Surgery may be superior to medication as a first-line therapy for some patients with Crohn’s disease, according to a new study by researchers at the Icahn School of Medicine at Mount Sinai and the Center for Molecular Prediction of Inflammatory Bowel Disease (PREDICT) at Aalborg University in Copenhagen, Denmark. The research could point toward a paradigm shift in Crohn’s disease treatment.
Traditionally, patients with Crohn’s disease are treated with anti-tumor necrosis factor (anti-TNF) therapy, such as infliximab. Surgery is usually reserved for people who do not respond to medication, experience adverse side effects, or develop complications of Crohn’s disease, such as fistulas or blockages. But some evidence has suggested earlier surgery may benefit patients. The randomized LIR!C trial showed that patients with limited, non-stricturing ileocecal Crohn’s disease who underwent ileocecal resection (ICR) as a primary treatment had improvements in quality of life similar to those who took infliximab.
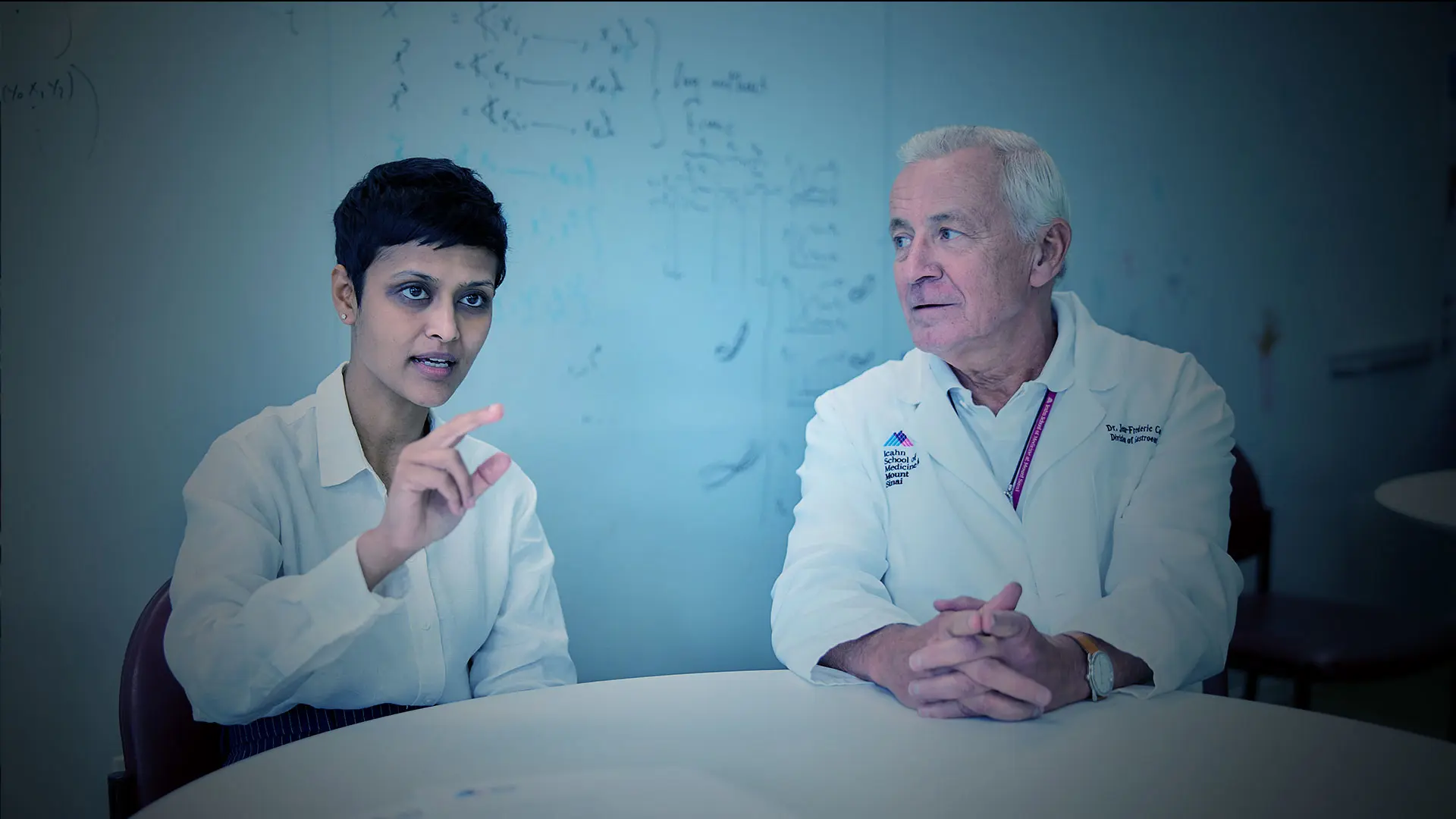
Manasi Agrawal, MD, MS, a gastroenterologist at The Mount Sinai Hospital and Assistant Professor of Medicine (Gastroenterology) at Icahn Mount Sinai, wanted to see how early surgery compared to anti-TNF therapy in the real world. She co-led the study with Anthony C. Ebert, PhD, a postdoctoral researcher at PREDICT, in collaboration with Kristine H. Allin, MD, PhD, Associate Professor and Partner in PREDICT, Jean-Frederic Colombel, MD, Co-Director of the Susan and Leonard Feinstein Inflammatory Bowel Disease Clinical Center at Mount Sinai, and other colleagues in Copenhagen and New York. They accessed Denmark’s cross-linked national health registries, which provided a rich data set that included the entire Danish population. PREDICT is led by Tine Jess, MD, DMSc, a professor at Aalborg University.
The researchers looked at individuals treated for Crohn’s disease between 2003 and 2018, following them over time to compare long-term outcomes between those treated with infliximab and those treated with early ICR. The primary outcome in their analysis was a composite of one or more of the following outcomes more than 30 days after initial treatment:
Crohn’s disease-related hospitalization
Systemic corticosteroid exposure
Major Crohn’s disease-related surgery
Perianal Crohn’s disease, one of the more serious complications of the illness
The risk of experiencing this composite outcome was 33 percent lower in patients who underwent surgery as a primary treatment. The results were published in Gastroenterology.
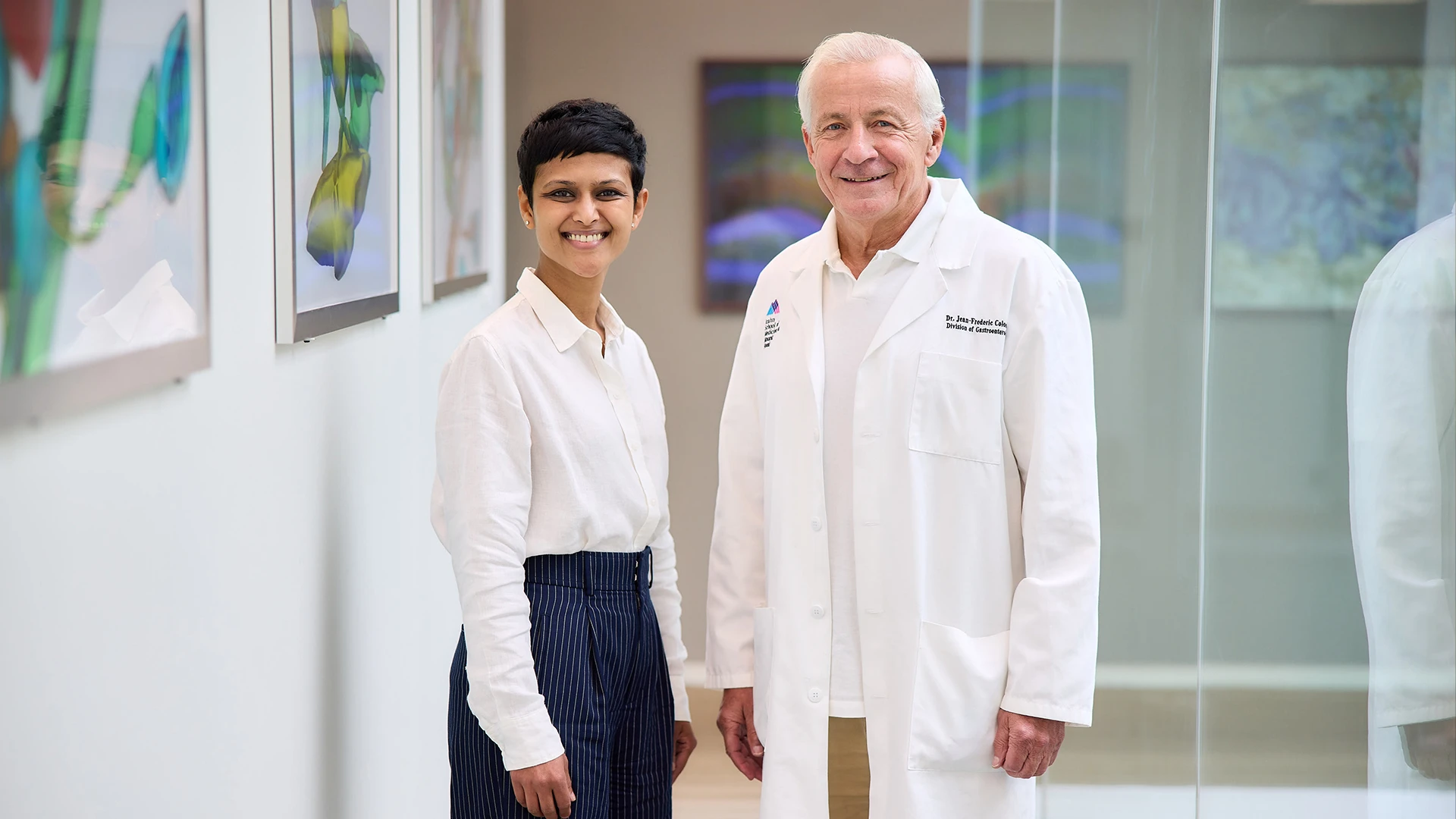
Manasi Agrawal, MD, MS, and Jean-Frederic Colombel, MD
In a secondary analysis, the researchers closely examined each outcome to better understand the impact of early surgery. They found no difference in hospitalizations or the development of perianal Crohn’s disease between patients in the two groups.
They did, however, find a 44 percent risk reduction in future Crohn’s disease surgeries among the patients in the surgery group compared with the infliximab group. What’s more, they found a 29 percent reduction in corticosteroid use in patients who had early ICR.
“Systemic corticosteroids are very common in patients with inflammatory bowel disease, but they come with several side effects. One of our goals as physicians is to minimize corticosteroid use, so this is an important finding,” Dr. Agrawal says.
Anti-TNF agents have been important tools for managing Crohn’s disease, but they can have considerable side effects, including increased infection risk. And in many patients, the treatments are ineffective or partially effective and lose efficacy over time. They’re also expensive and out of reach for patients in many parts of the world, Dr. Agrawal notes. “Inflammatory bowel disease is increasing in many developing and recently developed countries, where long-term biologic treatment is cost-prohibitive for many individuals. Surgery may be an important consideration in more resource-limited settings,” she says.
Dr. Agrawal and her colleagues at Mount Sinai’s Feinstein Inflammatory Bowel Disease Center are continuing this line of research, looking for ways to identify which patients stand the best chance of benefiting from early surgery. In the meantime, she says, this population-based study suggests physicians might consider changing their approach to treating some Crohn’s disease patients.
"The data for early surgery are very promising, but this is a treatment that needs to be considered for the right patient: Someone whose disease is limited to a short segment of the ileocecal region, with no previous perianal disease or inflammation elsewhere,” she says. “For the right patient, ICR can certainly be brought to the table. This is a paradigm shift in how we position our treatment options for patients with Crohn’s disease.”