For patients undergoing medialization laryngoplasty to address a paralyzed vocal cord, precision is required to regain normal voicing. Specifically, this entails testing and carving an implant, followed by repeated attempts at this until it occurs. This technique is more akin to an art and requires specific experience and training.
Diana N. Kirke, MD, believes she can shorten the operation and make it easier to perform. She is leading a team of Mount Sinai researchers in a first-of-its-kind study to investigate the potential of three-dimensional (3D) modeling of the paraglottic space to facilitate surgical treatment among patients who present with paralyzed vocal cords.
“There are some centers that are analyzing the paraglottic space, but no one is building the models like this,” says Dr. Kirke, Assistant Professor of Otolaryngology—Head and Neck Surgery at the Icahn School of Medicine at Mount Sinai. “Our goal is to use these models to assess whether volume differences are appreciable in paralyzed versus innervated hemi-larynges. This will create a basis for future work that achieves improvements in patient outcomes, surgical efficiency, and cost efficiency.”
Phase One: Creating 3D Models of the Paraglottic Space From CT Scans
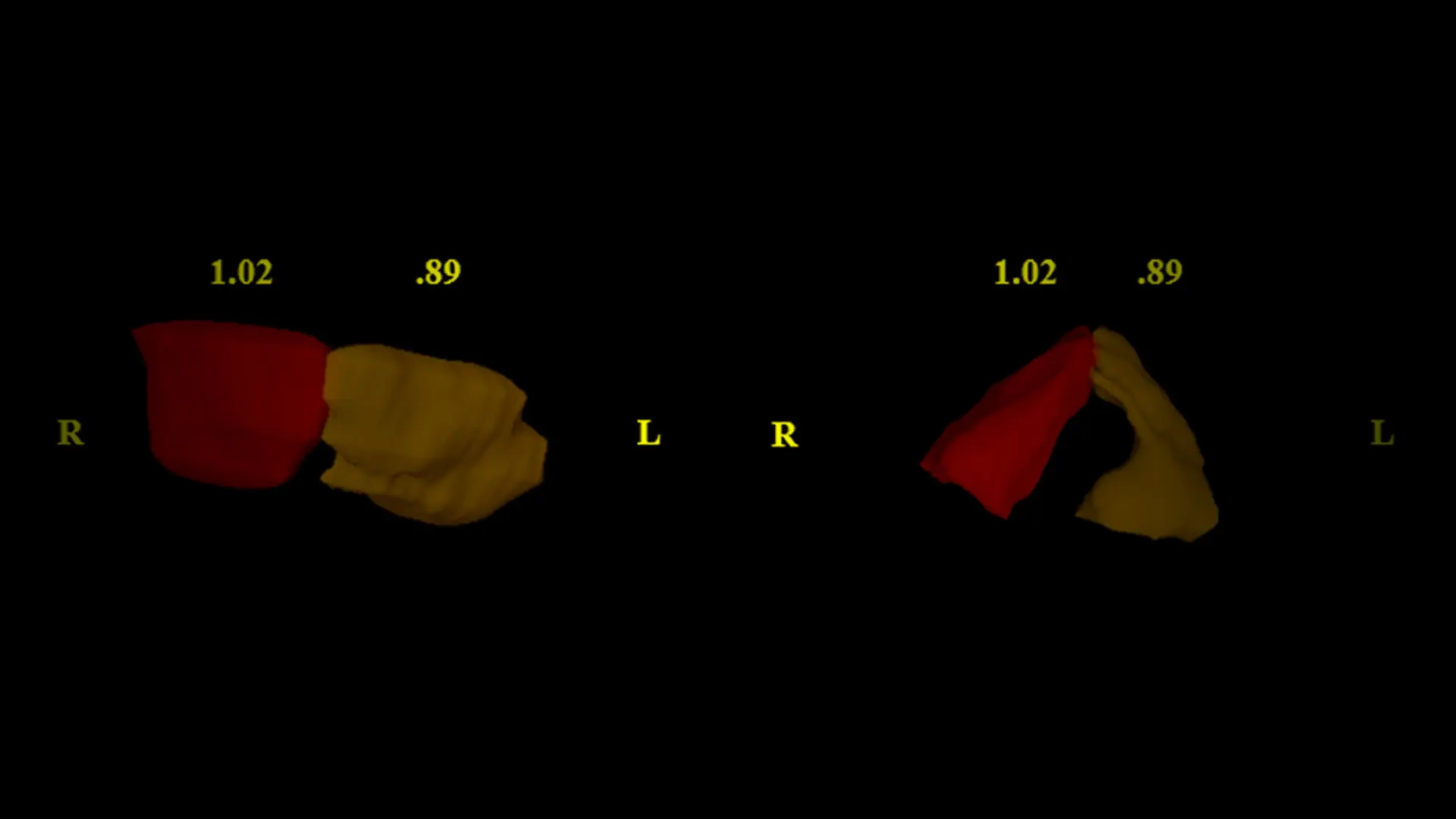
In the first phase of the study, Dr. Kirke and her colleagues conducted a retrospective chart review of 13 adult patients who presented with unilateral vocal fold paralysis but had no history of laryngeal framework surgery or head or neck radiation. Using software from Brainlab, a company that makes digital medical technology, the researchers created 3D models of the paraglottic space from computer tomography (CT) scans. The team was able to measure the volumes of the paraglottic space using these scans. They also observed a smaller space on the paralyzed side in 11 of the 13 scans, with a mean volume difference of 0.18 cm^3 (P=0.0002) (see Figure 1). Two of the scans demonstrated glottic height asymmetry, with the paralyzed vocal fold lower than the non-paralyzed fold (see Figure 2). Dr. Kirke says this was an important observation, as this mismatch clinically results in diplophonia.
Figure 1: Demonstration of volume loss in a patient with left vocal fold paralysis (volumes displayed).
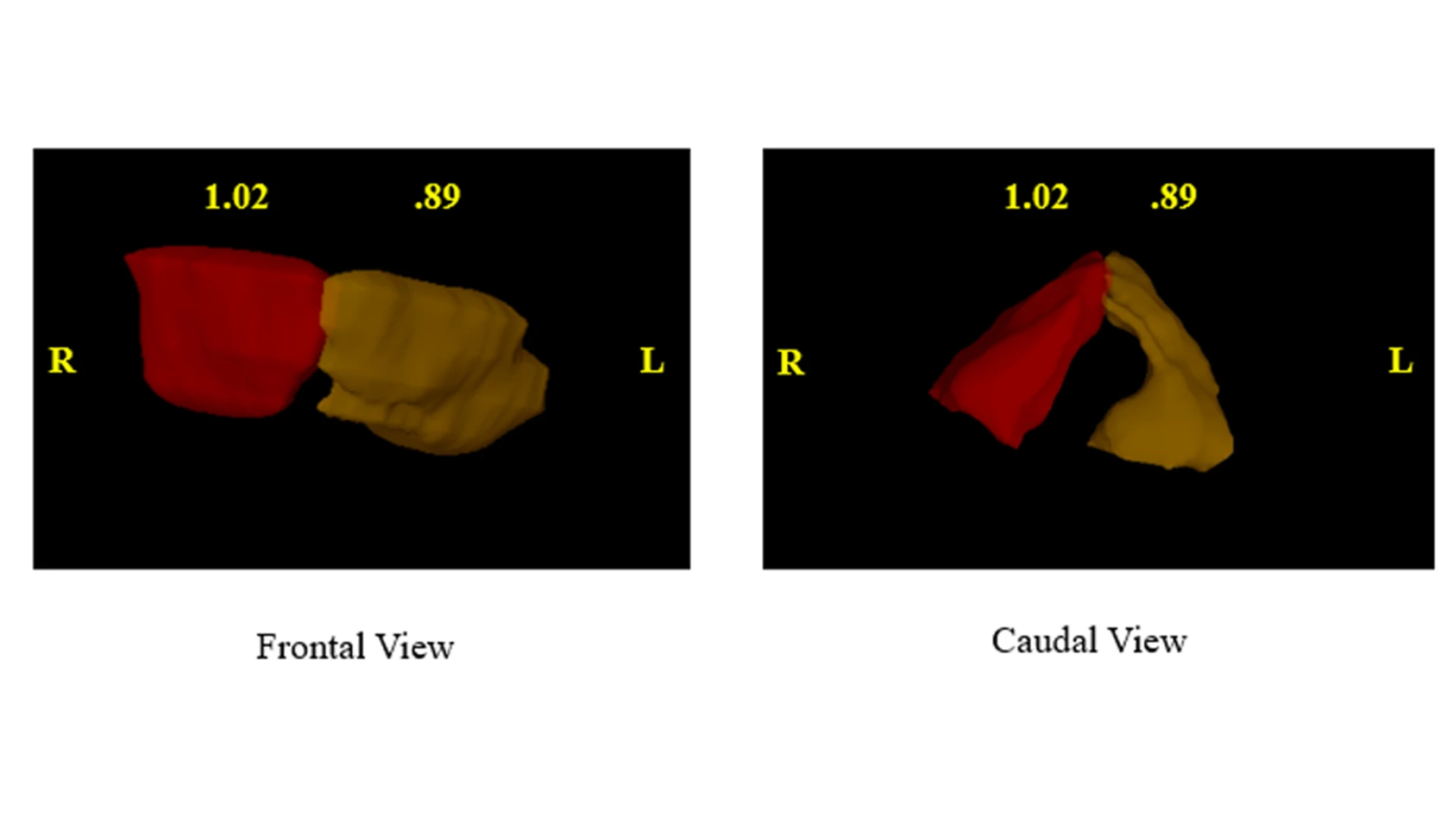
Figure 2: Templates of the paraglottis demonstrating appreciable height difference in two different patients (volumes displayed).
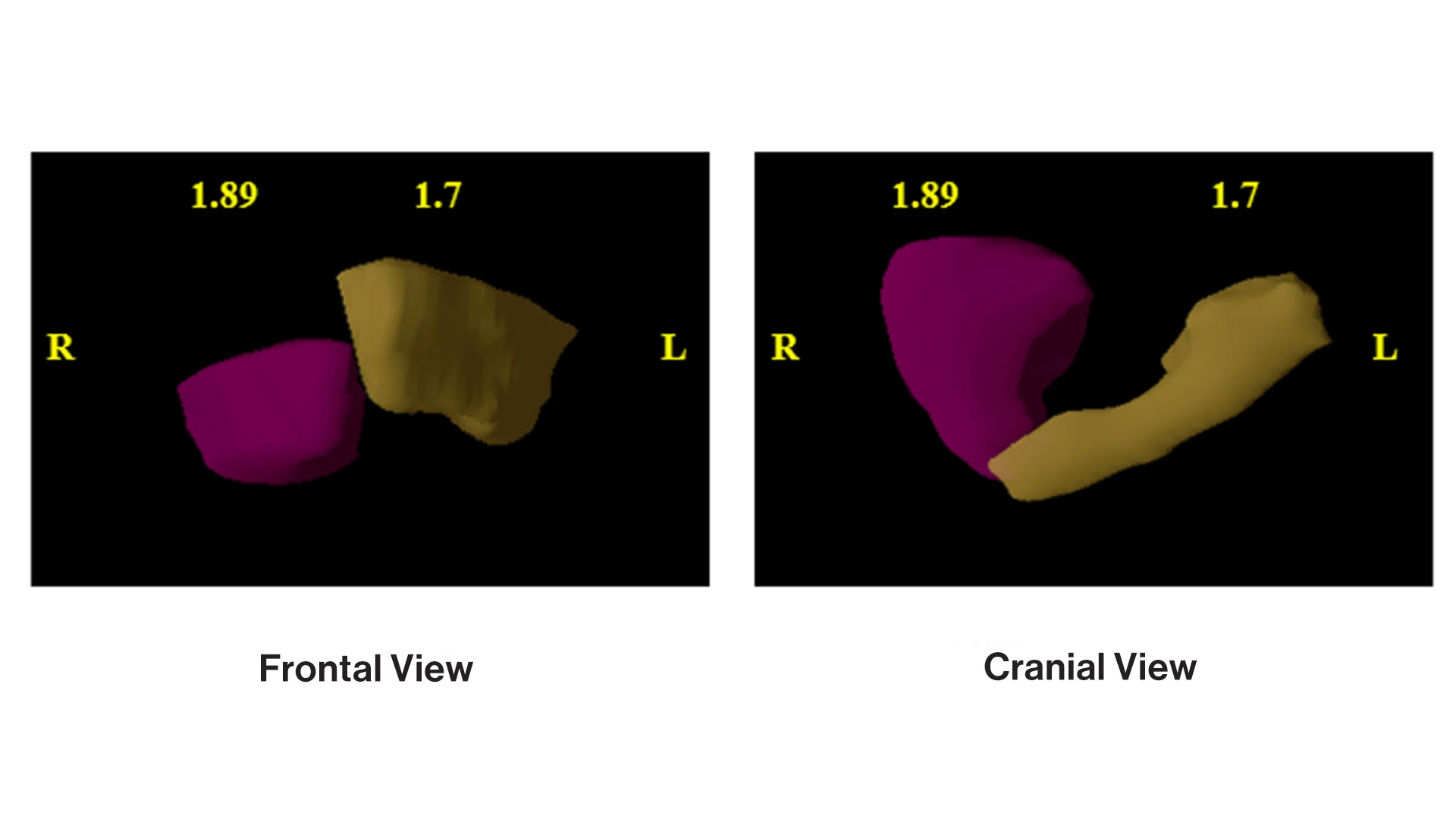
Right paralysis, 5.4 mm height difference.
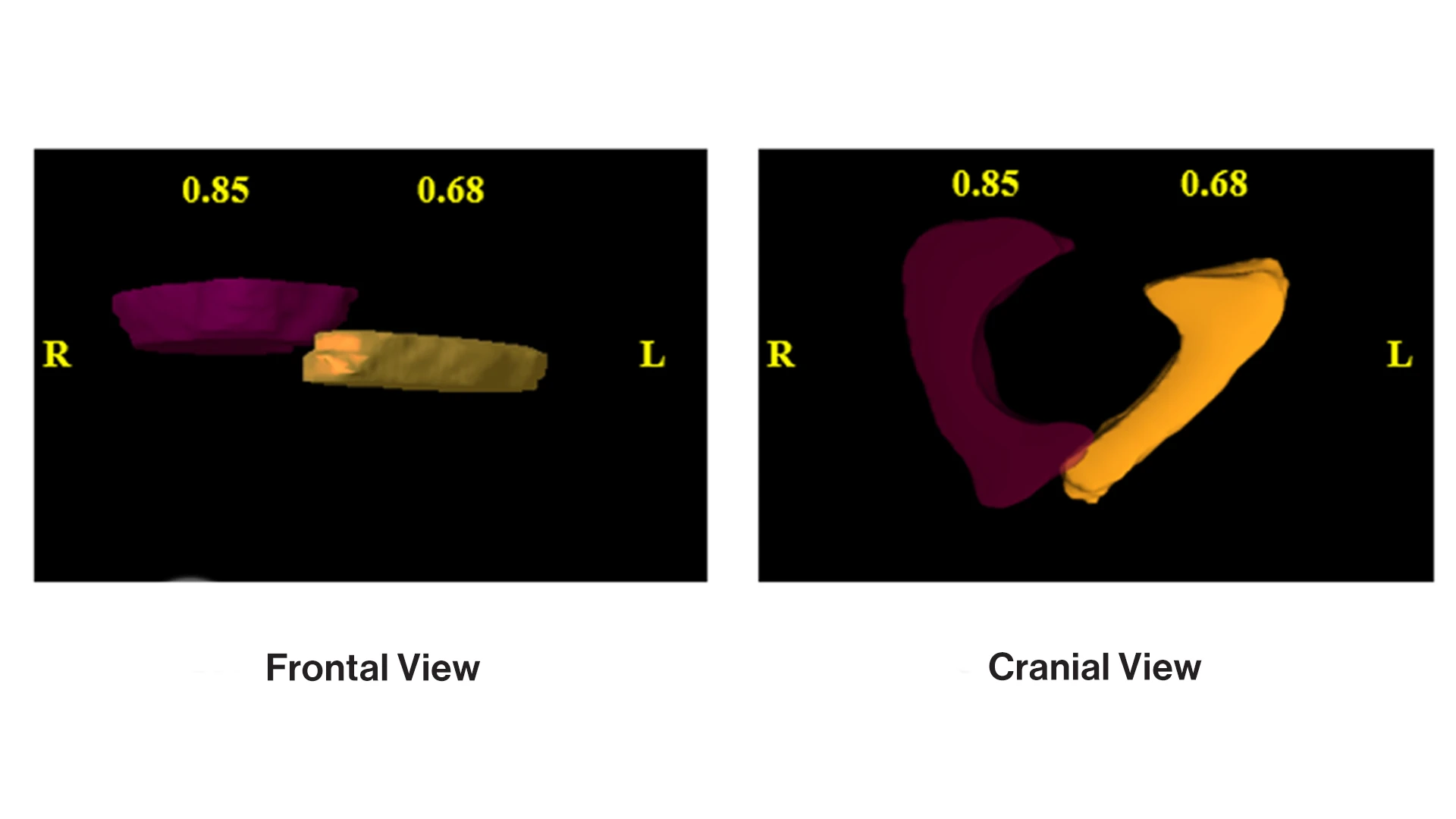
Left paralysis, 2.8 mm height difference.
“We found that 3D modeling of the paraglottic space provides an enhanced understanding of the anatomy of paralyzed vocal folds, in particular, mismatches in height with the non-paralyzed vocal fold as well as potentially the degree of volume that needs to be replaced in a type 1 medialization laryngoplasty to achieve effective medialization,” she says.
Phase Two: Creating 3D Models of Cadaveric Paraglottic Spaces
In the second phase of the study currently ongoing, the research team is scanning and building 3D models of cadaveric paraglottic spaces, which will be implanted on five cadaveric larynges. Once implanted, Dr. Kirke will conduct a two-tailed t-test to compare pre- and post-implantation volumes. If she is able to achieve a strong volume augmentation and complete the implants efficiently, she envisions a third phase involving human implantation trials. This will involve implantation of the 3D template to assess fit, record the voice, and take photos of the larynx. The template will then be removed, and the process will be completed with the gold standard implant to enable a comparative analysis based on procedure time and quality of voice.
If the results are favorable, Dr. Kirke says 3D paraglottic space modeling could significantly enhance type 1 medialization laryngoplasty planning. That could result in a significant reduction in the duration of the procedure from an average of 90 minutes to as little as 30 minutes. “That would mean reduced swelling, postoperative pain, and recovery time,” she says. “More importantly, it could enable us to improve time to voicing and achieve better voicing for our patients. That is our main goal.”
Featured

Diana Kirke, MD
Assistant Professor of Otolaryngology—Head and Neck Surgery