For years, Mount Sinai’s Mark Urken, MD, conducted intraoperative frozen section analysis of surgical margins for head and neck cancer specimens by leaving the operating room to confer with his colleagues in pathology. It was a process he found time consuming and inadequate, given that there was no way to accurately document the precise geographic location as well as the breadth of the supplemental margins that were taken, and, most importantly, the extent to which they accurately covered the areas of risk on the defect.
“Not only are the pathologists unaware of what is actually being done in the operating room, but they are also creating hand-drawn diagrams in an attempt to visually demonstrate the location of the samples, which can be misinterpreted and lacking in precision,” says Dr. Urken, Professor of Otolaryngology−Head and Neck Surgery at the Icahn School of Medicine at Mount Sinai.
“Moreover, the specimen is typically dissected and drastically physically altered during frozen section sampling,” he adds, “so it is no longer recognizable, and you do not have an enduring rendering of it for downstream care providers to further their understanding.”
Combining 3D Modeling and Teleconferencing Technology for Frozen Section Analysis
Dr. Urken, with his colleague Margaret S. Brandwein-Weber, MD, Professor of Pathology, Icahn Mount Sinai, and Chair of Pathology, Mount Sinai West and Mount Sinai Beth Israel, believe they have created a better approach. Using three-dimensional (3D) modeling technology, Drs. Urken and Brandwein-Weber have developed a workflow that has the potential to become the gold standard process for conducting frozen section analysis and communicating margin results. In this process, the patient’s specimen is removed and taken by a member of the surgical team to the pathology lab for examination and orientation. The intact specimen is scanned, and a virtual 3D model is generated and refined by a technician while the pathologist conducts inking, mapping, sampling, grossing, and microscopic analysis of the specimen. Although the actual specimen is essentially destroyed by the removal of innumerable samples for pathologic analysis, the 3D scan provides a precise and enduring replica of what was removed.
Once the status of the surgical margins is finalized, the pathologist uses Microsoft Paint 3D to annotate the 3D specimen model, indicating the locations of the sampled sections. The pathologist then uses Zoom, a popular video conferencing platform, to project this annotated specimen model onto operating room monitors for surgeons to visualize what was found in the frozen section lab. This 3D optical imaging-driven workflow, combined with teleconferencing technology, allows the pathologist and surgeon to look at the model together, remotely, while the surgeon remains scrubbed in the operating room, to discuss sites that may require additional supplemental resections.
Following the resection of the cancer, a second 3D scan of the defect in the patient is created. The surgeon then annotates the 3D image to show where supplemental margins were harvested, as well as the breadth of those margins. This bidirectional information flow allows a markedly improved level of communication and documentation of what was found in the pathology lab, as well as what was actually performed in the operating room. The report on 3D scanning of surgical defects, “Intraoperative three-dimensional scanning of head and neck surgical defects: Enhanced communication and documentation of harvested supplemental margins,” was published in Head & Neck in August 2023.
“This eliminates the need for the surgeon to unscrub and walk over to the pathology lab,” Dr. Urken says. “This approach has really transformed the conversation that occurs between the pathologist and the surgeon. Not only is it more efficient, but there is also a level of precision in information that heretofore could not have been achieved.”
Additionally, by using the teleconferencing platform, all members of the surgical and nursing teams are able to visually understand what was found and how it influences the course of the surgery. A time-out is called in the operating room to review the findings and reach consensus between the surgeon and the pathologist to ensure the goals of the oncologic resection have been accomplished. The introduction of a pathology time-out into the surgical workflow was published in an article titled “Frozen Section Time-out: Pilot Study to Reconcile Margins Using 3D Resected Specimen and Defect Scans” in The Laryngoscope in July 2023.

Intraoperative transfer of information from the frozen section lab to the operating room.
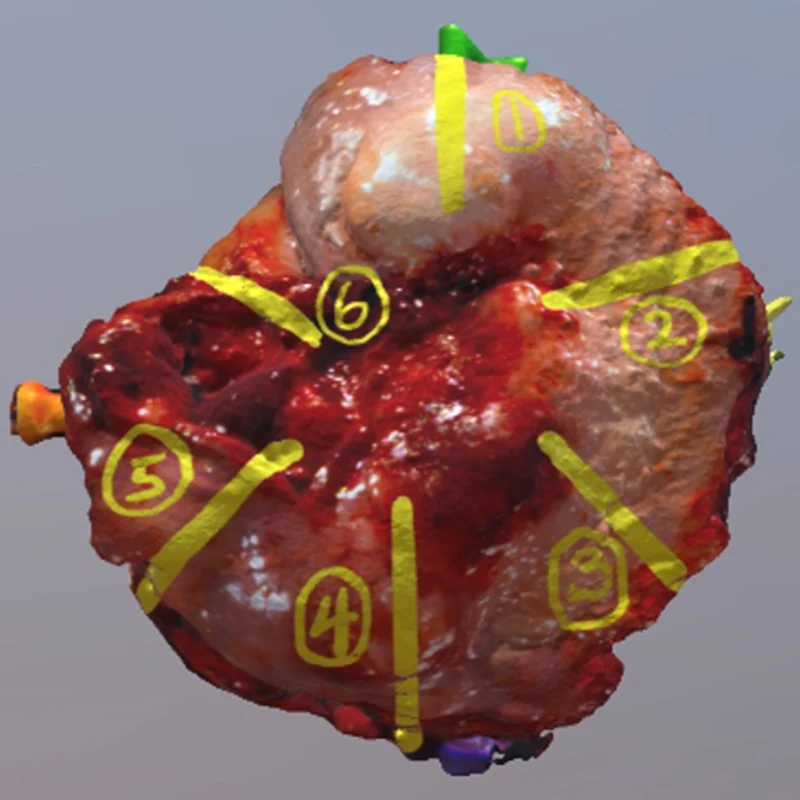
3D image of a scanned partial glossectomy specimen.
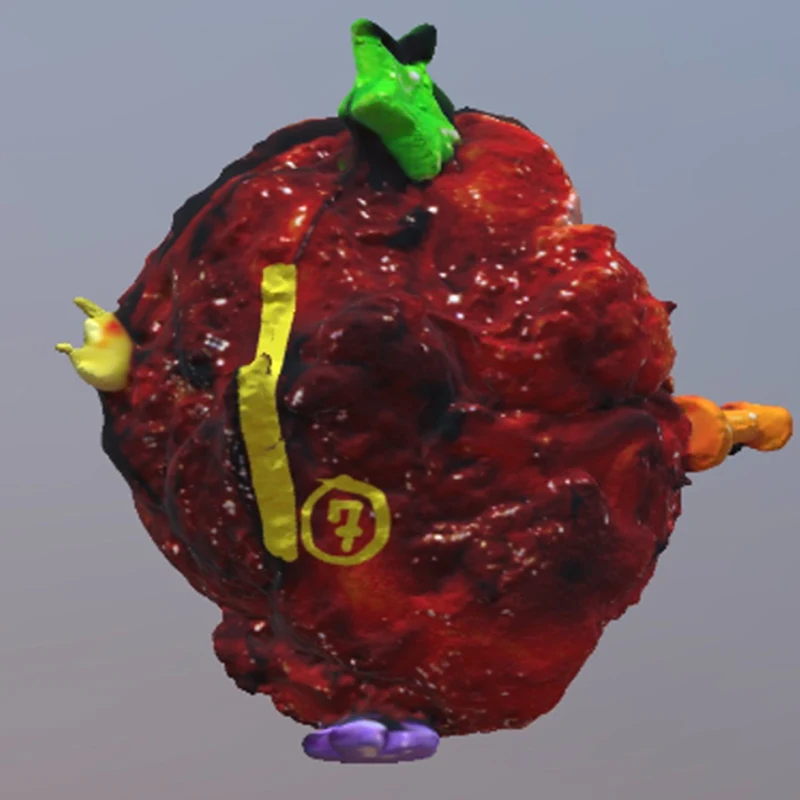
Deep surface of the same specimen with annotated margins indicated.
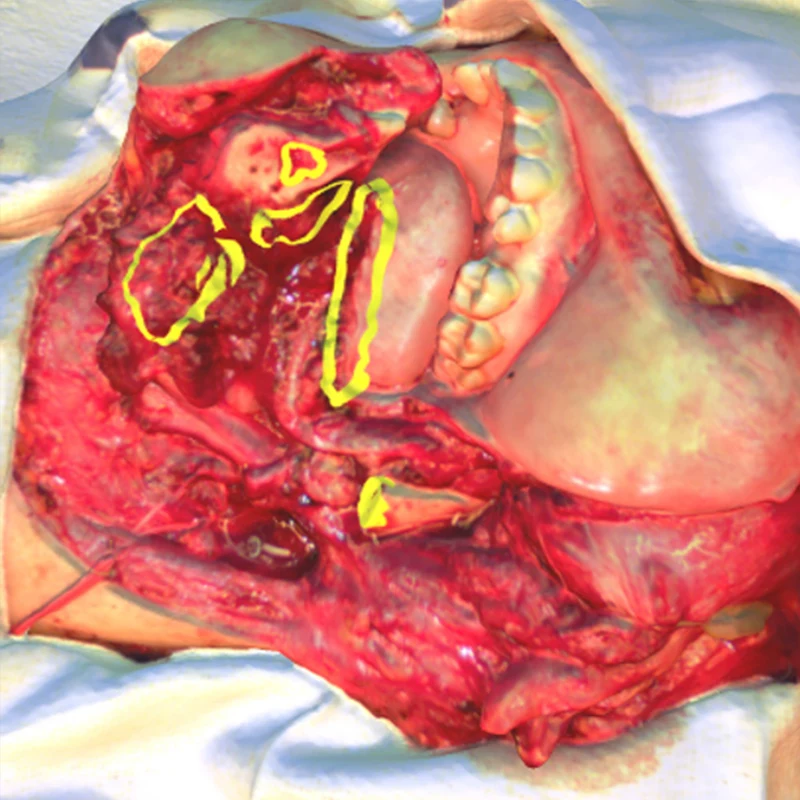
3D scanned image of a defect following a partial mandibulectomy and floor of mouth resection. Annotations indicate the precise location and breadth of supplemental margins harvested.
3D Models Become ‘Durable Parts’ of Patient Records
In a first-of-its-kind study, Dr. Urken demonstrated the efficacy of conducting intraoperative frozen section analysis using his 3D optical imaging-driven workflow. Fifty-five head and neck specimens were scanned, virtually annotated, and displayed in the operating room, providing a real-time specimen-to-defect relationship to guide further resections. He found that the average reporting time for margin results was 34 minutes using the workflow, and that the 3D scanner rendered accurate models of specimens that exceeded 3.0 x 3.0 x 3.0 cm. The results were published in the January 2023 edition of Head & Neck.
“There is a slight increase in the time required to perform these scans,” Dr. Urken says. “But the scans become durable parts of the patient’s record, which is invaluable for downstream providers. For example, radiation oncologists can use this information to make more informed decisions regarding adjuvant radiation therapy, which will be beneficial for patients.”
Drs. Urken and Brandwein-Weber plan to explore the benefits of this workflow further through studies that will analyze its impact on patient outcomes and its potential to reduce risk for cancer recurrence. Regardless, he says the quality assurance aspect is evident. This workflow can readily and inexpensively be adopted by other health care systems to achieve a more efficient and precise process for frozen section analysis.
“The standard approach to intraoperative frozen section analysis has long been stagnant,” Dr. Urken says. “We believe we have broken through a significant barrier and arrived at a place we never could have imagined. There are endless possibilities as to how far we can take this, and we will be exploring that further here at Mount Sinai.”
Featured
Mark Urken, MD
Professor of Otolaryngology-Head and Neck Surgery
