But this remarkable complexity comes with some notable downsides. Neurons are highly sensitive to stress and physical injury, they can be irreversibly damaged by infectious agents and chemicals in the environment, and unlike many other cells in the body they cannot self-replicate to replace damaged or aged neurons in the adult brain.
Unsurprisingly, disorders of the central nervous system (CNS), encompassing brain and spinal cord, are the least understood and the most difficult to treat of any health affliction: more than 700 million people worldwide currently have a debilitating CNS disorder. In the United States, life expectancy has fallen for the first time in decades, a shocking trend driven by so-called “deaths of despair” involving suicides, drug overdoses, diseases attributable to stress or substance abuse, and other mental health-related issues, further exacerbated by the COVID-19 pandemic.
Despite their prevalence and devastating impact, few CNS disorders are fully treated by available medications or other approaches. For example, there are currently no efficacious treatments to slow the progression of Alzheimer’s disease and other neurodegenerative disorders, lessen the debilitating cognitive deficits associated with schizophrenia and other psychotic disorders, prevent relapse in drug-addicted individuals, or alleviate the core symptoms of autism.
Few CNS disorders are effectively treated by current medications.
Significantly, most major pharmaceutical companies have scaled back their efforts to develop new treatments for CNS disorders. They cite difficulties getting drugs across the blood-brain barrier, and challenges in designing drugs that act selectively at their targets in the brain to exert a beneficial effect without also causing adverse side effects.
The Friedman Brain Institute (FBI)—in close collaboration with Mount Sinai’s Drug Discovery Institute—is taking a leadership role in efforts to advance therapeutic discovery. Our goal is to catalyze the development of much-needed new medications for the psychiatric and neurological disorders that are currently being investigated in our labs.
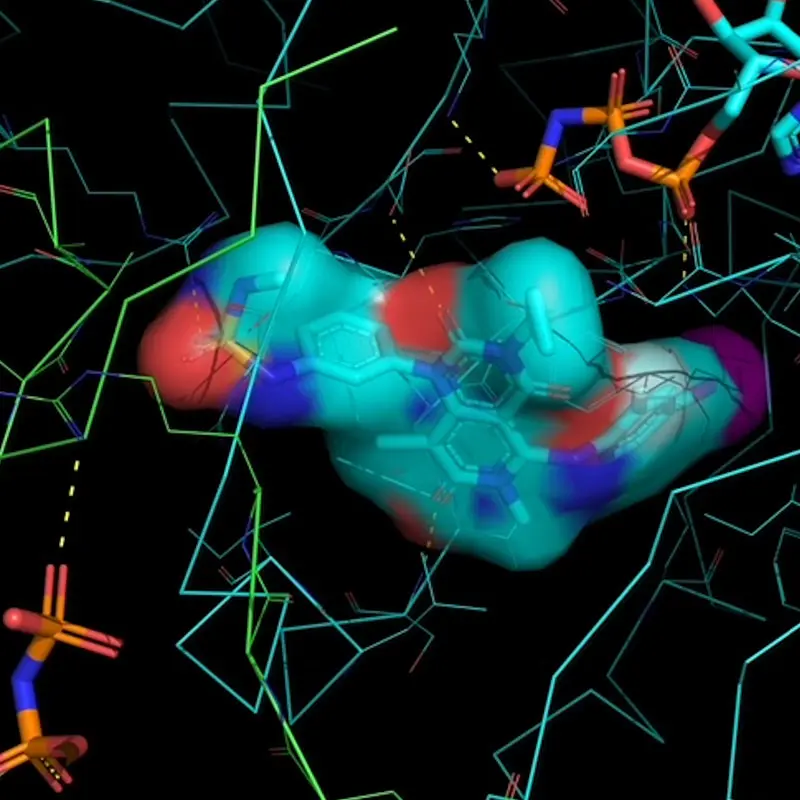
Above image: Binding of a small molecule drug at the interface of a protein-protein complex. Compounds of this class, referred to generally as ‘molecular glues,' offer powerful tools to rewire signal transduction cascades or short circuit disease pathways. Examples include drugs such as rapamycin and thalidomide. Recent work has identified a new class of compounds with molecular glue activity to target the RAS pathway. Credit: Arvin Dar, PhD, Professor, Oncological Sciences, and Pharmacological Sciences
We have recruited world-class scientists with the types of drug discovery expertise rarely seen in academic institutes and are investing in the infrastructure necessary to design and test new drugs. We are pushing the boundaries of artificial intelligence (AI) and other computational approaches to accelerate drug discovery.
We have some of the most prominent scientists studying GPCRs...
…a class of proteins considered exceptional drug targets.
The FBI is also home to some of the most prominent scientists working on a class of proteins called G protein-coupled receptors (GPCRs). This is important because GPCRs are known or suspected to be involved in a host of brain disorders and are considered exceptional targets for drug development. As many as 40 percent of all medications currently approved by the U.S. Food and Drug Administration exert their beneficial effects by targeting GPCRs. Raising further interest in GPCRs are recent breakthroughs in structural biology that are revealing new insights. Novel chemistry strategies are emerging that can be used to manipulate GPCRs in safe and effective ways, and AI tools are beginning to yield new GPCR drugs.
FBI scientists are also working on entirely new classes of drug targets. For example, our scientists have identified novel processes in neurons that regulate the expression of genes involved in psychiatric disorders such as drug addiction, depression, and autism. We expect that drugs that manipulate these transcriptional and epigenetic processes, including noncoding RNAs, will someday deliver “next generation” CNS medications.
Read on as we highlight some of the most promising recent advances our scientists have made in GPCR biology and chemistry—and the insights they have gained—as they explore new paths in CNS medication development.