Malnutrition is a common side effect in severe cases of inflammatory bowel disease (IBD), but a groundbreaking program at Mount Sinai’s Susan and Leonard Feinstein Inflammatory Bowel Disease Clinical Center is making significant inroads against it.
The first-of-its-kind program, known as iNourish, offers a full range of nutrition-focused clinical and research initiatives to support individuals with Crohn’s disease and ulcerative colitis. This platform includes a dedicated multidisciplinary clinic focused on malnutrition, which affects up to 70 percent of hospitalized IBD patients.
“Because malnutrition is so prevalent in the IBD population and has such a significant impact on clinical outcomes, it’s incredibly important to screen these patients and then implement a timely and effective intervention to improve their lives over the long run,” says Stephanie Gold, MD, Assistant Professor of Medicine (Gastroenterology) at the Icahn School of Medicine at Mount Sinai. She established iNourish in August 2022 and runs the malnutrition clinic along with clinical dietitian Laura Manning, MPH, RD, CDN.
“Our patients recognize the importance of diet in their treatment regimen, whether it’s in conjunction with a biologic or on its own,” Dr. Gold says. “If they’re malnourished, their primary concerns are restoring their nutrition status, preventing sarcopenia, and improving symptoms associated with malnutrition such as fatigue, weakness, confusion, and poor wound healing.”
The iNourish program is the umbrella for a host of IBD- and nutrition-focused initiatives. They include a multidisciplinary malnutrition specialty outpatient clinic, a dedicated inpatient IBD nutrition team, an active research initiative that has already shown highly favorable patient outcomes from its screening and intervention model, and a weight management program (dubbed WeightWise GI), which will be launching shortly.
The malnutrition outpatient clinic at The Mount Sinai Hospital has grown exponentially in its brief lifetime, treating about 200 patients to date. An initial visit embraces extensive anthropometric testing (including body composition assessment and muscle ultrasound); a detailed malnutrition assessment, screening for food insecurities as well as disordered eating patterns; and professional guidance from Dr. Gold, a gastroenterologist with specialty nutrition training, and Ms. Manning on healthful diets for patients with IBD, weight restoration, and improvement in muscle health.
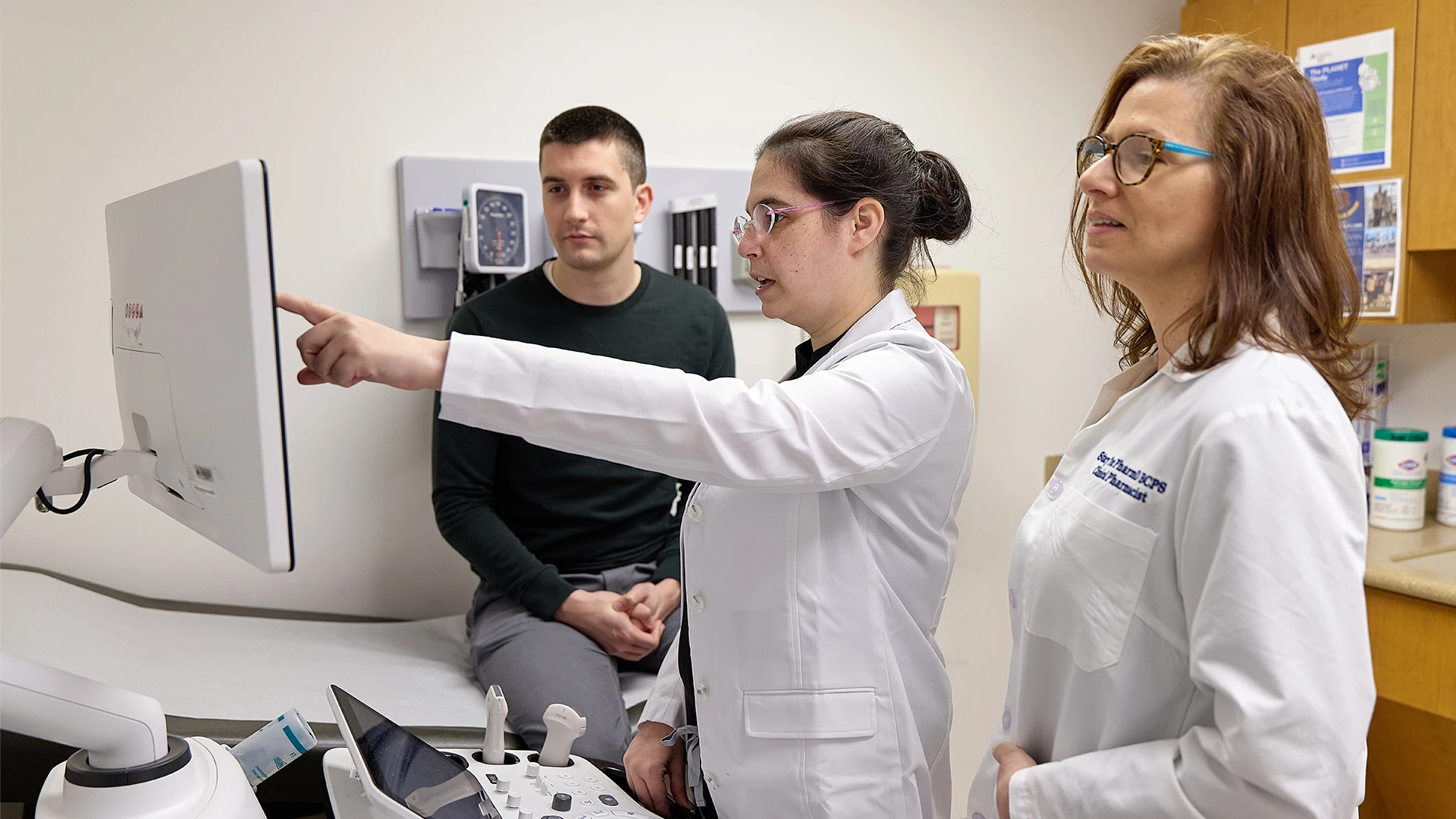
Stephanie Gold, MD, center, and Laura Manning, RD, right, help IBD patients develop diet plans to ensure proper nourishment.

Dr. Gold and Ms. Manning run the program, known as iNourish, which was established in 2022.
“Patients read a lot online about what to eat and not to eat,” acknowledges Dr. Gold. “After a careful assessment, we develop for them a thoughtful, evidence-based dietary plan based on their clinical history, hydration needs, and weight goals.”
That dietary blueprint is particularly important for IBD patients who have become malnourished due to any of a number of issues, including chronic inflammation in the gastrointestinal tract, reduced appetite from gastrointestinal symptoms, malabsorption, side effects from medications, and changes to the bowel following surgery. For patients intent on using diet as a therapeutic tool, whether alone or in combination with standard therapies, Dr. Gold and her team often recommend a Mediterranean-style diet heavy on fresh fruits, vegetables, and whole grains, or the Crohn’s Disease Exclusion Diet, which may be more tolerable for patients than the Exclusive Enteral Nutrition Diet by incorporating liquid nutrition and specific anti-inflammatory whole foods such as bananas, apples, eggs, chicken, and potatoes.
The effectiveness of Mount Sinai’s novel malnutrition screening and counseling approach was highlighted in a poster presentation at the Digestive Disease Week meeting in Washington in May 2024 and published in Gastroenterology. Based on data from the study involving 322 patients who had a positive malnutrition screening, the program’s interventions were associated with meaningful improvements in both nutritional outcomes and patient self-confidence in making dietary choices.
Beyond the clinic, the dedicated iNourish team is breaking ground in IBD dietary research. Among the projects being led by Dr. Gold is an evaluation of patients with Crohn’s disease who undergo a surgical resection; understanding dietary patterns in patients with a J-pouch; investigating the impact of partial enteral nutrition in combination with a biologic on clinical, endoscopic, and histologic remission; and exploring the effect of visceral adiposity on IBD outcomes and how GLP1 agonists might play a role in altering disease progression.
No mission is more critical to Dr. Gold, however, than ongoing education of both patients and providers. For the latter, she has started instructing gastroenterology fellows on the importance of nutrition in IBD care and has invited them into the malnutrition clinic for first-hand experience. A recent half-day education session for professionals and patients alike drew a virtual worldwide audience of several hundred.
“That’s the direction in which we intend to go,” affirms Dr. Gold. “We want to educate current and future IBD providers about the importance of nutrition care for these high-risk patients. By identifying and treating malnutrition early in the disease course, we can improve clinical outcomes and make a significant difference in the lives of those with IBD going forward.”
For more information on the iNourish program, contact Dr. Gold at stephanie.gold@mountsinai.org.
Featured

Stephanie Gold, MD
Assistant Professor of Medicine (Gastroenterology)
