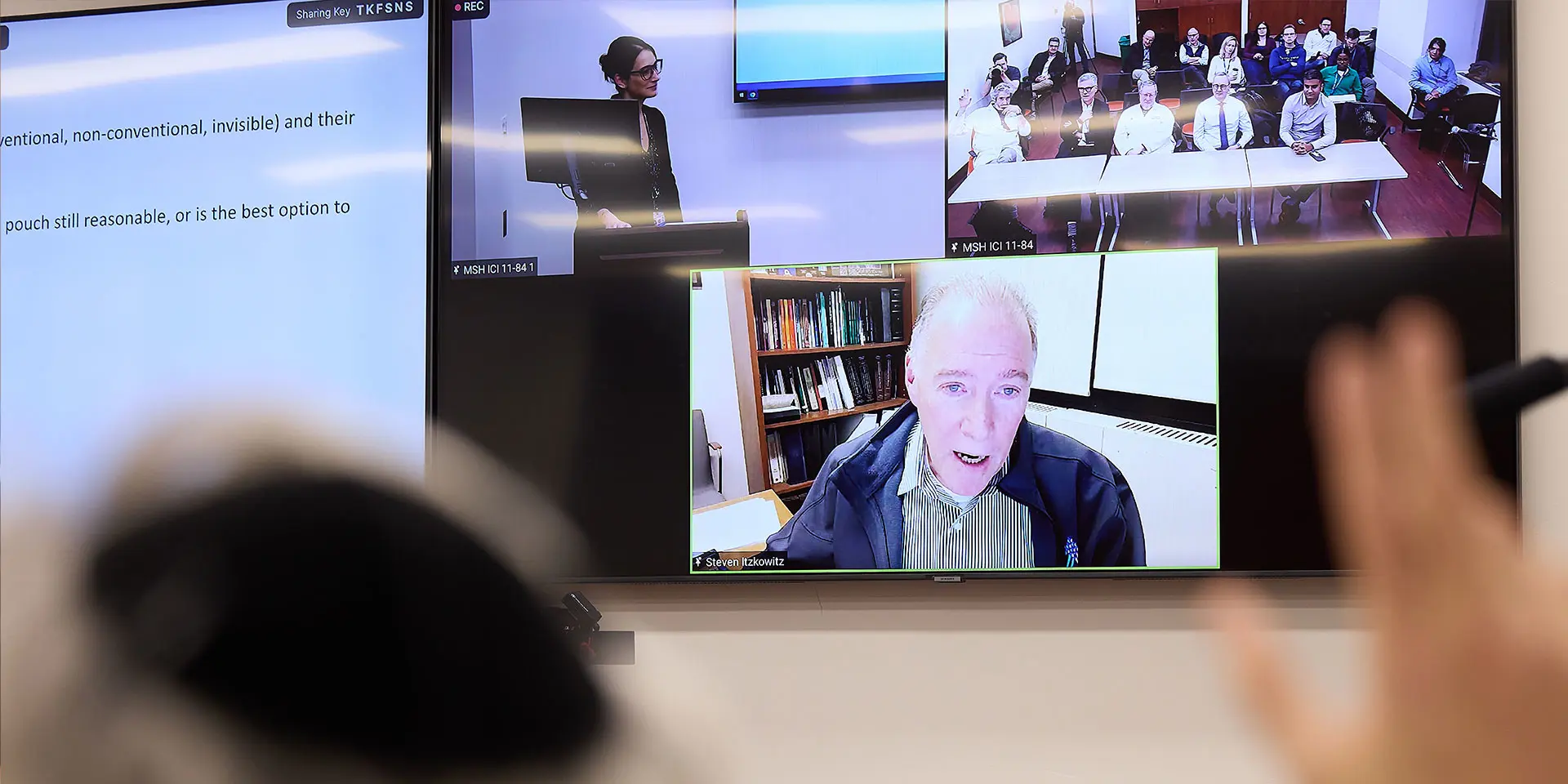
A recently launched Mount Sinai Health System program to help community physicians address inflammatory bowel disease (IBD) has given new meaning to the time-honored practice of medical rounds as a physician training tool.
The program, known as IBDebrief, brings Mount Sinai doctors practicing in the community together with nationally recognized experts from the Dr. Henry D. Janowitz Division of Gastroenterology to review often-complex cases and grow their knowledge base. It is especially helpful for IBD, a field where complicating factors and the onrush of new medicines in recent years have proven challenging for local providers.
“We believe we have a responsibility to share the vast amount of knowledge our faculty possesses in this field with physicians in the community,” says Zoë Gottlieb, MD, Assistant Professor of Medicine (Gastroenterology) at the Icahn School of Medicine at Mount Sinai, who organizes and leads each IBDebrief session. “We know it can be difficult for providers who don’t see IBD patients on a regular basis to create and implement treatment plans, especially when the disease is complex, so we’ve created a learning program that allows them to ask questions and get informed answers from our IBD experts at Mount Sinai.”
Those experts include Bruce Sands, MD, MS, the Dr. Burrill B. Crohn Professor of Medicine, and Chief of the Division of Gastroenterology at Icahn Mount Sinai, and Jean-Frédéric Colombel, MD, Professor of Medicine (Gastroenterology) and Director of the Susan and Leonard Feinstein Inflammatory Bowel Disease Clinical Center at Mount Sinai. Another contributor has been David Sachar, MD, Director Emeritus of the Division of Gastroenterology, the first American elected chair of the International Organization for the Study of Inflammatory Bowel Disease, and a legendary figure in the field of IBD.
Dr. Sands and Dr. Colombel began formulating plans for an IBD education network years ago, similar to Project Echo, the highly successful national model that engages clinicians in a virtual community with their peers to share knowledge, guidance, and professional support. When a grant from Pfizer provided the funding spark, they teamed up with Dr. Gottlieb to create IBDebrief, and have served as members of the panel of experts that is assembled for each session.
“What’s unique about this program is that the learning occurs around community physicians’ own IBD patients, rather than ours,” explains Dr. Sands. “We’re hopeful this type of engagement will continue to bring them back to learn more about the use of best practices for their patients.”

Bruce Sands, MD, MS, and Abhik Bhattacharya, MD, Assistant Professor of Medicine (Gastroenterology), at a recent IBDebrief meeting
IBDebrief, scheduled for the first Tuesday of each month, packs copious amounts of information into each hour-long session, and offers attendees continuing medical education credits. Doctors are surveyed prior to the session, and an opening “hot topic” identified in that survey is addressed in a 15-minute overview by an IBD expert. In the first gathering, the topic was management of moderate-to-severe Crohn’s disease; in the next, how to select the appropriate biologic therapy.
Next, the expert panel takes center stage to conduct an in-depth review of a case suggested in advance by one of the participants, supported by the patient’s anonymized medical records from the Mount Sinai Health System, including radiology reads, endoscopic photos, and pathology reports.
“These are IBD patients who may or may not have had complicated courses, so the question on the table is how to best manage them,” explains Dr. Gottlieb, who is also the Associate Director of Mount Sinai’s IBD Preconception and Pregnancy Planning Clinic. “In the first session, we reviewed the case of a patient with very mild colonic Crohn’s, which is often harder to manage than a more complex case because there’s not necessarily a straightforward path, nor are there many medicines for mild forms of the disease.”
In the second session, the subject turned to an IBD patient who had failed almost every biologic medicine, with the next option being a JAK inhibitor. Complicating matters was the fact that the patient had a history of blood clots, posing the dilemma for the panel of experts: how do you weigh administering a medicine that may increase the risk of an adverse event against the benefit of helping a patient with no other real treatment options? Future topics are set to include therapeutic solutions using new biologics and small molecules, and IBD in special populations, such as pregnant patients and the elderly.
The high praise that the participating Mount Sinai doctors have voiced for the program in its early days is reinforcing plans by organizers to grow their effort to include physicians outside the Health System.
“We’d like to see IBDebrief expand regionally and ultimately nationally,” declares Dr. Gottlieb. “Everyone wants these patients to get the best possible care, and we believe we’re taking a major step in that direction by sharing the wisdom of some of the world’s leading minds in IBD with a broad physician population that can clearly benefit from that expertise.”