For the 40,000 new rectal cancer patients each year in the United States, chemoradiation has proven increasingly successful in eradicating tumors that threaten the anal sphincter. That’s scant consolation, however, for individuals with aggressive low rectal lesions that don’t respond completely to chemoradiation and are too difficult for laparoscopy or robotic surgery to reach.
An advanced surgical technique known as transanal total mesorectal excision (taTME), developed nearly 15 years ago by Patricia Sylla, MD, Chief of the Division of Colon and Rectal Surgery at the Mount Sinai Health System, could potentially help many of these patients preserve their sphincters. Unfortunately, many oncologic surgeons are unaware the procedure exists, and only 11 sites across the country perform it in meaningful volume.
“It’s clear that many more patients should be referred to an expert taTME center to determine if they’re a candidate for sphincter salvage, but we just don’t see that happening yet,” says Dr. Sylla, Professor of Surgery at the Icahn School of Medicine at Mount Sinai, who has trained surgeons around the world on the complex technique that combines both abdominal and transanal dissection. “Patients in danger of losing their anal sphincter should know they have options other than removal of their rectum and anus through an abdominoperineal resection, requiring creation of a permanent ostomy bag. Unless the tumor has completely invaded the sphincter, at least partial sphincter preservation is possible with taTME.”
A timely new study led by Mount Sinai promises to raise the profile for transanal TME. The phase 2 trial at 11 sites across North America is the largest to date to confirm the safety and favorable pathologic outcomes of the procedure when performed by experienced surgeons using a two-team hybrid approach. At the center of the study, published in Surgical Endoscopy in September 2023, were 100 patients with stage I-III rectal adenocarcinoma located less than 10 cm from the anal verge.
Among the most important findings was that taTME resulted in only a 2 percent rate of conversion to open abdominal surgery. Elaborates Dr. Sylla: “When tumors are very low—6 cm or less—conversion rates are as high as 15 percent as surgeons struggle to get below the tumor. With transanal TME, those rates are well under 5 percent because we use two collaborative teams that work simultaneously. One team performs the more straightforward ‘upper’ part of the rectal resection laparoscopically or robotically, while a specially trained transanal surgeon performs the ‘bottom’ or more complex part of the rectal dissection. This hybrid approach is technically demanding and resource-intensive, but it cuts down on the mental workload for surgeons and, I believe, is faster and safer.”
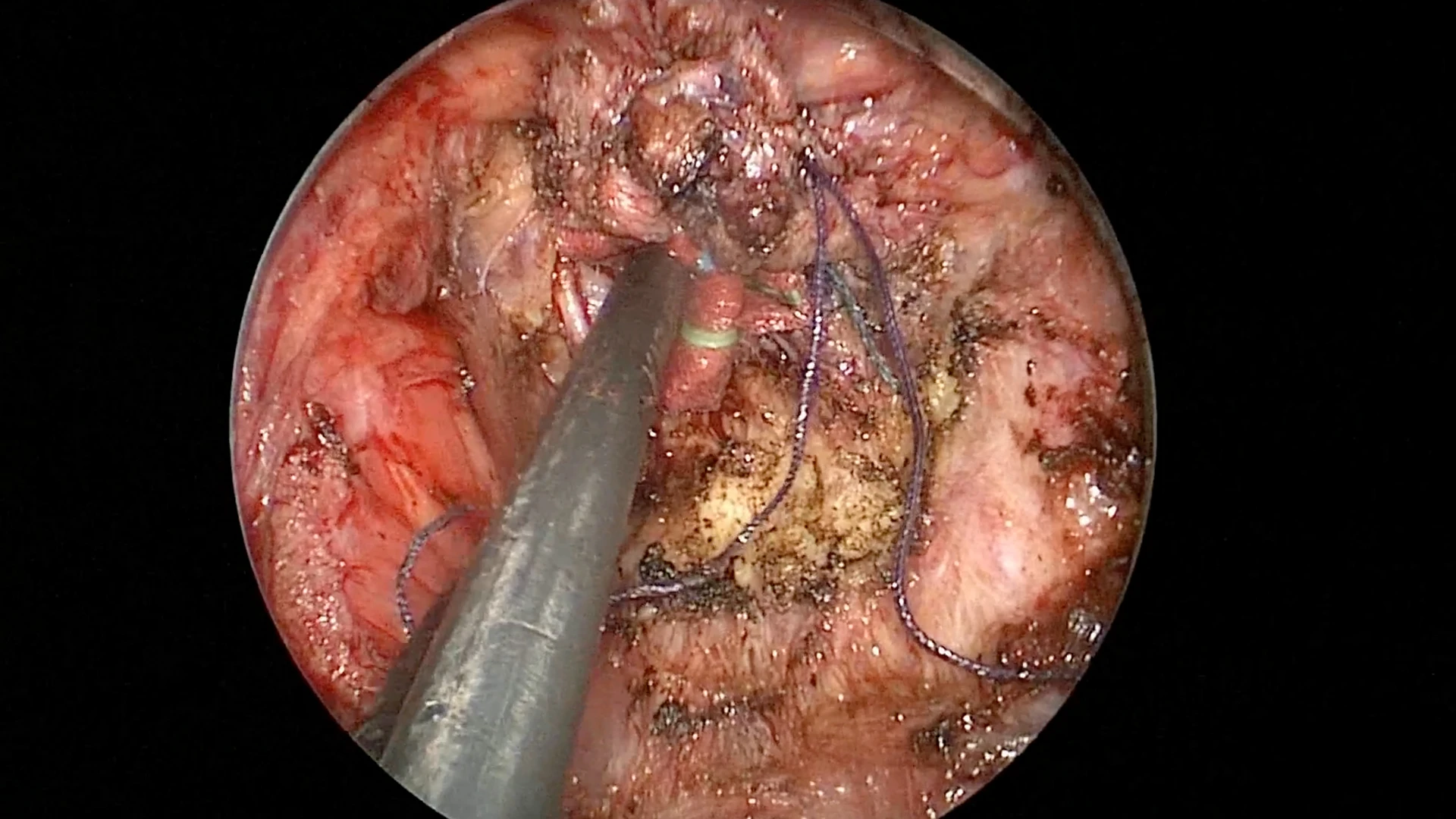
Watch Dr. Sylla perform a taTME procedure in this video.
The effectiveness of taTME was further reflected in the stoma closure rates reported in the Mount Sinai-led study of 70 male and 30 female patients. This key metric showed that 93 percent of temporary stomas were closed by 12 months, and 98 percent by 23 months, following surgery. Dr. Sylla termed these results “excellent” inasmuch as they are a marker for proper healing and overall success of the surgery. No less meaningful was mesorectal TME grade achieved—a critical pathologic endpoint based on a postsurgical specimen that serves as a strong predictor of local recurrence and disease-free survival, as well as of overall surgical quality. Investigators found that complete or near-complete TME grade was achieved in 90 percent of all surgeries.
Because rectal cancer surgery is complex, particularly in patients who have previously been treated with chemoradiation, the study showed 30-day and 90-day morbidity rates of 49 percent and 56 percent, respectively. What’s more, anastomotic complications were reported in 18 percent of patients. While acknowledging those rates are high, Dr. Sylla notes that most leaks and complications were not severe and fully correctable, as evidenced by the favorable stoma closure rates following surgery.
The surgical/research team under Dr. Sylla is now focused on functional results in patients treated with taTME. To that end, it presented in April 2024 at the American Surgical Association meeting findings in the areas of sexual, urinary, and defecatory function at three to four months and nine to twelve months after ileostomy closure. Those results will soon be published in Annals of Surgery.
“For now, we can confidently say that our study validates the safety and integrity of taTME for patients with complex low rectal tumors who want to avoid the trauma of a permanent ostomy,” says Dr. Sylla. “Our hope is that there is a taTME center near them where they can get an expert second opinion on preserving their sphincter through transanal TME.”
Featured

Patricia Sylla, MD
Professor of Surgery