Already one of the top three centers in the world for proctocolectomy with ileal pouch-anal anastomosis (IPAA), commonly known as J-pouch surgery, Mount Sinai is helping patients—especially women—navigate the often-rough postoperative waters through a Comprehensive Pouch Program within the Susan and Leonard Feinstein Inflammatory Bowel Disease (IBD) Clinical Center.
As Marla Dubinsky, MD, Professor of Pediatrics (Gastroenterology), and Medicine (Gastroenterology), and Co-Director of the Feinstein IBD Center, puts it, “We now have a program that integrates the surgical, medical, and research sides of J-pouch surgery to ensure the best possible outcomes for patients undergoing a life-altering procedure.”
J-pouch surgery is steeped in history at Mount Sinai. The program began in 1978 and its internationally recognized colorectal surgeons have since helped to pioneer a three-stage, minimally invasive approach to proctocolectomy for patients with treatment-resistant ulcerative colitis (UC). These surgeons—who currently include Alexander Greenstein, MD, Associate Professor of Surgery at the Icahn School of Medicine at Mount Sinai; Sergey Khaitov, MD, Assistant Professor of Surgery; Sue Hahn, MD, Assistant Professor of Surgery; and Patricia Sylla, MD, Associate Professor of Surgery—collectively perform about 75 proctocolectomies a year, while other institutions typically average 5 to 10.
Mount Sinai’s newest J-pouch initiative is the creation of a Comprehensive Pouch Program to closely monitor patients after surgery, ensuring continuous, hands-on care designed to prevent postoperative problems. “With surgery comes many potential inflammatory complications and quality-of-life issues for patients that require intense follow-up by both surgeons and gastroenterologists,” says Maia Kayal, MD, previously a fellow at Mount Sinai who was chosen by the IBD leadership team to head up the Comprehensive Pouch Program. “Our clinic helps to minimize disability and maximize positive outlook by providing that co-management capability. It gives patients a highly supportive home base they know they can come to if any problems or concerns develop.”
75
5 to 10
J-pouch surgery has become the gold standard for medically refractory ulcerative colitis, representing a vast improvement over previous surgery requiring a permanent ostomy. Yet the incidence of pouchitis—the most common type of postoperative inflammation—remains a persistent problem. In one of the first research projects she led over the past five years, Dr. Kayal found that approximately 30 percent of patients undergoing pouch surgery are at risk of developing chronic antibiotic-refractory pouchitis, or Crohn’s disease-like pouch inflammation, which may require recycling the same medications they were on before surgery.
“It’s really unfortunate to see patients experiencing the same symptoms they had presurgery, such as urgency, nocturnal awakenings, and bleeding,” notes Dr. Kayal, Assistant Professor of Medicine (Gastroenterology) at Icahn Mount Sinai. Findings from the multiple studies she has conducted on pouchitis prevalence convinced Dr. Kayal that J-pouch patients have an overwhelming need for standardized care and support. From that awareness, the Comprehensive Pouch Program was born.
“The program attempts to get ahead of postsurgery issues through protocols that require lab work and stool samples every three to six months,” Dr. Kayal explains. “Patients in the program can also draw on the expertise of nutritionists, nurses, psychologists, and social workers, depending on their specific needs. We’re often able to help struggling patients with some fairly simple tweaks to their diet and medications, or by introducing stress- and anxiety-reducing techniques.”
Among UC patients most in need of counseling are women considering pregnancy. Studies have shown a nearly 50 percent risk of infertility following J-pouch surgery because of scar tissue that builds up around the Fallopian tubes. But that finding was based largely on traditional open J-pouch surgery; clinicians and researchers at Mount Sinai are now determined to learn if the rate of infertility remains that high in the age of laparoscopic surgery. The research team, led by Zoe Gottlieb, MD, Assistant Professor of Medicine (Gastroenterology), has thus created the first-ever prospective fertility registry of women who have had the surgery at Mount Sinai, along with the Pre-Conception and Pregnancy Planning Clinic, to provide informed answers to questions of infertility.
“We want to be the final authority for women who may have delayed having surgery they really need because of the fear of infertility,” says Dr. Dubinsky. “And in keeping with the Pouch Program’s overriding focus on patient-centered care, we closely manage these women through their pregnancy and postpartum.”
Featured
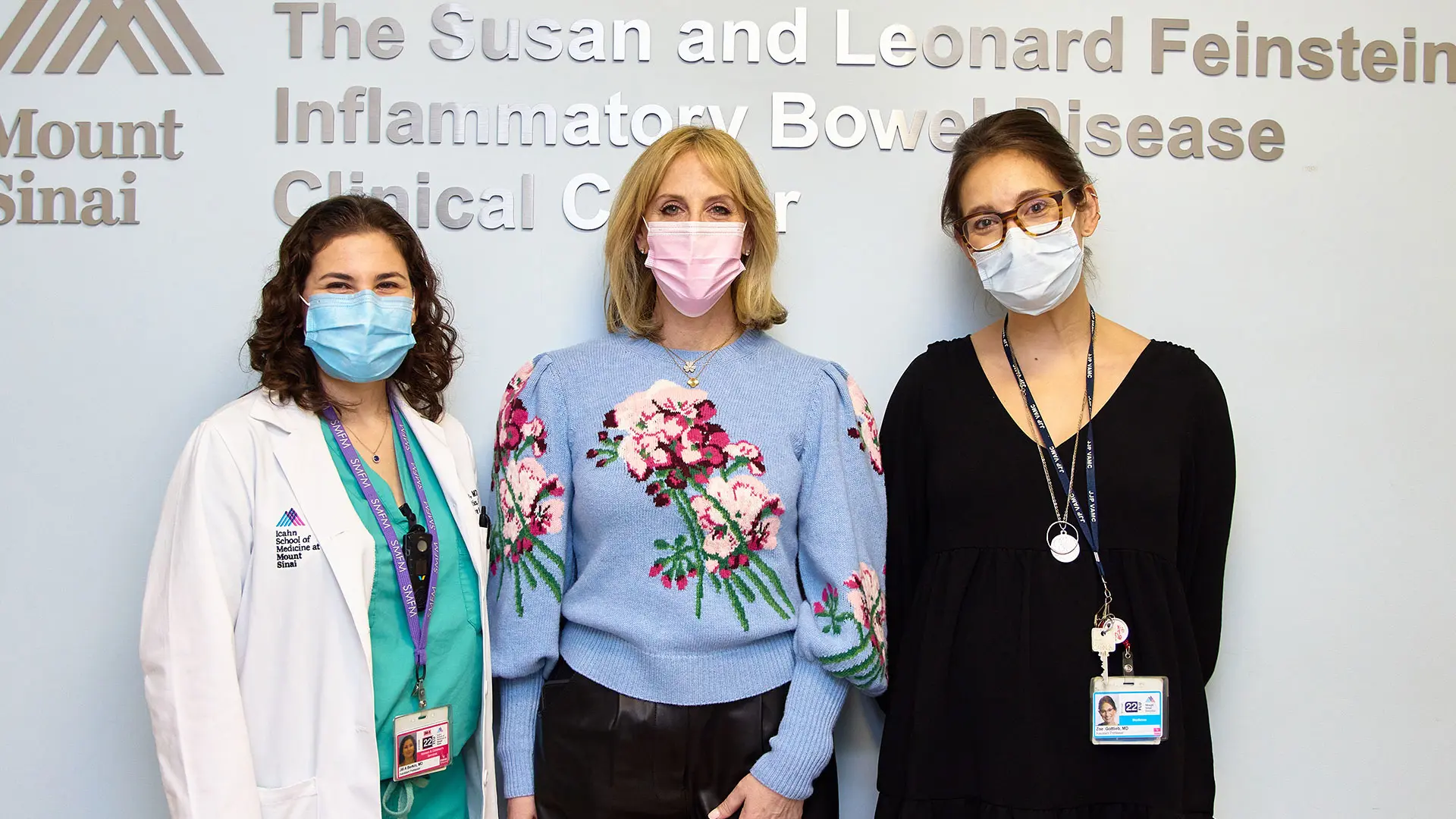
From left: Jill Berkin, MD, Assistant Professor of Obstetrics, Gynecology, and Reproductive Science, the program's lead OB/GYN specialist; Marla Dubinsky, MD; Zoe Gottlieb, MD
