When COVID-19 swept across New York City in early 2020, few medical specialties felt the disruption as acutely as otolaryngology. Nasal and upper airway surgeries were paused at Mount Sinai to protect patients, surgeons, and staff from potential exposure to SARS-CoV-2, leaving patients without critical interventions. For Alfred-Marc Iloreta Jr., MD, the crisis demanded a solution.
Dr. Iloreta, Director, Endoscopic Skull Base Surgery, and Research, The Mount Sinai Hospital; and Assistant Professor of Otolaryngology, and Neurosurgery, and Artificial Intelligence and Human Health, Icahn School of Medicine at Mount Sinai, turned to Mount Sinai BioDesign, the Mount Sinai Health System’s hub for medical device innovation. Founded in 2018 by Joshua Bederson, MD, Mount Sinai BioDesign brings together entrepreneurs, engineers, project managers, and clinical researchers to transform unmet clinical needs into commercializable medical technologies.
“Surgeons are often the first to encounter practical challenges, unmet needs, and opportunities to improve patient outcomes,” says Dr. Iloreta. “We are in a unique position to identify inefficiencies and conceptualize novel solutions. That being said, we are also limited by training bias, engineering resources, and our ability to commercialize solutions. Mount Sinai BioDesign was pivotal—not just in helping refine the idea, but in guiding us toward something that could truly become a viable product.”
Through an iterative design process with Mount Sinai BioDesign, the concept took shape and soon drew positive feedback from outside surgeons and industry partners. After securing a Phase I Small Business Technology Transfer grant from the National Institutes of Health, Pharyvac Surgical Technologies Inc. was able to transition from concept development to product development.
“Having the Mount Sinai Biodesign lab and engineering team in the same building as the surgical team was critical to our success. The ability to identify clinical problems, develop solutions, and rapidly iterate benchtop prototypes in close collaboration with expert surgeons—incorporating immediate feedback—was a key driver of our accelerated path to commercialization. We developed solution-specific models simulating heavy intraoperative bleeding (Figure 1) and the technical demands of bimanual endoscopic drilling (Figure 2) to recreate real-world conditions and identify gaps between the ‘problem’ and the proposed ‘solution,’” says Dr. Iloreta.
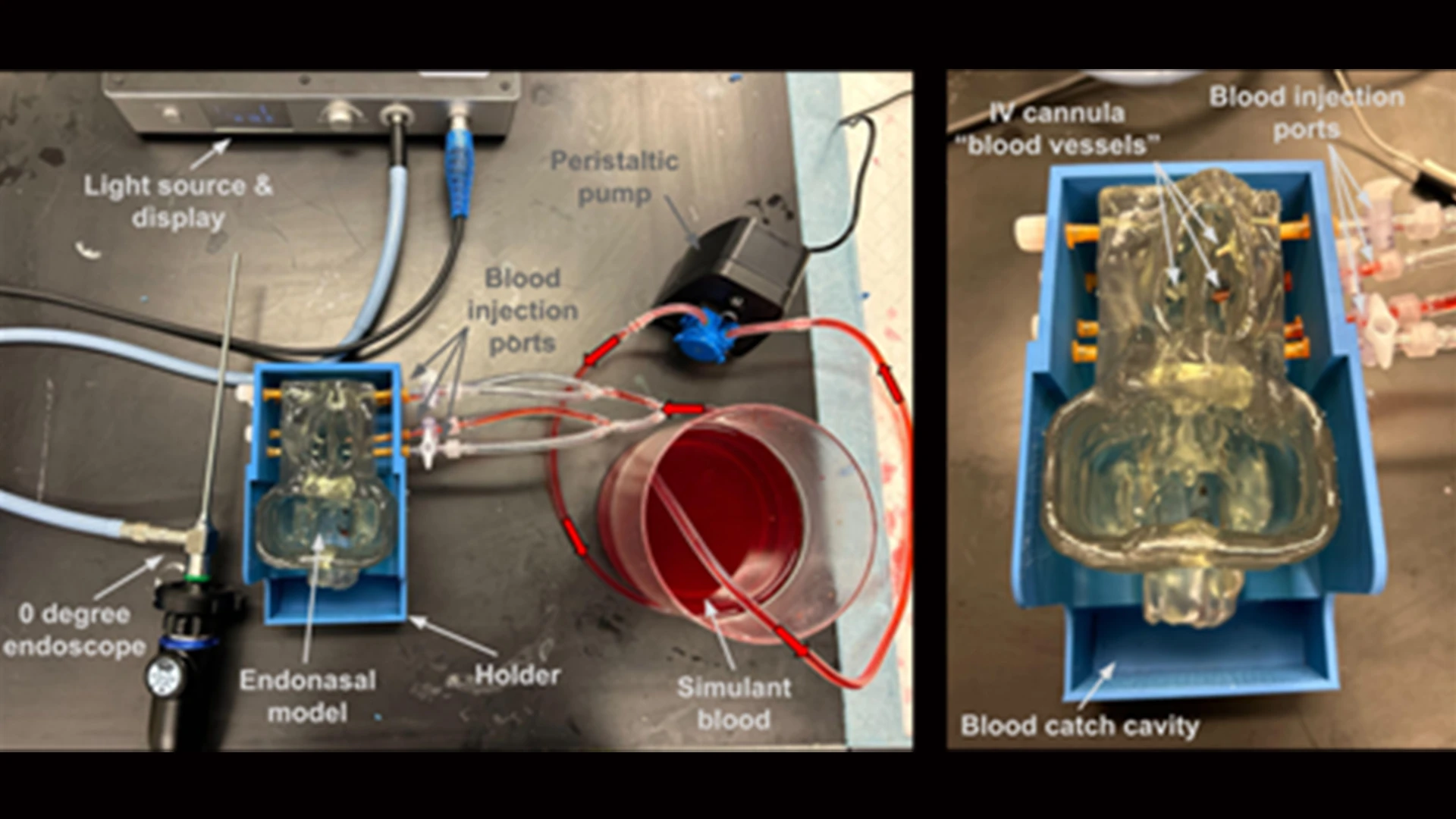
Figure 1. Purpose-built multiformat 3D-printed model used to simulate endoscopic bleeding challenges. The model includes eight anatomically relevant injection ports, each with a peristaltic pump that injects a blood surrogate at a variable infusion rate. Surgeons can use a variety of methods, from hemostatic clips, bipolar cautery, and mechanical tamponade to stop bleeding.
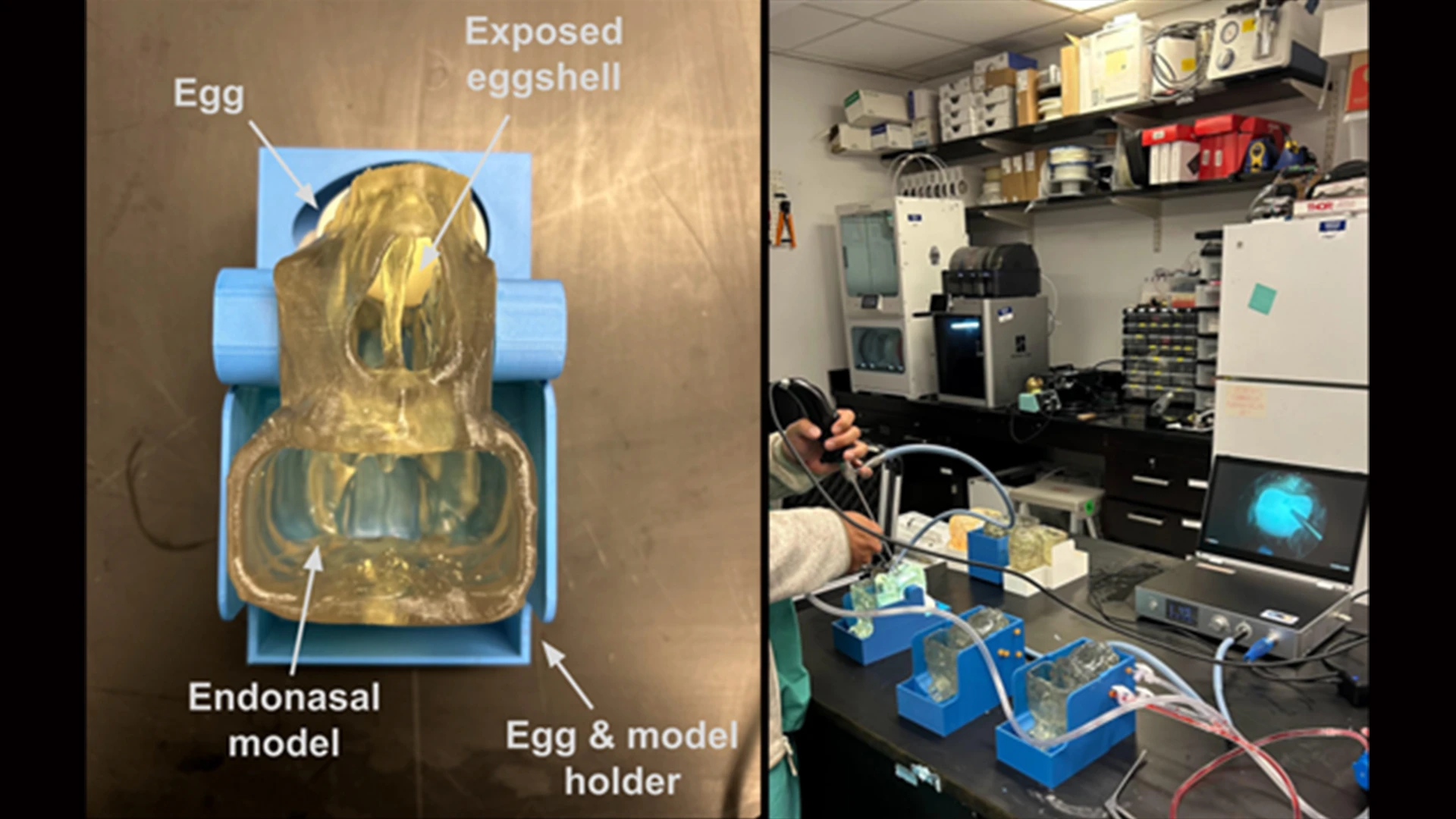
Figure 2. Endoscopic Skull Base Simulation model. This model fuses a 3D-printed human endoscopic model with the natural tissue properties of a raw chicken egg to simulate the experience of performing endoscopic osteotomies and durotomies. The tissue interface between the calcium eggshell and the yolk membrane replicates the surgical experience with high fidelity.
The company has since raised an initial seed round and is advancing development of its first device, a sterile, single-use cuffed surgical catheter that provides continuous evacuation of blood, smoke, and debris from a patient’s nasal passages and airway. In addition, the device has the ability to irrigate the surgical cavity to provide continuous cleaning of the cavity. A first-of-its-kind intrapharynx aspiration catheter, the Pharyvac replaces throat packs and suction tubes with a single, user-friendly device that reduces visual interference during surgery and the risk of aspiration and accumulation of blood in the stomach. The device was undergoing human trials at the end of 2025 in France and is expected to be ready for clinical use in 2026.
The success of Pharyvac reflects a broader culture at Mount Sinai, where departments such as Otolaryngology and Neurosurgery are at the forefront of reimagining surgery through technology. By driving innovation directly from the operating room, these teams are shaping the future of patient care; developing tools and techniques that make surgery safer, more effective, and more precise. Dr. Iloreta’s ability to actively participate in Pharyvac Surgical Technologies while maintaining a busy surgical practice is one example of how clinician-innovators at Mount Sinai are helping define the next era of surgical medicine.
“This innovation model takes advantage of the massive network of experience within the Department of Otolaryngology, the technical expertise of Mount Sinai BioDesign, and the efficiency and speed of a biotech startup,” says Dr. Iloreta. “We can develop ideas, solve problems, and create solutions in real time. The immediacy with which we can function at a high level creates a positive feedback loop. Successful projects generate greater engagement, encourage bolder ideas, and demonstrate that high-performing, collaborative teams can quickly improve patient care.”
That spirit will continue to shape the future. The Department of Otolaryngology, led by Eric Genden, MD, MHCA, FACS, Isidore Friesner Professor and Chair of Otolaryngology – Head and Neck Surgery at the Icahn School of Medicine, is now joining forces with Mount Sinai BioDesign in a more formal collaboration, dedicating engineering and project management support to identify the next wave of breakthroughs in ENT.
“We’ve only just begun,” says Dr. Genden. “This is proof of what can happen when surgeons are empowered to innovate. I’m excited to continue supporting this work. Our department has a vast network within and beyond the institution—surgeons, scientists, industry partners, entrepreneurs. The innovation engine will only grow stronger, and I have no doubt we’ll see many more breakthroughs coming out of our department in the years ahead.”
For Mount Sinai, and for the surgeons and patients they serve, it signals the arrival of a new model for medical innovation, one forged at the intersection of necessity, collaboration, and vision.
Featured

Alfred-Marc Iloreta Jr., MD
Assistant Professor, Otolaryngology - Head and Neck Surgery, and Neurosurgery, Artificial Intelligence and Human Health
Eric M. Genden, MD, MHA, FACS
Professor and Chair of Otolaryngology – Head and Neck Surgery
