Patients who undergo mandibulectomy have long faced the debilitating psychosocial impact of leaving the operating room without teeth. Mount Sinai’s Department of Otolaryngology–Head and Neck Surgery has found a way to not only achieve the immediate restoration of their smiles post-surgery, but also accelerate the timeline to implantation of permanent teeth.
The Department has developed an all-in approach to tumor resection and reconstruction that includes same-day implantation of temporary teeth. This approach is the culmination of years of pioneering work both in the surgical treatment of patients, such as the use of implants and fibula free flaps to create a new jaw, and in the development of sophisticated computer-assisted planning software.
“Using this technology, we are able to conduct patient scans and not only proceed with the fabrication of a customized prosthetic, but also create very precise cutting guides and predictive holes so we can place that prosthetic at the end of surgery,” says Daniel Buchbinder, MD, DMD, Chief, Division of Oral and Maxillofacial Surgery and Professor of Oral, Maxillofacial Surgery, and Otolaryngology at the Icahn School of Medicine at Mount Sinai.
Although other centers offer all-in approaches to mandibulectomy, Michael Turner, MD, DDS, Chief of Oral and Maxillofacial Surgery at The Mount Sinai Hospital, believes Mount Sinai’s approach is unique.
“For one, we put together a system where all our experts are under one roof, which results in a cohesive workflow,” he says. “We also have the resources to offer everything from the most basic services, such as printing 3D teeth, to the most complex, such as making titanium or porcelain teeth. That enables us to treat patients from all walks of life, and I am not aware of any other center that has that ability.”

The surgical team, comprising head and neck surgeons, oral and maxillofacial surgeons, and prosthodontists, in the operating room.
Combining the Benefits of a Multidisciplinary Team With Virtual Planning
Treatment begins with a series of same-day patient consultations with a multidisciplinary team that includes a head-neck oncologist, surgical oncologist, reconstructive surgeon, and prosthodontist. Following confirmation of the diagnosis, the team works with Mount Sinai’s BioMedical Engineering and Imaging Institute to conduct computed tomography scans and develop customized virtual models of the patient’s jaw and teeth, as well as an optical scan to facilitate development of the temporary prosthetic.
Once the scans are completed and combined in a stereolithography (STL) file, the multidisciplinary team performs a virtual tumor and jaw resection, along with placement of the fibula free flap. The STL file of the dental implants and superstructures enables the team to control the pitch and roll of the reconstruction to ensure everything aligns precisely with the upper dentition.
“That is the advantage of virtual planning,” Dr. Turner says. “By determining exactly where the implants need to be, we can proceed with the design of the temporary prosthesis and apply it in the operating room.”

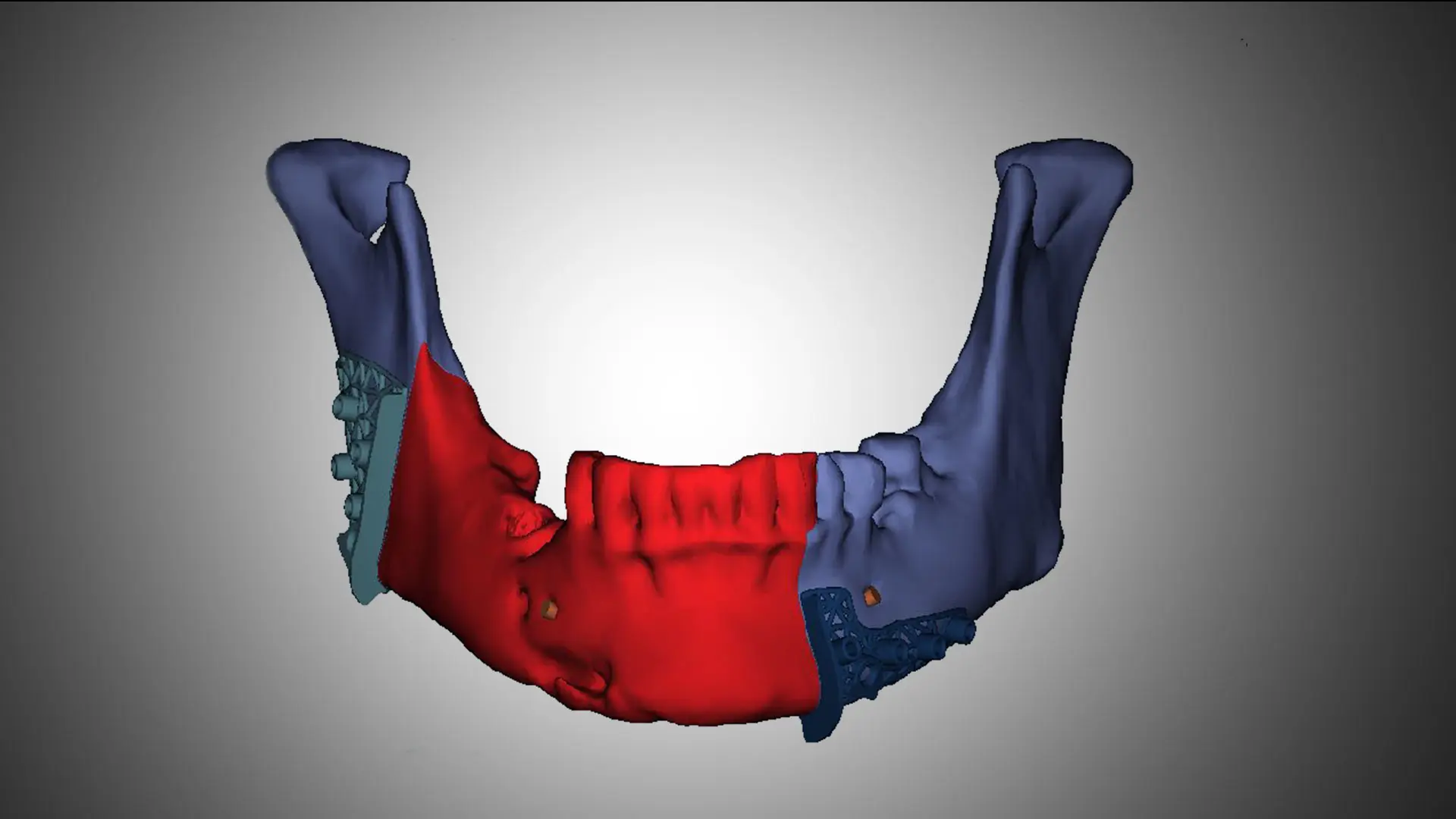
3D CT radiograph of the diseased mandible.
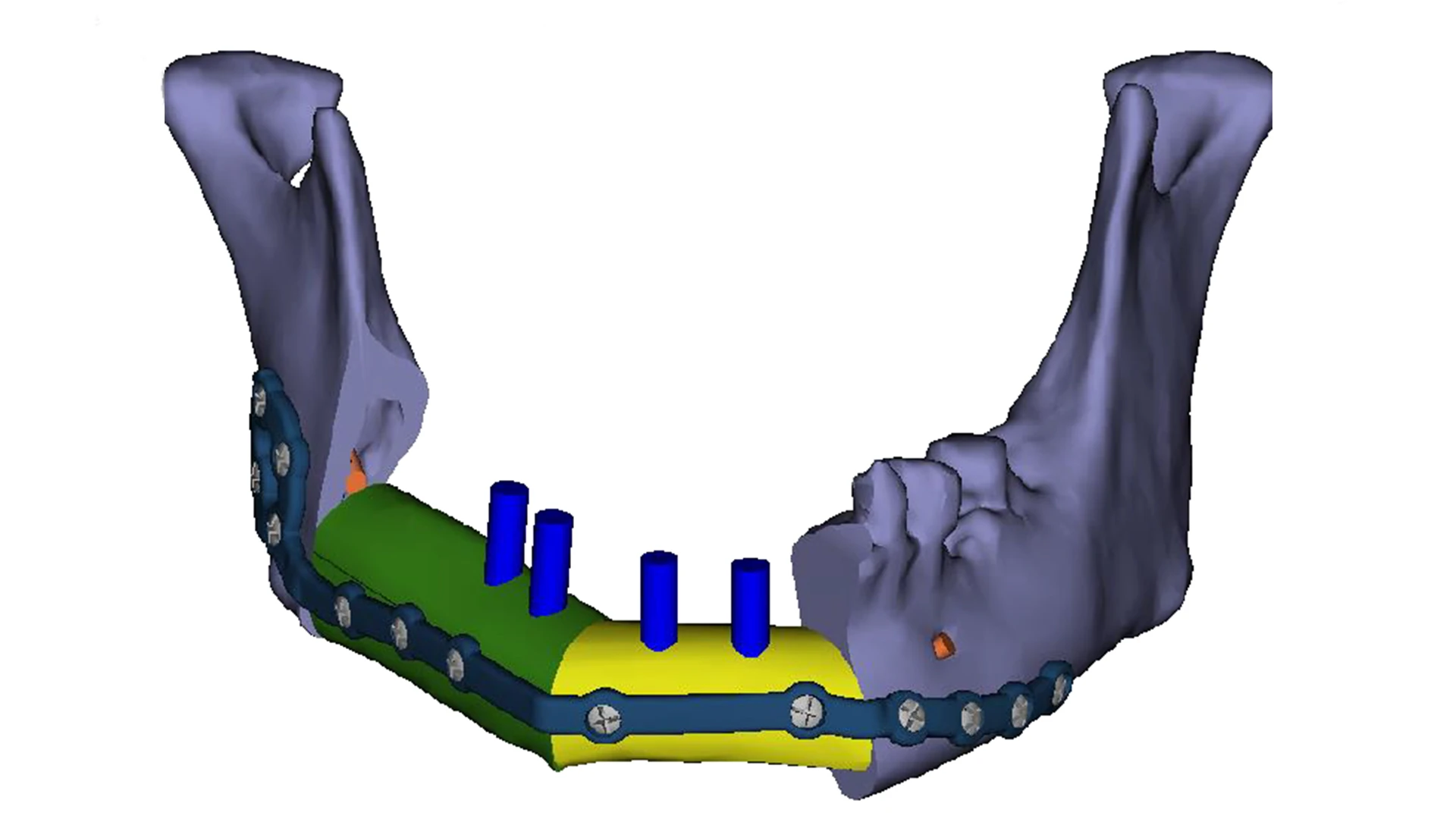
Planned reconstruction of the jaw using a vascularized fibula free flap (green and yellow) and dental implants (blue).
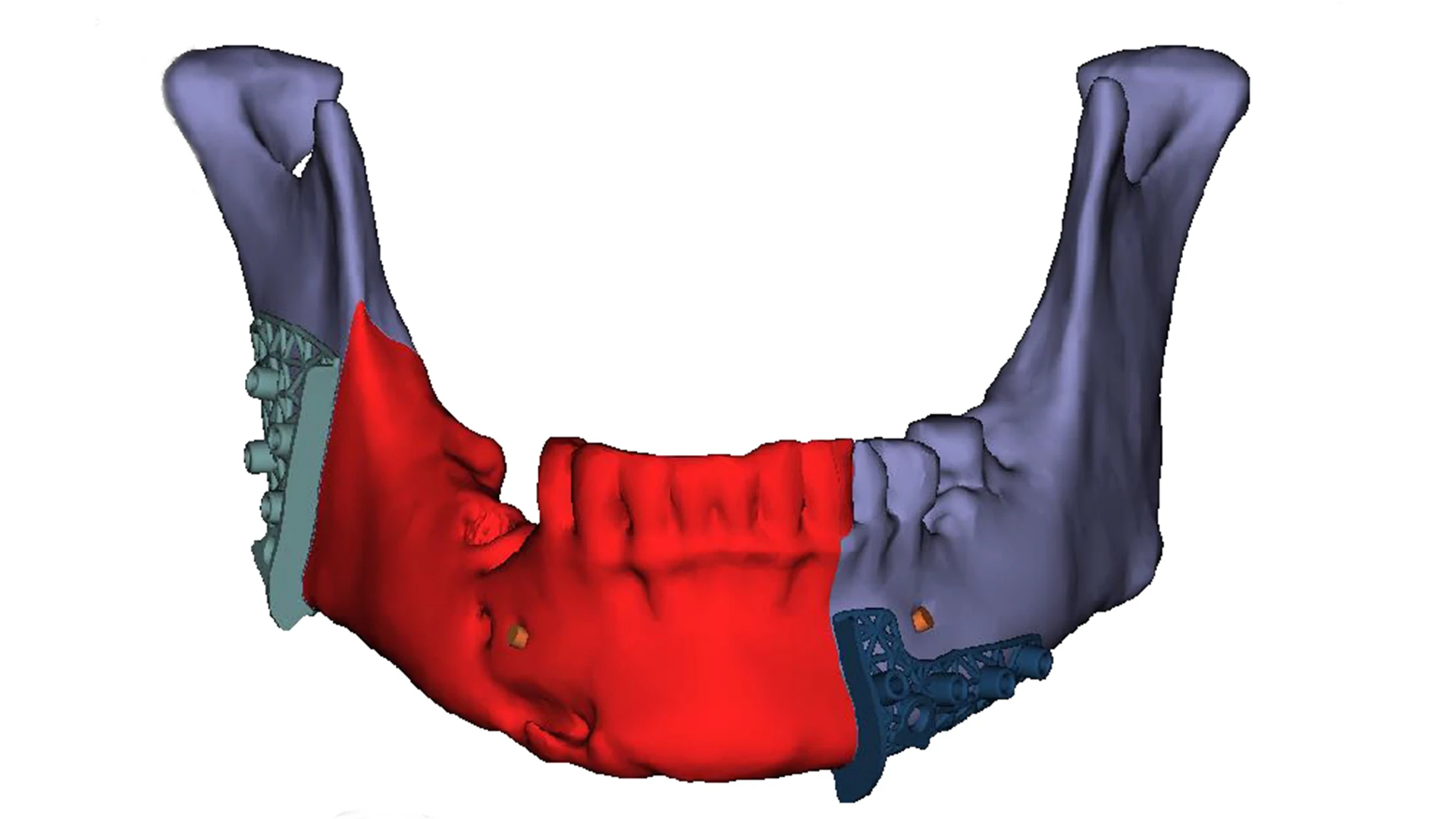
Planned removal of the diseased portion of the mandible (red).

The plan for the teeth to be created prior to the surgery.
Reducing Wait Times for Permanent Prosthesis
The team also develops the cutting guides and predictive holes that will facilitate the all-in surgical procedure, which typically takes between six to eight hours to complete. The priorities for Drs. Buchbinder and Turner during the procedure are to achieve complete resection of the tumor, survival of the bone flap, and infraocclusion placement of the temporary prosthesis. Although the functionality of the temporary prosthesis is relatively limited, Dr. Buchbinder says it serves two important purposes: it contributes to the patient’s psychosocial well-being, and it helps prevent scarring and deformity, facilitating implantation of the permanent prosthesis.
“The process used to take approximately 18 months, but now we are able to make and apply the permanent prosthesis at four to six months, which is done in office by the prosthodontist,” Dr. Buchbinder says.

Patient two weeks after surgery.
Having successfully completed 10 all-in procedures as proof of concept, Drs. Buchbinder and Turner are now looking at ways to make the procedure more precise and seamless. They are interested in working with the manufacturers of 3D bone plates, cutting guides, and dental implants to achieve those goals.
“Better implants mean better distribution of the biting forces, resulting in improved and quicker function for patients,” Dr. Turner says. “At the same time, the more precise we are, the better the outcomes. I believe we have the resources to take this to the next level and, with the resources we have at Mount Sinai, we will.”
Featured

Daniel Buchbinder, MD, DMD
Chief, Division of Oral and Maxillofacial Surgery and Professor of Oral, Maxillofacial Surgery, and Otolaryngology

Michael Turner, MD, DDS
Chief of Oral and Maxillofacial Surgery