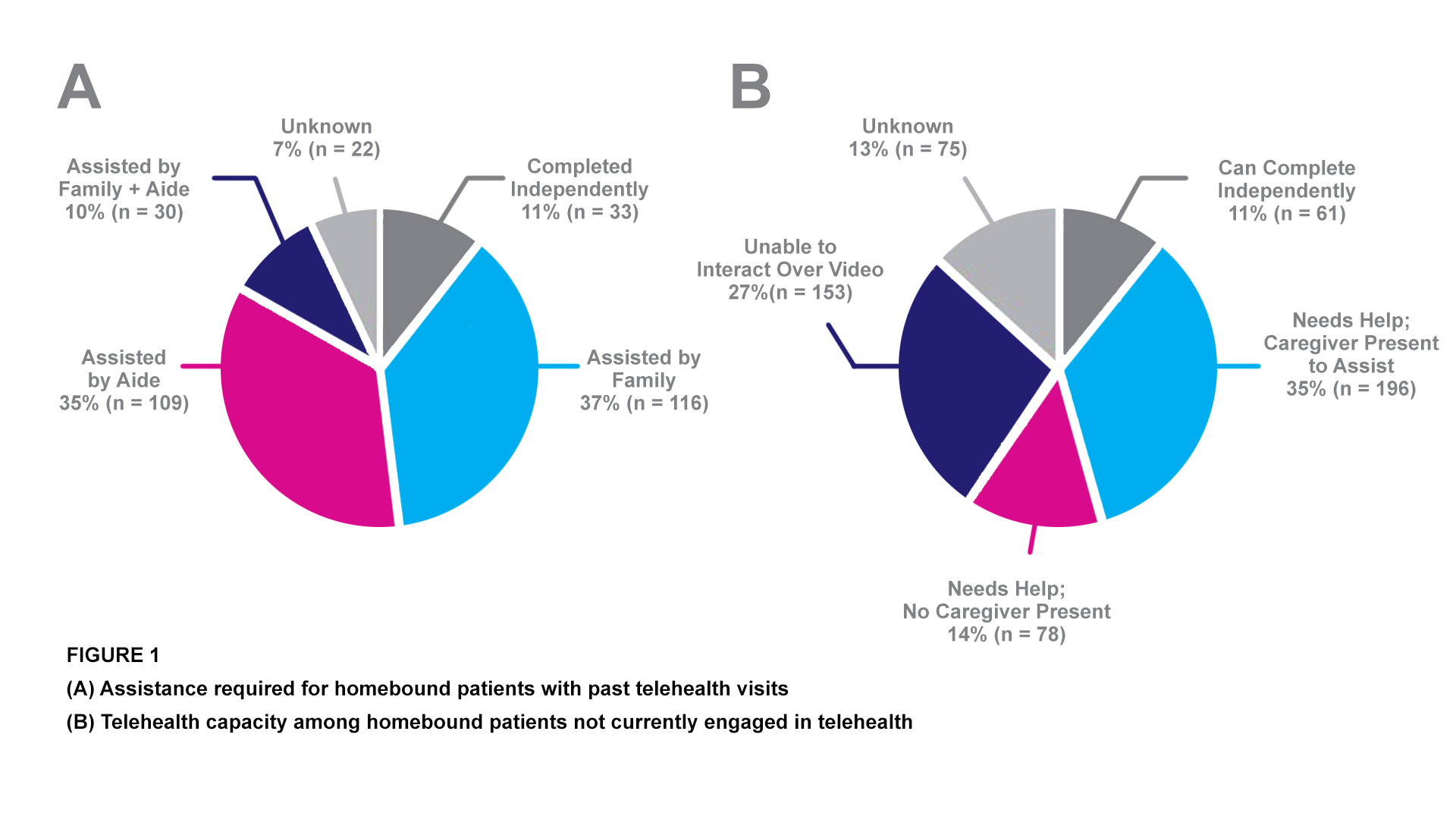
This chart shows some of the barriers to telehealth access among homebound older adults, part of research by Alexander V. Kalicki, BS, Kate A. Moody, BS, Emily Franzosa, DrPH, Peter M. Gliatto, MD, and Katherine A. Ornstein, PhD, MPH.
Source: Journal of the American Geriatrics Society, April 2021
