It turns out that when our brain senses a threat in the environment (even a psychological or social one) it sends signals—via a complex network of peripheral nerves—that mobilize the immune system, readying it to protect us from injury. While critical for survival, such brain-mediated activation of the immune system when it is excessive and prolonged can lead to a wide array of illnesses, including cardiovascular disease and depression. Recent studies by Icahn School of Medicine at Mount Sinai researchers have begun to advance understanding of the bidirectional connections between the brain and the immune system that mediate these effects.
Major depressive disorder (MDD) is the leading cause of worldwide disability and the most common mood disorder. The prevalence of MDD is two- to threefold higher in patients with cardiovascular disease and, conversely, MDD is associated with an ∼80% increased risk of cardiovascular morbidity and mortality.
Major depressive disorder: the leading cause of worldwide disability
It’s 2-3 times more prevalent in patients with cardiovascular disease.
Chronic inflammation has been associated with atherosclerotic plaque formation, progression, and rupture, likely contributing to the pathogenesis of cardiovascular disease and heart failure. Concomitantly, clinical studies report higher levels of peripheral inflammation in a subset of patients with MDD, a pattern that has been replicated in animal models of depression.
Work from the laboratories of Filip Swirski, PhD, who will be joining Mount Sinai in June 2021 as Director of the Cardiovascular Research Institute, and Zahi A. Fayad, PhD, Director of the BioMedical Engineering and Imaging Institute, has shown that chronic stress mobilizes the immune system and stimulates enhanced production of monocytes, a type of immune cell that produces inflammatory molecules known as interleukins that then circulate throughout the bloodstream and can contribute to chronic pathology such as atherosclerosis, the leading cause of heart attack and stroke.
Given the high comorbidity between these cardiovascular risk factors and depression, it is believed that chronic stress increases risk for both conditions by activating shared immune mechanisms. Therapeutic strategies to reduce inflammation, which are known to benefit patients with cardiovascular disease, are currently being tested for their antidepressant properties, especially in the subtype of patients who display evidence of a hyperinflammatory state. In mice, drugs targeting the immune system are well documented to have pro-resilient and antidepressant-like properties.
Groundbreaking research in human depression, currently being conducted at Mount Sinai by the Depression and Anxiety Discovery Center led by James Murrough, MD, PhD, shows great potential for novel immunomodulatory drugs to treat MDD. Such a strategy, if successful, could result in the development of one of the first biologically distinct classes of antidepressant therapeutics in several decades.
Inflammatory molecules diffuse more readily into the brain following prolonged periods of stress in animal models.
- Scott Russo, PhD, and Miriam Merad, MD, PhD
A major research question being tested at Mount Sinai is how interleukins and other peripheral inflammatory molecules interact with the brain—and vice versa—to control disease. Work led by Scott Russo, PhD, Director of the Center for Affective Neuroscience, and Miriam Merad, MD, PhD, Director of the Precision Immunology Institute, has demonstrated that inflammatory molecules diffuse more readily into the brain following prolonged periods of stress in animal models. This is due, in part, to stress-induced damage to blood vessels that make up the blood-brain barrier (BBB), a structure that normally functions to protect the brain from such inflammatory insults, and that this damage occurs only in selected regions of the brain important for mood and emotions. Early brain imaging investigations suggest that patients with MDD may suffer from similar damage to blood vessels in the brain.
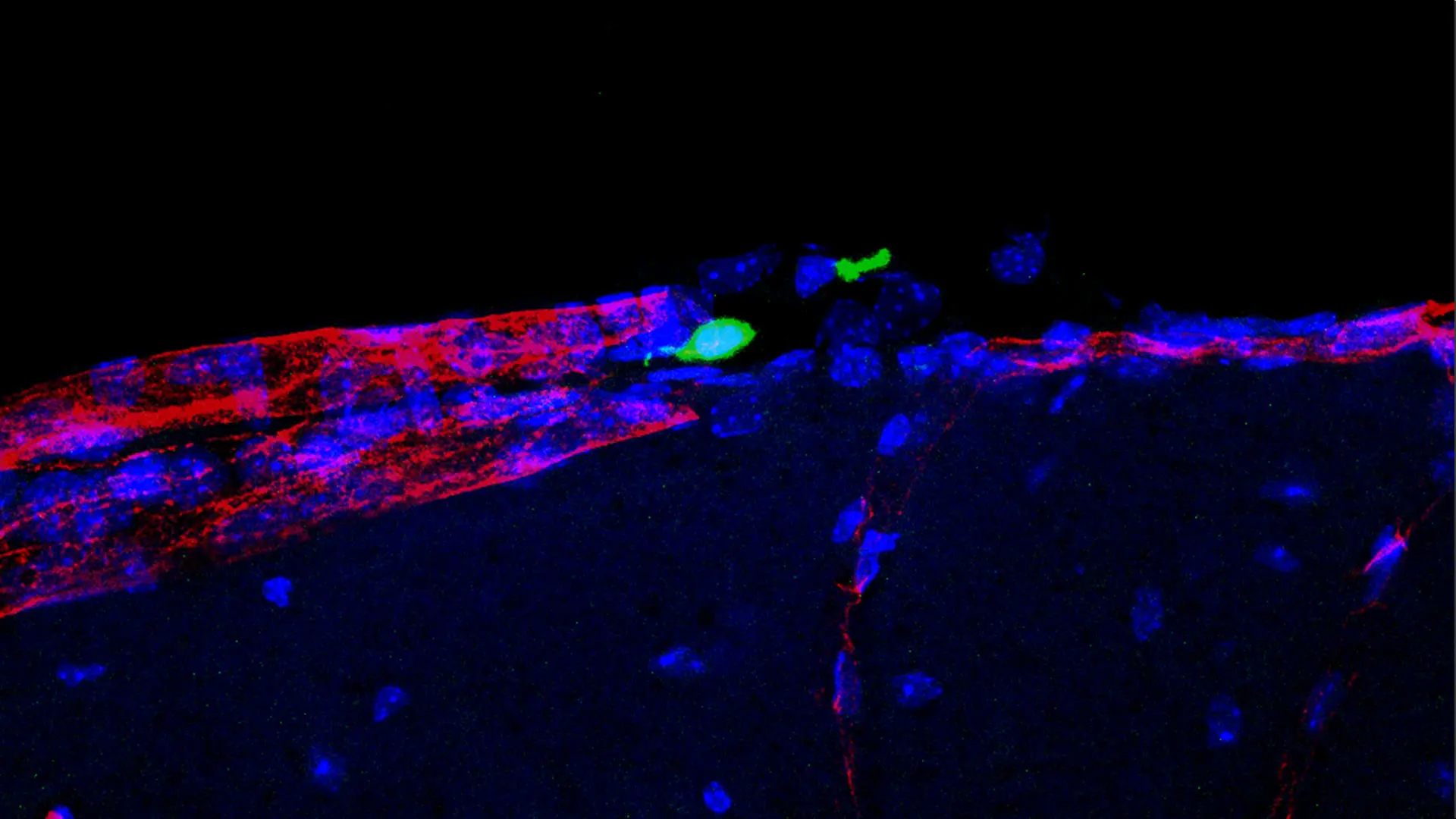
Peripheral monocytes accumulate in the meningeal space. (Created by Flurin Cathomas, MD, postdoctoral fellow, and Carrie Hsiao-Yun Lin, visiting postdoctoral fellow, Russo lab.)
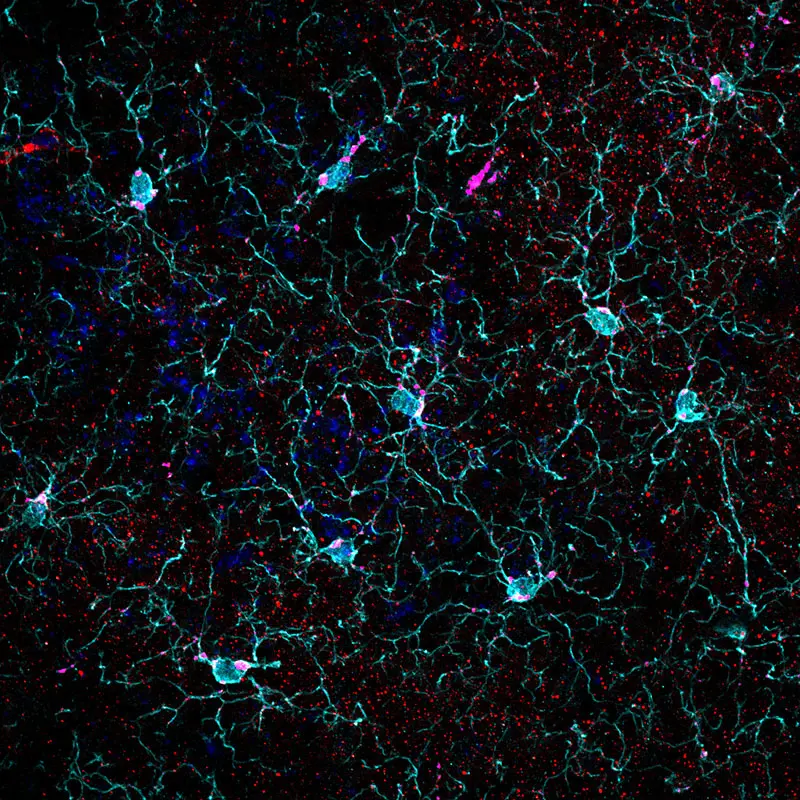
Microglia mediates synaptic pruning. (Created by Carrie Hsiao-Yun Lin, visiting postdoctoral fellow, Russo lab.)
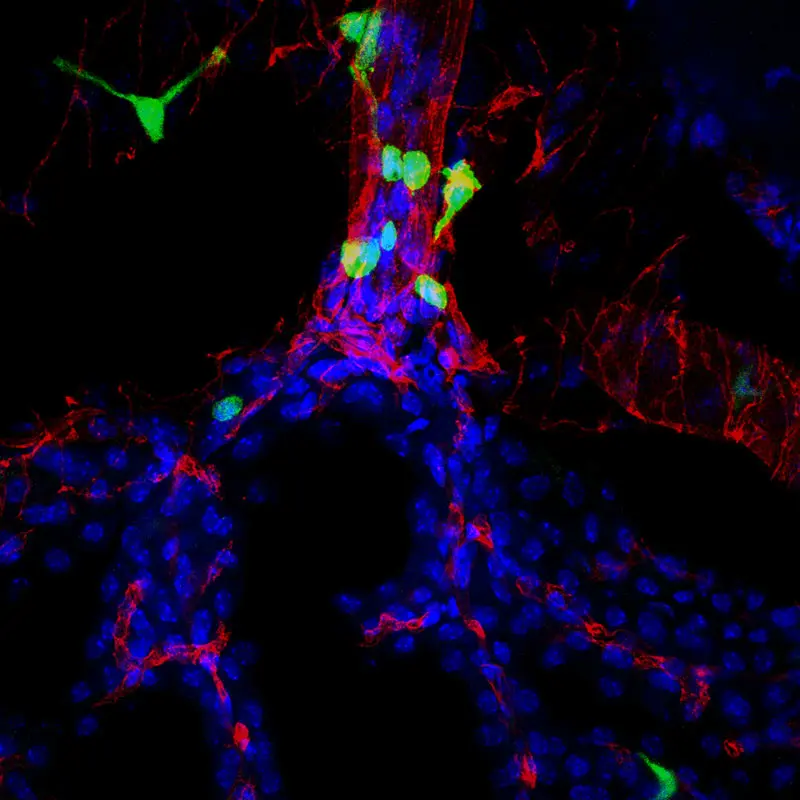
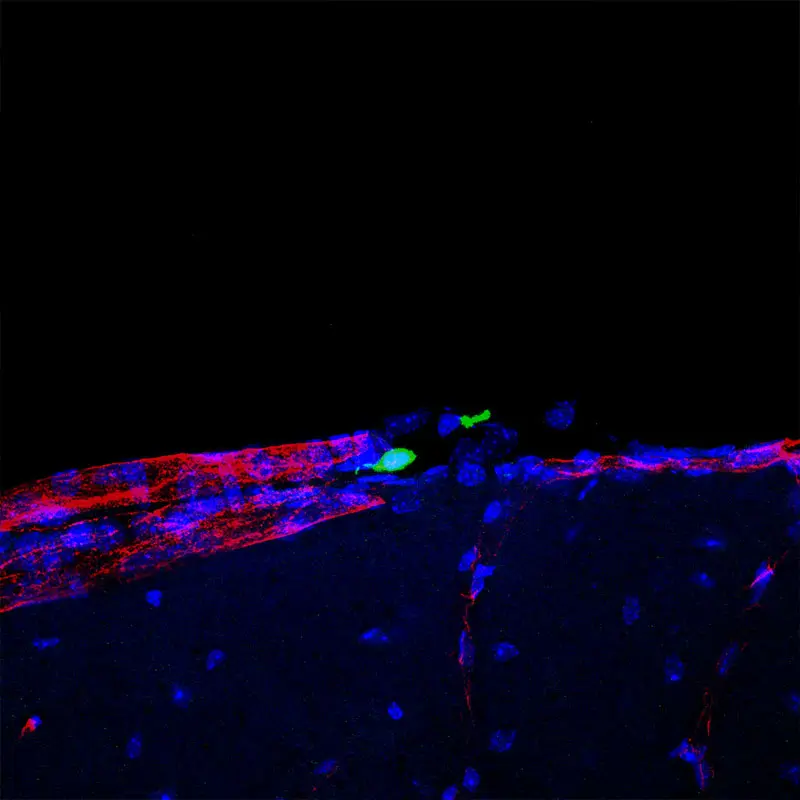
Peripheral monocytes accumulate in the choroid plexus. (Created by Flurin Cathomas, MD, postdoctoral fellow, and Carrie Hsiao-Yun Lin, visiting postdoctoral fellow, Russo lab.)
Another research interest, being explored by Drs. Swirski and Russo, is to understand how specific brain regions—acting through control of peripheral nerves—modulate immune cell function, which in turn results in damaged blood vessels contributing to increased risk for heart disease and depression. The hope is that gaining a detailed mechanistic understanding of this process at the molecular level will spur collaboration with the Mount Sinai Drug Discovery Institute, led by Paul Kenny, PhD, which can leverage these data to screen for novel therapeutic agents that can enhance repair of endothelial damage to blood vessels due to stress and prevent or reverse risk for heart disease and depression in susceptible individuals.
Increasing evidence indicates that the immune system also contributes to the pathogenesis of Alzheimer’s disease. For additional information about Mount Sinai’s leading role in this area of inquiry, read about our Interdisciplinary Center in Neural Circuitry and Immune Function, created recently with a gift from the Sanford J. Grossman Charitable Trust.
Interactions between the nervous and immune systems are representative of the brain’s reciprocal connections with all other organs in the body. Another key example is peripheral metabolism: we know that a host of brain circuits control feeding and metabolic state, and that peripheral feeding hormones and metabolites exert a powerful influence on brain function, including mood, motivation, reward, and cognition. What we eat also affects the gut microbiome, which in turn shapes both the immune and nervous systems. In light of this burgeoning field, Mount Sinai has launched the Brain & Body Research Center, under the direction of Dr. Russo, one of the first of its kind in the nation. This new Center will bring together work across numerous departments and institutes on campus and harness advances in this growing field to better diagnose and treat today’s most impactful diseases.
Featured

Scott J. Russo, PhD
Mount Sinai Professor of Affective Neuroscience, Director of the Center for Affective Neuroscience, and Professor of Neuroscience

Zahi A. Fayad, PhD
Professor of Medicine (Cardiology), and Diagnostic, Molecular and Interventional Radiology; Director of BioMedical Engineering and Imaging Institute

James Murrough, MD, PhD
Director of Mount Sinai’s Depression and Anxiety Center for Discovery and Treatment, and Associate Professor, Psychiatry, and Neuroscience

Miriam Merad, MD, PhD
Mount Sinai Endowed Professor in Cancer Immunology, Director of the Precision Immunology Institute, Professor of Oncological Sciences, and Medicine

Filip Swirski, PhD
Senior Faculty, Department of Medicine (Cardiology)