The first time that Alfred M.C. Iloreta Jr., MD, administered 5-aminolevulinic acid (5-ALA) to resect a squamous cell carcinoma in September 2021, he was not sure what to expect. Would it fluoresce once the lights went out in the surgical theater, providing a clear topography of the tumor to facilitate its removal, or would he have to rely on his expertise and conventional imaging equipment to proceed?
“The tumor was literally glowing within the surgical cavity,” recalls Dr. Iloreta, Assistant Professor of Otolaryngology and Neurosurgery at the Icahn School of Medicine at Mount Sinai. “It gave an immersive, multidimensional image of what was cancer and what was normal tissue. I think everyone who was there was excited because we could see the future of cancer surgery glowing right before our eyes.”



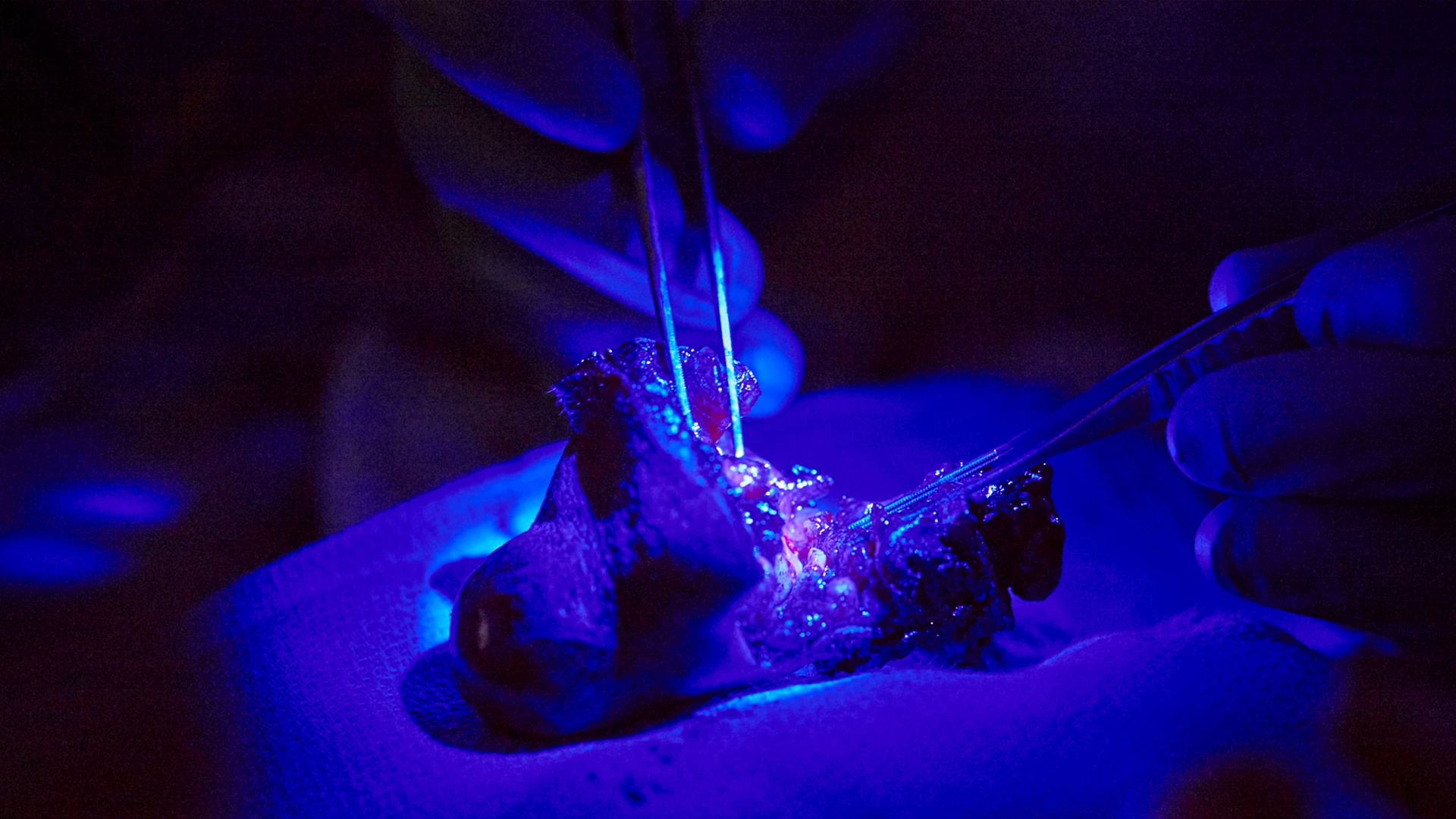
A naturally occurring substance that many use as an antioxidant, 5-ALA will concentrate and convert into a porphyrin when administered at a high dose, causing it to glow when exposed to specific wavelengths of light. Currently, the substance is only indicated for use among patients undergoing glioblastoma surgery by the U.S. Food and Drug Administration; however surgeons are increasingly adopting it for other applications. Dr. Iloreta is one of the first to explore its application among patients who present with head and neck tumors.
Using 5-ALA creates a visible cellular profile of the cancer, which enables the surgeon to be more precise in distinguishing between normal tissue and a tumor. Use of this technology offers a level of precision that gives surgeons insight on the cellular level. This can be more precise than the standard combination of CT and MRI imaging, surgical loops, and microscopes. “Given that the tumors of the head and neck are located in anatomical areas that contain many structures that are vital to quality of life—such as the optic nerve—it is important that we remove as much tumor as possible while preserving as much normal tissue as we can,” Dr. Iloreta says. “Utilizing 5-ALA enhances our ability to do that.”
Dr. Iloreta notes that the inspiration to use the substance came from collaborating with neurosurgeons at Mount Sinai on surgeries involving the resection of intracranial and sinonasal tumors. “Having observed first-hand what my colleagues were able to achieve using tumor fluorescence, we looked into the metabolic and oncologic rationale of why it works for glioblastoma, and we realized it would work for any tumor.”
The first surgery Dr. Iloreta performed using 5-ALA is part of an Institutional Review Board-approved clinical trial he is conducting to assess its feasibility, usability, and safety among patients with squamous cell carcinomas. He is recruiting 25 patients for the study. Each patient will be administered 5-ALA approximately three to six hours prior to surgery, which is performed as normal, but with instrumentation that is capable of fluorescing the tumor. Based on initial success using the procedure in two patients, Dr. Iloreta is already looking to explore the application of 5-ALA in every type of head and neck malignancy.
“We intend to launch clinical trials for those applications to provide meaningful data that show the true impact of the utility of this technique,” he says. “If we find that the predictive value is superior or at least equivalent to the standard of care, which involves sending frozen sections of tumor to pathology for verification, which can be both costly and time consuming, then I can see us using it in both routine cancer cases as well as more complex cases that involve critical structures, such as the carotid artery or the optic nerve, where there is the potential for detrimental impacts for the patient.”
Featured

Alfred-Marc Iloreta Jr., MD
Assistant Professor, Otolaryngology - Head and Neck Surgery, and Neurosurgery, Artificial Intelligence and Human Health
Eric M. Genden, MD, MHA, FACS
Professor and Chair of Otolaryngology – Head and Neck Surgery