Related Article
Two new grants from Pfizer will help the Mount Sinai NASH Center of Excellence deliver on its dual mission: to provide exemplary care to all patients with nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH), and to increase scientific knowledge about the causes of these conditions. The grants will enable the Center to educate primary care providers on how to identify at-risk patients and address inequities in diagnosis and care.
A $250,000 educational grant awarded to the Center’s Director, Meena Bansal, MD, will support efforts to raise awareness about electronic health record system tools such as FIB-4, a noninvasive test that estimates a patient's degree of liver fibrosis and is integrated into Mount Sinai’s Epic system. These tools can assist primary care and other front-line providers in screening patients who are at risk of developing NASH with significant fibrosis and in making appropriate referrals for evaluation and treatment based on the American Gastroenterological Association’s Clinical Care Pathway.
Dr. Bansal says providers will receive customized reports that demonstrate both the value of screening patients for advanced fibrosis and the impact of adhering to the established care pathway, such as referring patients with intermediate NAFLD fibrosis scores for a FibroScan®.
“Primary care providers are the first line of defense, and they need to have appropriate tools to identify patients who should undergo further evaluation,” says Dr. Bansal, Professor of Medicine (Liver Diseases) at the Icahn School of Medicine at Mount Sinai. “By introducing them to these tools, showing them how they work, and then providing feedback on the impact of using the care pathway, we believe we can promote continuous learning and quality development among primary care providers. Equally important, we believe our efforts will lead to increased screening and identification of at-risk patients.”

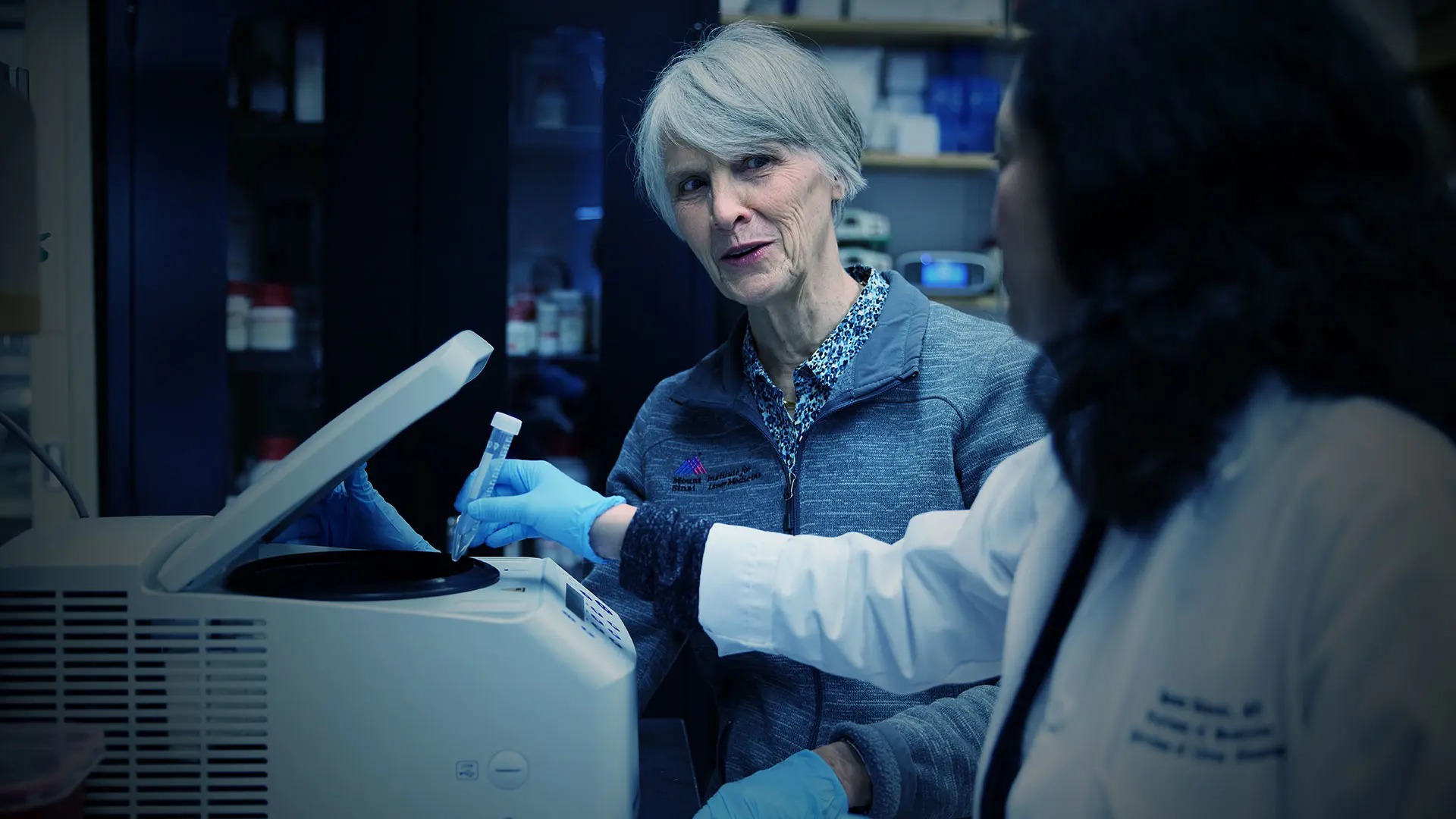
Meena Bansal, MD, is working to encourage primary care providers to screen their patients for liver diseases like NAFLD and NASH.
A second Pfizer grant, valued at $140,000, is enabling Andrea D. Branch, PhD, and her colleagues to use the National Health and Nutrition Examination Survey datasets to identify NAFLD and fibrosis risk factors that differ among non-Hispanic Black, Mexican American, and non-Hispanic white populations. The goal is to build a more comprehensive understanding of the unique risk factors among these populations.
For example, in previous studies supported by the Centers for Disease Control and Prevention and the National Institute for Occupational Safety and Health, Dr. Branch found that advanced liver scarring among non-Hispanic Black populations is not only associated with cadmium exposure—which is associated with scarring in all populations—but also with lead exposure and poverty. These findings suggest that toxic and environmental exposures play a larger role in liver scarring among non-Hispanic Black than among non-Hispanic white populations.
“We have assumptions about disease presentation and risk factors that are not appropriate for all demographic groups and that can result in care policies that are not equitable,” says Dr. Branch, Professor of Medicine (Liver Diseases) at Icahn Mount Sinai. “I want to ensure that policies are equitable. My hope is that, through this grant, we will identify distinct factors that enable us to catch disease at an earlier stage among these populations. We plan to use these findings to develop an algorithm that will flag people at risk in our electronic health record system, enabling their early diagnosis and linkage to care.”
These grants complement several undertakings launched by the Center since its formation in January 2022 that seek to better understand disease drivers and thus achieve improved patient prognosis and treatment. Among the most notable is a longitudinal registry that will enroll 5,000 Mount Sinai patients across the whole spectrum of the disease—and Mount Sinai’s diverse patient population—to explore why inflammation and fibrosis are stimulated in some individuals but not others. The goal, given the heterogeneity of NASH, Dr. Bansal says, is to develop a rigorous algorithm that enables phenotyping and risk stratification of patients for likelihood of rapid fibrosis progression based on biological and social factors. This will facilitate earlier interventions that can be tailored to the drivers of disease in individual patients.
“We want to be the leader in NASH in all aspects from basic science to clinical,” Dr. Bansal says. “Through our combined expertise, work, and our diverse patient population, I think we are uniquely positioned to make valuable contributions to understanding and treating this disease.”
Featured Faculty and Division Leadership

Meena Bansal, MD
Professor of Medicine (Liver Diseases); System Chief, Division of Liver Diseases

Andrea D. Branch, PhD
Professor of Medicine (Liver Diseases)