Research at the Brookdale Department of Geriatrics and Palliative Medicine has reached a new threshold with its key components—funding, infrastructure, data sets, and experienced investigators—firmly in place.
The Brookdale Department continues to build off the strong performance of 2020, when 35 National Institutes of Health (NIH) grants and four foundation grants helped attract $5.5 million in new funding for studies focused on evaluating and improving treatment and care of older adults in the United States.
35 NIH grants and 4 foundation grants attract $5.5 million in funding
The following two studies help illustrate the significant strides our researchers are making:
Preparing Hospice Care for the Next Emergency
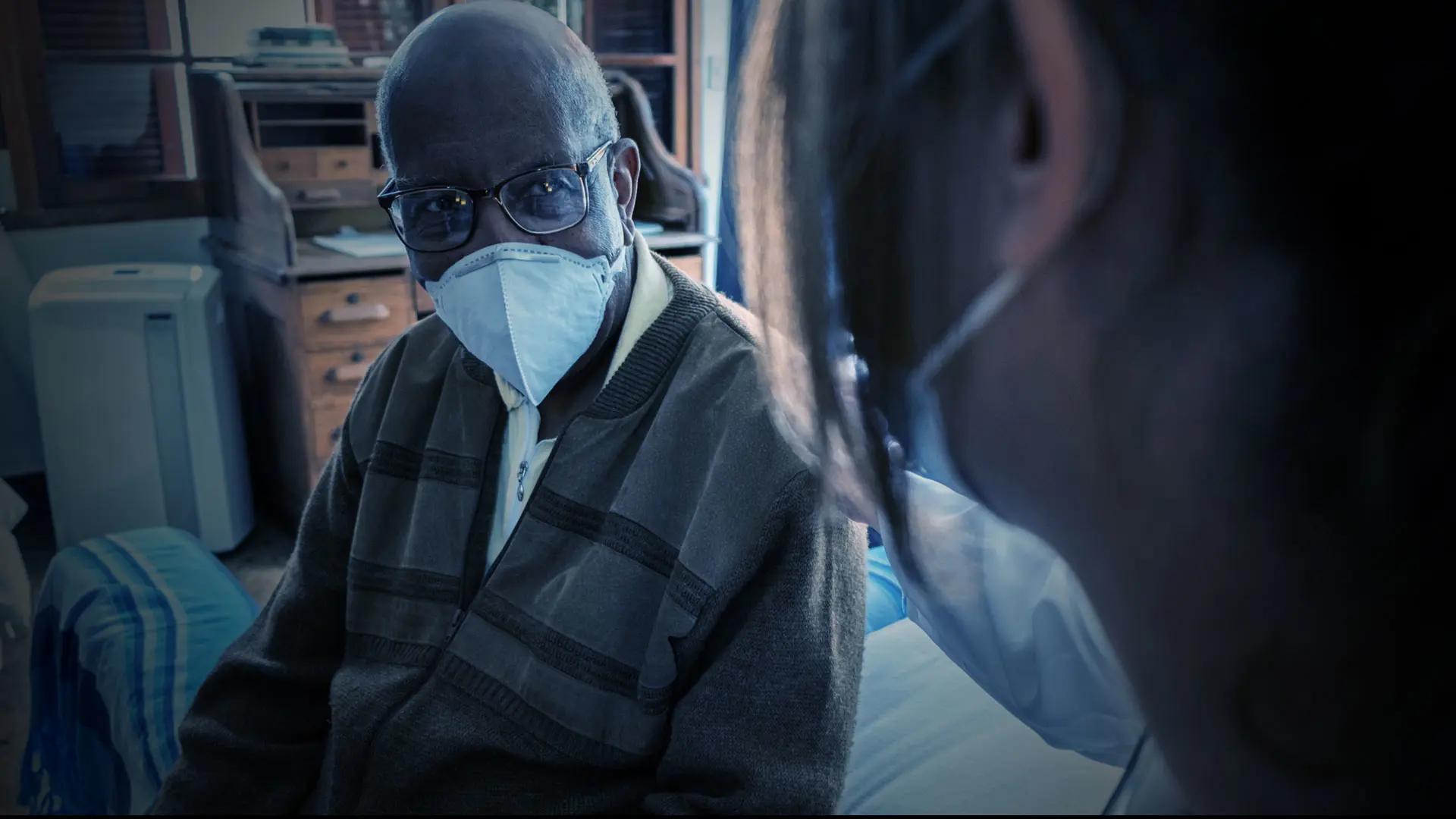
Hospice care has played a critical role in supporting seriously ill patients in their homes during the ongoing COVID-19 pandemic, yet there have been few assessments of hospice practices, and a paucity of guidance, that could help hospice organizations across the country improve their preparedness. Indeed, New York City experienced a shortage of hospice services at the height of the pandemic in early 2020, exposing vulnerabilities and raising questions about the system’s ability to respond to a future health crisis.
Against that backdrop, the Brookdale Department launched an in-depth study to understand the challenges of delivering end-of-life care in New York City during the pandemic. Backed by a $1.7 million grant from the National Institute of Nursing Research (NINR), the Brookdale Department is investigating the barriers to hospice care access, as well as the difficulties in care coordination experienced by patients and their families during the pandemic. The work will include a national survey of hospice agencies to determine what they learned, and how that knowledge has impacted policies and practices.
“This project is unique in its rapid, mixed methodologies approach to studying the care available to a large and highly vulnerable population during the COVID-19 pandemic,” says Principal Investigator Melissa Aldridge, PhD, MBA, Professor of Geriatrics and Palliative Medicine and Vice Chair for Research at the Brookdale Department of Geriatrics and Palliative Medicine.
The study builds off of work led by Katherine Ornstein, PhD, MPH, Associate Professor, Geriatrics and Palliative Medicine, and Director of Research for the Institute of Care Innovations at Home at Mount Sinai, examining the experience of individuals who died at home during the first wave of COVID-19 in New York City and demonstrates the collaborative nature of the Brookdale Department’s research teams.
“We believe our work will help to inform current and future planning and policy, and contribute new insights into how hospices can improve end-of-life care for patients and families during a public health emergency,” says Dr. Aldridge.
The Effects of Comorbid Dementia on Hospice Care
Our understanding of hospice use among people with dementia is based almost exclusively on those with a primary diagnosis of terminal dementia, leaving a significant gap in our understanding of how comorbid dementia affects hospice use patterns.
Researchers from the Brookdale Department tackled that important question by studying more than 3,100 Medicare beneficiaries who were enrolled in U.S. hospice programs and died between 2004 and 2016.
They found that approximately 15 percent had a primary hospice diagnosis of dementia, while an additional 30 percent had comorbid dementia and died of another illness. Those with comorbid dementia were at increased risk for long hospice enrollment periods and disenrollment following six months of hospice care. The authors concluded that “consideration of the high prevalence of comorbid dementia should be inherent in hospice staff training, quality metrics, and Medicare hospice benefit policies.”
The study, which was published in October 2021 in the Journal of Palliative Medicine, is part of the Brookdale Department’s recent research focus in dementia care following a large National Institute on Aging program grant obtained in 2020.
Dr. Aldridge was the lead author for the study along with senior author Amy Kelley, MD, MSHS, Senior Associate Dean for Gender Equity in Research Affairs and Hermann Merkin Professor in Palliative Care, Brookdale Department of Geriatrics and Palliative Medicine; and co-authors Lihua Li, PhD, Assistant Professor, Geriatrics and Palliative Medicine, Population Health Science and Policy; Mohammed Husain, MA; and Lauren Hunt, PhD, University of California, San Francisco.
Featured

Melissa Aldridge, PhD, MBA
Professor of Geriatrics and Palliative Medicine and Vice Chair for Research at the Brookdale Department of Geriatrics and Palliative Medicine